doi.org/10.20986/revesppod.2025.1745/2025
ORIGINAL
Relationship between gait parameters and fear of falling in individuals with fibromyalgia
Relación entre los parámetros de la marcha y el miedo a caerse en personas con fibromialgia
Coral Moya-Cuenca1
Sara Zúnica-García1
Hayla Pérez-Matilla1
Ana López-González1
Alba Gracia-Sánchez1
Esther Chicharro-Luna1
1Ciencias del Comportamiento y Salud. Universidad Miguel Hernández de Elche. Alicante, España
Abstract
Introduction: Fibromyalgia is a syndrome characterized by chronic pain, fatigue, and gait and balance impairments, which may contribute to fear of falling. The aim of this study was to analyze the relationship between fear of falling and gait parameters in individuals with fibromyalgia.
Patients and methods: An observational study was conducted in fibromyalgia associations and specialized centers. Sociodemographic, anthropometric, lifestyle, and clinical data related to the disease were collected. Fear of falling was assessed using the Spanish version of the Falls Efficacy Scale-International (FES I), and gait parameters were analyzed using the OptoGait® system.
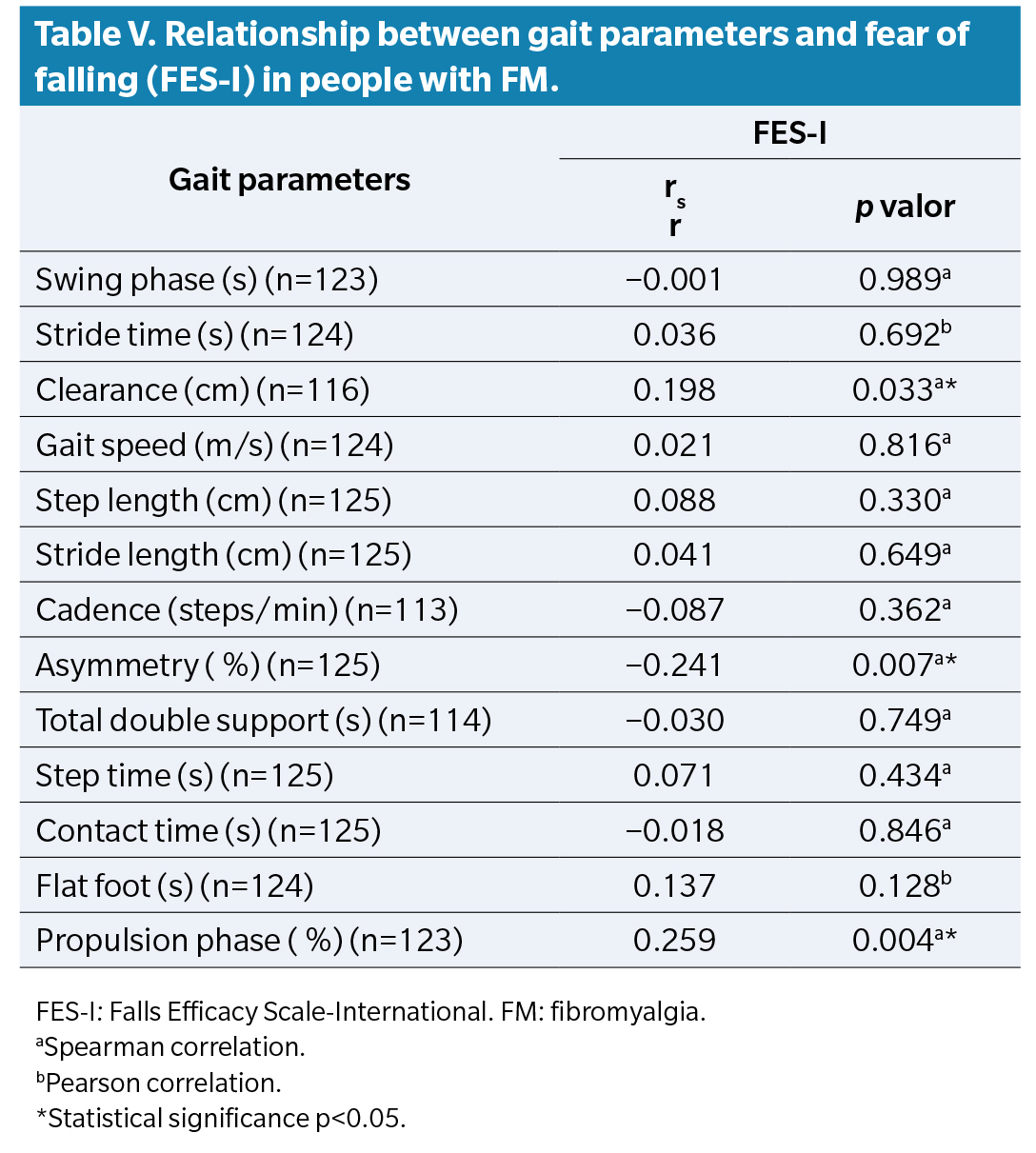
Results: A total of 125 individuals diagnosed with fibromyalgia participated; 95.2 % were women. The mean FES-I score was 37.15 ± 11.57. Higher levels of fear of falling were observed in individuals not engaged in paid work, and those with depression, sleep apnea, or diabetes. In addition, fear of falling was significantly associated with 3 gait parameters: propulsion (r = 0.259; p = 0.004), foot clearance (r = 0.198; p = 0.033), and instability (r = -0.241; p = 0.007).
Conclusion: The results suggest an association between fear of falling and specific gait parameters in individuals with fibromyalgia, highlighting the importance of considering this factor in patient assessment and therapeutic management.
Keywords: Fibromyalgia, fear of falling, gait analysis, gait, Falls Efficacy Scale-International
Resumen
Introducción: La fibromialgia es un síndrome caracterizado por dolor crónico, fatiga y alteraciones en la marcha y el equilibrio, que podrían contribuir al miedo a caerse. El objetivo principal de este estudio fue analizar la relación entre los parámetros de la marcha y el miedo a caerse en personas con fibromialgia.
Pacientes y métodos: Estudio observacional realizado en asociaciones y centros especializados de fibromialgia. Se recogieron datos sociodemográficos, antropométricos, de estilo de vida y variables clínicas relacionadas con la enfermedad. El miedo a caerse se evaluó mediante la versión española del cuestionario Escala Internacional de Eficacia ante Caídas (FES-I), y los parámetros de la marcha se analizaron con el sistema OptoGait®.
Resultados: Participaron 125 personas con diagnóstico de fibromialgia, el 95.2 % eran mujeres. La puntuación media en el FES-I fue de 37.15 ± 11.57. Se observaron niveles más altos de miedo a caerse en personas inactivas laboralmente y en aquellas con depresión, apnea del sueño o diabetes. Además, el miedo a caerse se asoció de forma significativa con 3 parámetros de la marcha: propulsión (r = 0.259; p = 0.004), elevación del pie (r = 0.198; p = 0.033) y desequilibrio (r = -0.241; p = 0.007).
Conclusión: Los resultados sugieren una asociación entre el miedo a caerse y parámetros específicos de la marcha en personas con fibromialgia, lo que subraya la necesidad de futuros estudios para explorar los mecanismos implicados y su impacto en la prevención de caídas.
Palabras claves: Fibromialgia, miedo a caerse, análisis de la marcha, marcha, Escala Internacional de Eficacia ante Caídas
Corresponding author
Sara Zúnica-García
szunica@umh.es
Received: 11-07-2025
Accepted: 08-09-2025
Introduction
Fibromyalgia (FM) is a disease of unknown cause characterized by chronic widespread musculoskeletal pain, accompanied by fatigue, sleep disorders, headaches, and emotional disturbances(1). Its global prevalence is 2.10 %, with higher figures reported in Spain (2.40 %) and in the Valencian Community (3.69 %). It mainly affects women between 40 and 49 years of age, with a female-to-male ratio of 21:1(2).
Although its etiology is not fully understood, it has been linked to alterations in pain perception and stress response, involving neurochemical imbalances in serotonin, substance P, growth hormone, and cortisol, leading to abnormal processing of sensory signals and a reduced pain threshold(1,3). Several risk factors have been identified, including female sex, low educational level, reduced income, and comorbidities such as irritable bowel syndrome, rheumatoid arthritis, migraines, sleep disorders, and psychological disturbances such as anxiety and depression(4).
FM significantly impacts functionality, particularly in the lower limbs, where limitations derived from pain and fatigue promote a sedentary lifestyle and increase the risk of disability(5). Foot involvement is of particular relevance, as it produces pain(6,7,8)and is associated with a marked reduction in quality of life(8). Reported alterations include joint stiffness(7), hallux degeneration(7), painful trigger points(7,9), and peripheral neuropathies(10,11), which not only intensify pain but also may compromise gait and stability.
Gait, as an essential motor function, requires coordination, strength, balance, and reaction time(12).In individuals with FM, disturbances such as slowness, bradykinesia, reduced step length, and balance problems have been observed(5,13). These deficits resemble the gait pattern seen in older adults and may increase the risk of falls. As a consequence, persistent fear of falling may develop, which negatively affects autonomy and quality of life(14).Although both gait impairment and risk of falls in FM have been documented, the direct relationship between objective gait parameters and fear of falling has not been clearly established. Therefore, the main objective of this study was to analyze this relationship in individuals with FM.
Patients and methods
Study design
We conducted a cross-sectional observational study from December 2024 through April 2025 in associations and specialized FM centers in Alicante and Murcia (Spain). The present paper was designed and conducted in accordance with the STROBE guidelines for observational studies(15). The research followed the principles of the Declaration of Helsinki(16,17).
Study population
Subjects were recruited consecutively as they attended the participating centers and met the inclusion and exclusion criteria.
Inclusion criteria: individuals with a clinical diagnosis of FM, aged ≥ 18 years, able to walk at the time of assessment, and who signed informed consent. Exclusion criteria: individuals with cognitive impairment, severe mental disorders, or a recent history (within the last 6 months) of surgery or musculoskeletal injuries in the lower limbs that limited ambulation.
Variable measurement
Data collection was performed by podiatrists with more than 5 years of clinical experience, during an individual consultation with each participant, lasting approximately 15 minutes.
Collected data included sociodemographic variables (sex, age, educational level, marital status, employment status), anthropometric measures (weight, height, body mass index [BMI]), lifestyle habits (tobacco use, physical activity level), and clinical variables related to FM (family history, time since first symptoms, disease duration, age at diagnosis, diagnostic latency, comorbidities, and current treatment).
BMI was calculated as weight/height(2) and classified according to WHO criteria: underweight (<18.5), normal weight (18.5–24.9), overweight (25–29.9), and obesity (≥30) (18). Participants were considered physically active if they engaged in at least 150 minutes of moderate-intensity aerobic activity per week, in line with WHO recommendations. Moderate activity was defined as that which increases heart rate and breathing but still allows conversation, such as brisk walking, light swimming, gentle cycling, social dancing, or household chores requiring effort(19).
Fear of falling was assessed with the validated Spanish version of the Falls Efficacy Scale-International (FES-I) (20), composed of 16 items scored from 1 (not at all concerned) to 4 (very concerned), with a total score ranging from 16 to 64, where higher scores indicate greater concern about falling.
Gait analysis was performed using the OptoGait® system(21), consisting of 2 parallel bars (emitter and receiver) separated by 1.5 m and equipped with 96 infrared sensors. The GAIT TEST protocol was applied, in which participants walked in their usual footwear, at a comfortable and natural pace. They were instructed to start walking before reaching the system, cross the sensorized section, and continue at least 3 steps beyond the bars, to ensure reliable measurement. The total path allowed recording of approximately 50 steps per participant, providing a precise and representative assessment of gait pattern.
Gait parameters evaluated with OptoGait® included: swing phase (s), step time (s), velocity (m/s), foot clearance (cm), step length (cm), stride length (cm), cadence (steps/min), asymmetry between right and left steps ( %), double support time (s), contact phase (s), flat-foot phase (s), and propulsion phase (s).
Sample size
Sample size calculation was performed using software developed by the Clinical Epidemiology and Biostatistics Unit of Complejo Hospitalario Universitario de A Coruña, Universidade da Coruña (Galicia, Spain) (www.fisterra.com). The calculation considered an estimated national prevalence of 2.4 %, a 95 % confidence level, 5 % precision, and an expected proportion of 6 %. Considering Spain’s population of 48,946,035 as of October 1, 2024, according to the National Statistics Institute, a sample of 96 individuals with FM (87 cases + 10 % loss) was required.
Statistical methods
Statistical analysis was performed using IBM SPSS Statistics, version 29 (IBM Corp., Armonk, NY, USA). Qualitative variables were described with frequency distributions (absolute frequencies and percentages), whereas quantitative variables were summarized with means and standard deviations. Normality of distributions was assessed with the Kolmogorov–Smirnov test (for n ≥ 50).
Inferential bivariate analysis was performed. For quantitative variables not normally distributed, the Mann–Whitney U test (for 2-group comparisons) or Kruskal–Wallis test (for >2 groups) was applied. Correlations between quantitative variables were assessed using Pearson’s correlation coefficient (r) when both had normal distribution, or Spearman’s rank correlation coefficient (rs) otherwise. Multiple linear regression was performed using the total FES-I score as the dependent variable. Independent variables included those with clinical relevance and those showing significant association in univariate analysis. Employment status was recoded into 2 categories: employed (1) and not employed (0). Statistical significance was set at p<0.05.
Results
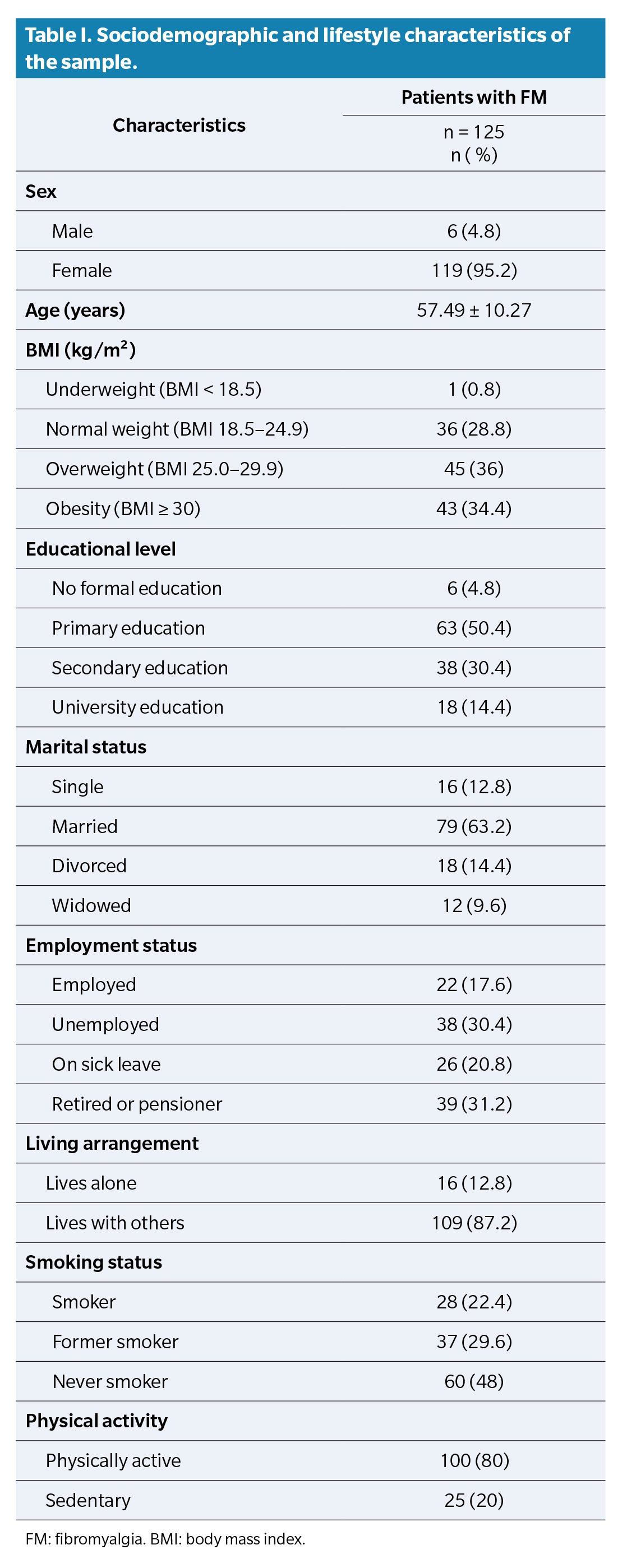
The study included 125 patients diagnosed with FM, of whom 95.2 % were women. Mean BMI was 27.95 ± 5.48 kg/m² (Table 1). Family history of FM was reported by 20.8 % of participants. Regarding clinical course, the mean time since symptom onset was 20.16 ± 12.82 years, while time since diagnosis was 11.88 ± 10.09 years. Diagnostic latency (time between symptom onset and diagnosis) averaged 8.29 ± 8.95 years. Mean age at diagnosis was 45.23 ± 10.04 years. The most frequent comorbidities were anxiety (64.8 %), depression (57.6 %), and hypercholesterolemia (40 %).
In terms of treatment, most patients visited a podiatrist (65.6 %), mainly for chiropody procedures (50.4 %) and plantar orthoses (35.2 %). Additionally, 62.4 % received physical therapy, 52.8 % psychological treatment, and 28 % psychiatric care. A total of 68.8 % were receiving pharmacological pain management, and 76.8 % were taking psychotropic drugs, mainly antidepressants (64.8 %).
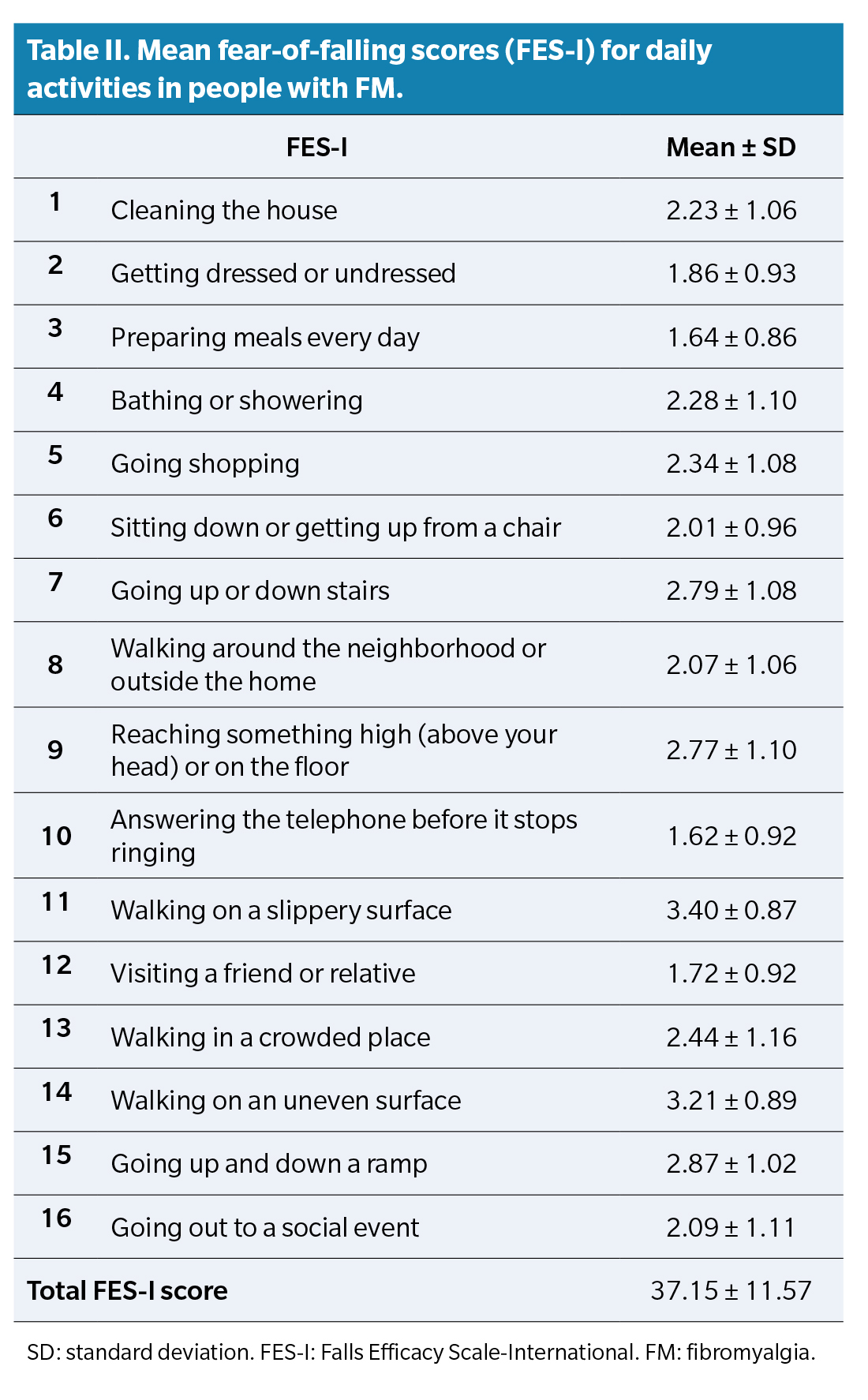
Mean FES-I score was 37.15 ± 11.57 points. The activities generating the greatest concern were walking on slippery surfaces (3.40 ± 0.87), walking on uneven surfaces (3.21 ± 0.89), and going up or down a ramp (2.87 ± 1.02) (Table 2).
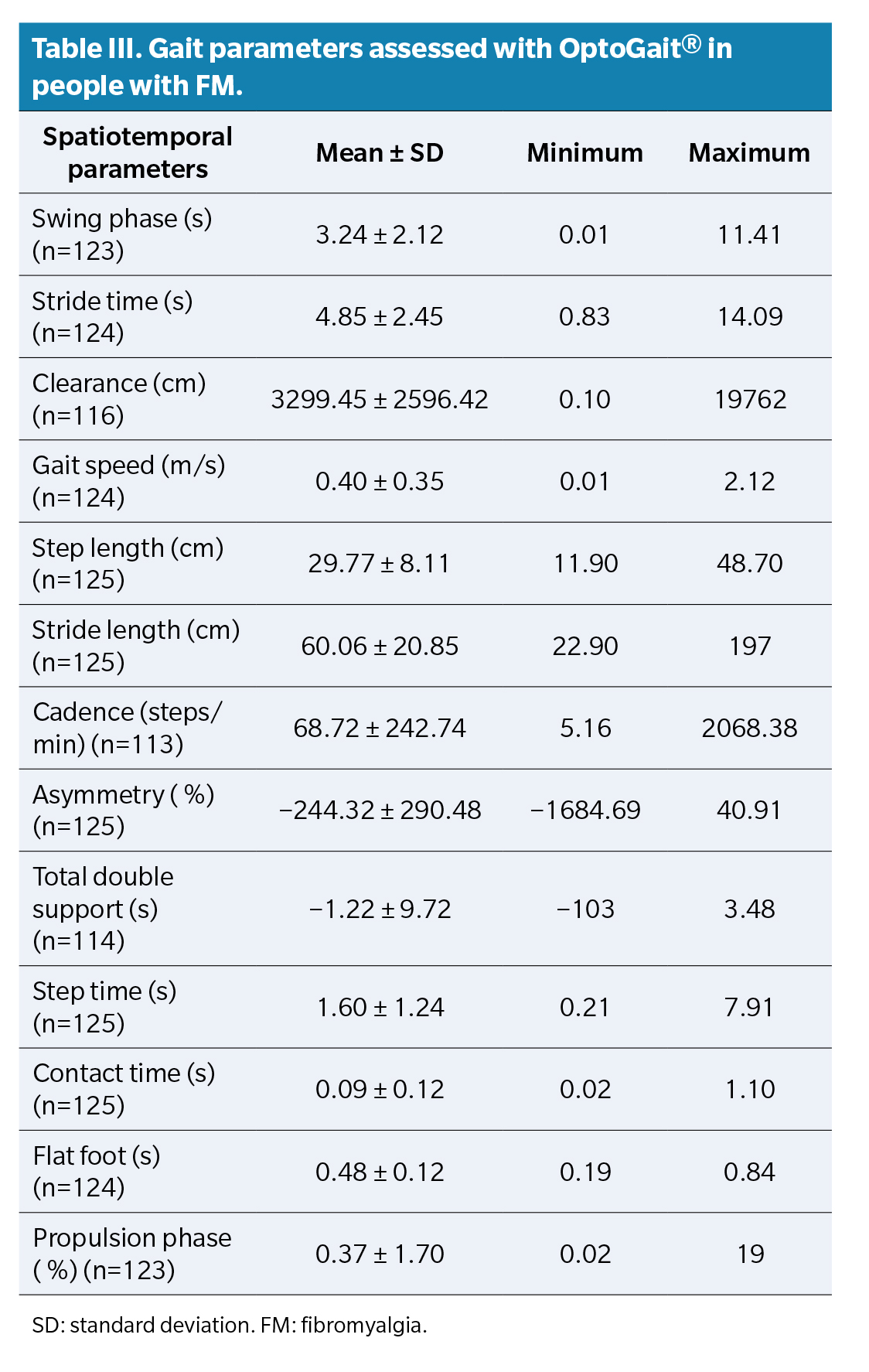
Spatiotemporal gait parameters assessed with the OptoGait® system are presented in detail in Table 3.
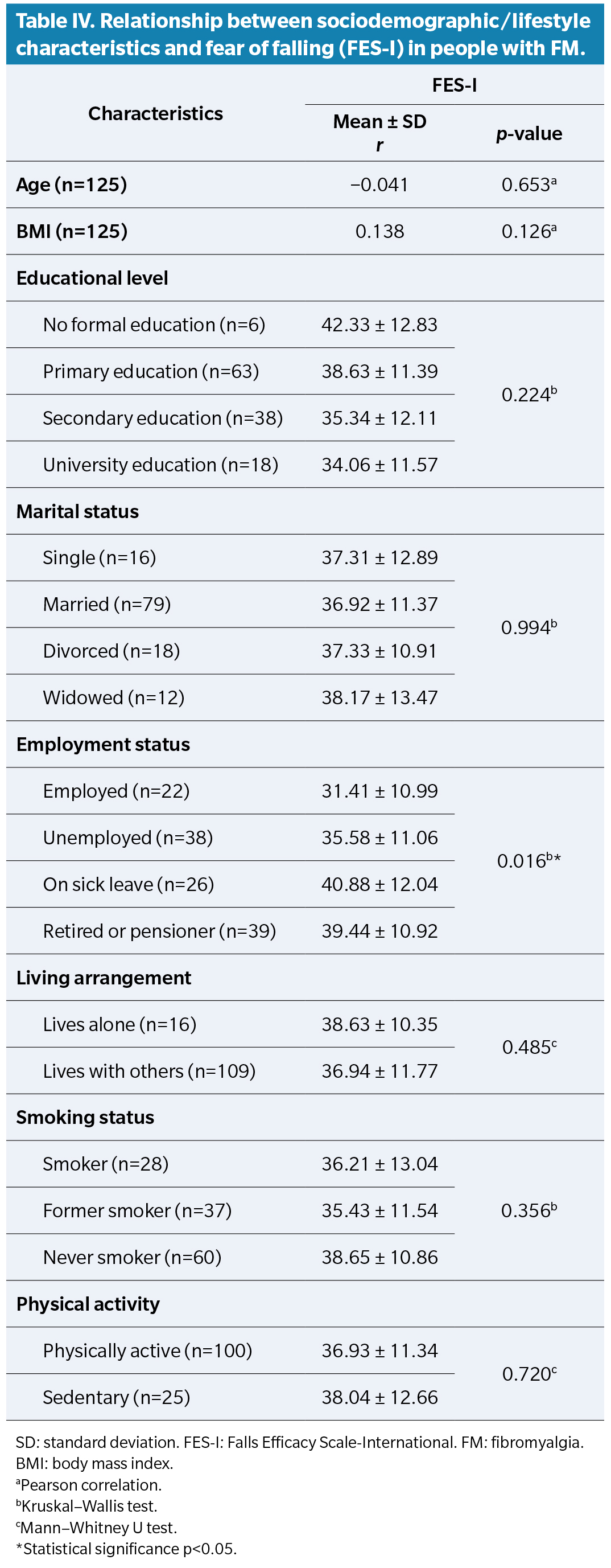
Significant differences were found in FES-I score according to employment status, with higher scores in unemployed or retired individuals compared to those employed (p = 0.016) (Table 4). No significant correlations were found between fear of falling and years since symptom onset (r = −0.168; p=0.062), disease duration (r = −0.137; p=0.128), or age at diagnosis (r = 0.022; p = 0.811).
Analysis of comorbidities showed significantly higher FES-I scores in patients with diabetes (44.25 ± 7.48 vs 36.67 ± 11.67; p = 0.043), depression (39.22 ± 11.83 vs 34.34 ± 10.69; p = 0.022), and sleep apnea (44.44 ± 12.11 vs 36.08 ± 11.15; p = 0.011), compared with those without these conditions. No significant associations were found with other comorbidities.
The relationship between gait parameters and fear of falling showed significant associations with 3 variables: propulsion phase (r = 0.259; p = 0.004), foot clearance (r = 0.198; p = 0.033), and asymmetry (r = −0.241; p = 0.007) (Table 5).
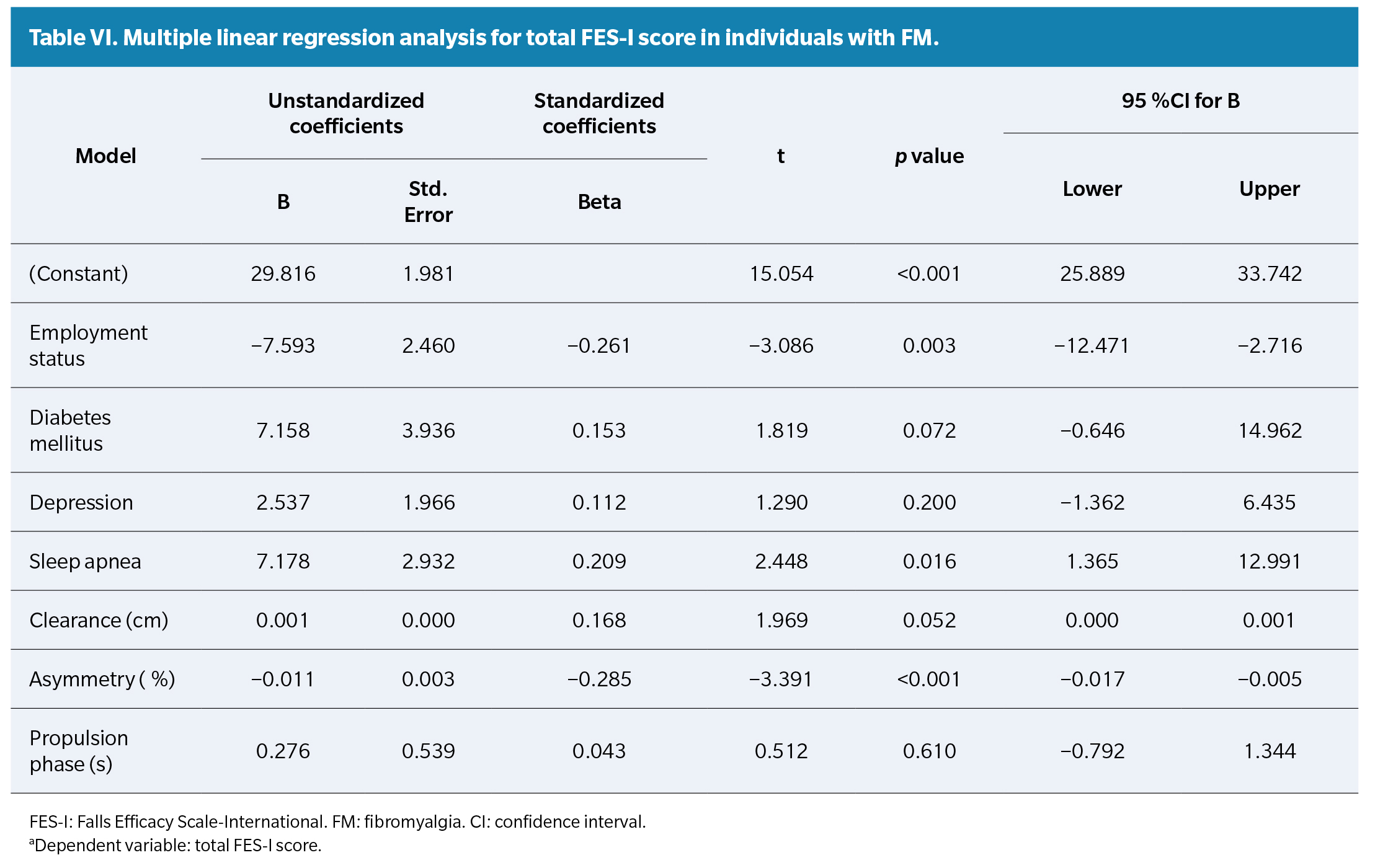
Finally, multivariate analysis (R² = 0.27) showed that being employed was associated with lower fear of falling (p = 0.003), whereas sleep apnea (p = 0.016) and asymmetry (p <0.001) were significantly associated with higher FES-I scores (Table 6).
Discussion
The main objective of this study was to assess the relationship between gait parameters and fear of falling in individuals with FM. Greater fear of falling was associated with increased propulsion phase time, greater foot clearance during gait, and reduced step asymmetry. Although these associations were of low magnitude, they may reflect motor adjustments aimed at maintaining stability and reducing fall risk. However, in multivariate analysis, only asymmetry remained an independent predictor of fear of falling.
Human gait consists of 2 main phases: stance and swing. Within the stance phase, the final stage—propulsion—requires activation of ankle plantar flexors to generate the necessary impulse for forward movement(22). In patients with greater fear of falling, this phase tends to be deliberately prolonged, favoring a more controlled execution. This adaptation has been described as a compensatory response to motor insecurity(5,23). Similarly, studies such as Góes et al.(24) have identified greater plantar flexion during toe-off in women with FM, which may be interpreted as an adaptation to improve postural control at a key moment in the gait cycle. Greater foot clearance during swing, observed in participants with greater fear, may represent a strategy to avoid tripping(25), consistent with Heredia-Jiménez et al. (26), who linked this modification to improved balance control.
The finding of less step asymmetry in individuals with greater fear of falling, though apparently contradictory, may reflect a more symmetrical gait execution as a precise motor control mechanism(5,27). In this regard, Collado-Mateo et al. (28) highlighted that fear of falling is more strongly associated with subjective perception of balance than with actual physical performance, suggesting that individuals adjust their gait pattern in anticipation of perceived risk. The meta-analysis by Carrasco-Vega et al¹² reinforces this interpretation, noting that FM patients tend to adopt a more conservative gait pattern, characterized by lower speed, stride length, and cadence. Such adjustments may represent an adaptive response to elevated fear of falling(12,28).
Consistent with our findings, other studies have reported gait alterations in women with FM, particularly when performing a simultaneous cognitive task. In these situations, a slower and more stable pattern is observed, supporting the idea that dual-tasking ability is impaired in this population(29,30).
The “fibrofog” described in the literature—characterized by impairments in attention, working memory, and executive functions—may hinder gait automatization in individuals with FM, particularly under conditions of higher cognitive or emotional demand such as fear of falling(31). These deficits may contribute to the adoption of slower, more stable gait patterns, consistent with our observations. Additionally, kinesiophobia, widely described in FM, has been linked to greater disease impact, fear of falling, and functional limitations. According to the Fear-Avoidance Model, chronic pain generates fear of recurrence and leads to movement avoidance, perpetuating inactivity and progressive functional decline(32).In this context, fear of movement may contribute to slower, more conservative gait patterns, as a reflection of the need to feel safer while walking.
It has also been reported that individuals with fear of falling show increased muscle co-activation at the ankle joint during gait(33). This greater stiffness, although less efficient, may provide a stronger sense of stability, possibly explaining some of the gait modifications observed in our participants with higher fear.
The mean FES-I score in our sample indicates a moderate level of concern about falls, consistent with previous studies(32,34,35). Higher scores were observed in unemployed individuals, which may be linked to greater functional limitation and elevated perceived risk. These findings are in line with evidence showing that FM significantly affects work performance due to persistent pain, fatigue, and functional impairment, favoring job loss or reduction in working hours(36,37º). Similarly, Ertem and Alp(38) identified kinesiophobia as a factor interfering with work participation, with fear of falling as a potential subtype of this movement avoidance.
This study has several limitations. Consecutive sampling may limit representativeness, and the cross-sectional design precludes causal inference. We did not control for whether participants were experiencing an acute FM flare, which may have influenced symptoms and measurements. Additionally, the wide age range, without an upper limit, may have affected results, as both fear of falling and gait can be influenced by age. Finally, footwear type was not standardized, representing a methodological limitation, since footwear can modify gait parameters.
The findings of this study suggest that certain gait parameters, such as propulsion phase time, foot clearance, and step asymmetry, may serve as useful indicators for assessing fear of falling in individuals with FM. Although associations were of low magnitude, their inclusion in clinical assessment may contribute to a more comprehensive understanding of the patient’s functional status and help guide decisions on interventions aimed at stability and gait safety.
Future studies should include a control group and standardize footwear type among all participants to reduce confounding factors and enhance validity. Additionally, analyzing age influence by including balanced age groups would allow more precise exploration of the role of fear of falling in gait alterations in individuals with FM.
In conclusion, the results of this study show a significant association between fear of falling and specific gait modifications in individuals with FM, namely greater propulsion phase time, greater foot clearance, and lower step asymmetry, although these associations were of low magnitude.
Conflicts of interest
None declared
Funding
None declared
Ethics statement
The study was approved by the Research Ethics Committee on Medicinal Products (CEIm) of the FISABIO Foundation (code: 20241129/06/P)
Authors’ Contributions
Study conception and design: CMC, SZG, ECL. Data collection: CMC, SZG, HPM, ALG. Analysis and interpretation of results: SZG, HPM, ALG. Drafting and manuscript preparation: SZG, AGS, ECL. Final review: CMC, SZG, AGS, ECL
References
- Jahan F, Nanji K, Qidwai W, Qasim R. Fibromyalgia syndrome: An overview of pathophysiology, diagnosis and management. Oman Med J. 2012;27(3):192-5. DOI: 10.5001/omj.2012.44.
- Cabo-Meseguer A, Cerdá-Olmedo G, Trillo-Mata JL. Fibromyalgia: Prevalence, epidemiologic profiles and economic costs. Med Clin (Barc). 2017;149(10):441-8. DOI: 10.1016/j.medcli.2017.06.008.
- Sarzi-Puttini P, Giorgi V, Marotto D, Atzeni F. Fibromyalgia: An update on clinical characteristics, aetiopathogenesis and treatment. Nat Rev Rheumatol. 2020 [citado 9 Jul 2025];16(11):645-60. DOI: 10.1038/s41584-020-00506-w.
- Creed F. The risk factors for self-reported fibromyalgia with and without multiple somatic symptoms: The Lifelines cohort study. J Psychosom Res. 2022;155:110745. DOI: 10.1016/j.jpsychores.2022.110745.
- Da Silva Costa I, Gamundí A, Vivas Miranda JG, Souza França LG, Novaes de Santana C, Montoya P. Altered functional performance in patients with fibromyalgia. Front Hum Neurosci. 2017:11:14. DOI: 10.3389/fnhum.2017.00014.
- Ciaffi J, Brognara L, Gangemi G, Vanni E, Assirelli E, Neri S, et al. Prevalence and characteristics of fibromyalgia in patients with foot and ankle pain: The experience of an academic podiatry clinic. Medicina (Lithuania). 2023;59(1). DOI: 10.3390/medicina59010058.
- De Maya-Tobarra M, Zúnica-García S, Gracia-Sánchez A, Chicharro-Luna E. Relationship between morphofunctional alterations of the foot and its functionality in patients with fibromyalgia syndrome: A case–control study. J Clin Med. 2024;13(21):6439. DOI: 10.3390/jcm13216439.
- López-Muñoz S, Gracia-Vesga MÁ, Gracia-Sánchez A, Zúnica-Garcia S, Gijón-Nogueron G, Chicharro-Luna E. Impact of fibromyalgia and related factors on foot function and quality of life: Cross-sectional study. Foot Ankle Surg. 2023;29(8):627-32. DOI: 10.1016/j.fas.2023.07.014.
- Tornero-Caballero MC, Salom-Moreno J, Cigarán-Méndez M, Morales-Cabezas M, Madeleine P, Fernández-de-Las-Peñas C. Muscle trigger points and pressure pain sensitivity maps of the feet in women with fibromyalgia syndrome. Pain Med. 2016;17(10):1923-32. DOI: 10.1093/pm/pnw090.
- Shookster L, Falke GI, Ducic I, Maloney CT, Dellon AL. Fibromyalgia and Tinel’s sign in the foot. J Am Podiatr Med Assoc. 2004;94(4):400-3. DOI: 10.7547/0940400.
- Jo YS, Yoon B, Hong JY, Joung C Il, Kim Y, Na SJ. Tarsal tunnel syndrome in patients with fibromyalgia. Arch Rheumatol. 2021;36(1):107-13.
- Carrasco-Vega E, Ruiz-Muñoz M, Cuesta-Vargas A, Romero-Galisteo RP, González-Sánchez M. Individuals with fibromyalgia have a different gait pattern and a reduced walk functional capacity: A systematic review with meta-analysis. Pee rJ. 2022;10. DOI: 10.7717/peerj.12908.
- Auvinet B, Bileckot R, Alix AS, Chaleil D, Barrey E. Gait disorders in patients with fibromyalgia. Joint Bone Spine. 2006;73(5):543-6. DOI: 10.1016/j.jbspin.2005.10.020.
- Trevisan DC, Driusso P, Avila MA, Gramani-Say K, Moreira FMA, Parizotto NA. Static postural sway of women with and without fibromyalgia syndrome: A cross-sectional study. Clinical Biomech (Bristol). 2017;44:83-9. DOI: 10.1016/j.clinbiomech.2017.03.011.
- von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. J Clin Epidemiol. 2008;61(4):344-9. DOI: 10.1016/j.jclinepi.2007.11.008.
- Holt GR. Declaration of Helsinki-the world’s document of conscience and responsibility. South Med J. 2014;107(7):407. DOI: 10.14423/SMJ.0000000000000131.
- World Medical Association declaration of Helsinki: Ethical principles for medical research involving human subjects. JAMA. 2013;310(20):2191-4. DOI: 10.1001/jama.2013.281053.
- WHO Technical Report Series Obesity: Preventing and managing the global epidemic. 2000.
- World Health Organization: Physical activity. [citado 11 Ago 2025]. Disponible en: https://www.who.int/news-room/fact-sheets/detail/physical-activity
- Yardley L, Beyer N, Hauer K, Kempen G, Piot-Ziegler C, Todd C. Development and initial validation of the Falls Efficacy Scale-International (FES-I). Age Ageing. 2005;34(6):614-9. DOI: 10.1093/ageing/afi196.
- Lienhard K, Schneider D, Maffiuletti NA. Validity of the Optogait photoelectric system for the assessment of spatiotemporal gait parameters. Med Eng Phys. 2013;35(4):500-4. DOI: 10.1016/j.medengphy.2012.06.015.
- Jiménez Leal R, Gómez Maya M, Dapueto Menchaca D, Escribano Sánchez SM. Estudio articular del miembro inferior durante la fase de apoyo de la marcha. Rev Esp Pod. 2012;23(3):108-10.
- Heredia Jiménez JM, Aparicio García-Molina VA, Porres Foulquie JM, Delgado Fernández M, Soto Hermoso VM. Spatial-temporal parameters of gait in women with fibromyalgia. Clin Rheumatol. 2009;28(5):595-8. DOI: 10.1007/s10067-009-1101-7.
- Góes SM, Leite N, Stefanello JMF, Homann D, Lynn SK, Rodacki ALF. Ankle dorsiflexion may play an important role in falls in women with fibromyalgia. Clin Biomech [Bristol). 2015;30(6):593-8. DOI: 10.1016/j.clinbiomech.2015.03.026.
- Maki BE. Gait changes in older adults: Predictors of falls or indicators of fear? J Am Geriatr Soc. 1997;45(3):313-20. DOI: 10.1111/j.1532-5415.1997.tb00946.x.
- Heredia-Jimenez J, Orantes-Gonzalez E, Soto-Hermoso VM. Variability of gait, bilateral coordination, and asymmetry in women with fibromyalgia. Gait Posture. 2016;45:41-4. DOI: 10.1016/j.gaitpost.2016.01.008.
- Jones KD, Horak FB, Winters-Stone K, Irvine JM, Bennett RM. Fibromyalgia is associated with impaired balance and falls. J Clin Rheumatol. 2009;15(1):16-21. DOI: 10.1097/RHU.0b013e318190f991.
- Collado-Mateo D, Gallego-Diaz JM, Adsuar JC, Domínguez-Muñoz FJ, Olivares PR, Gusi N. Fear of falling in women with fibromyalgia and its relation with number of falls and balance performance. Biomed Res Int. 2015;2015. DOI: 10.1155/2015/589014.
- Radunovi? G, Veli?kovi? Z, Raši? M, Janji? S, Markovi? V, Radovanovi? S. Assessment of gait in patients with fibromyalgia during motor and cognitive dual task walking: A cross-sectional study. Adv Rheumatol. 2021;61:53. DOI: 10.1186/s42358-021-00212-5.
- Martín-Martínez JP, Villafaina S, Collado-Mateo D, Fuentes-García JP, Pérez-Gómez J, Gusi N. Impact of cognitive tasks on biomechanical and kinematic parameters of gait in women with fibromyalgia: A cross-sectional study. Physiol Behav. 2020;227. DOI: 10.1016/j.physbeh.2020.113171.
- Kravitz HM, Katz RS. Fibrofog and fibromyalgia: A narrative review and implications for clinical practice. Rheumatol Int. 2015;35(7):1115-25. DOI: 10.1007/s00296-014-3208-7.
- Leon-Llamas JL, Murillo-Garcia A, Villafaina S, Domínguez-Muñoz FJ, Morenas J, Gusi N. Relationship between kinesiophobia and mobility, impact of the disease, and fear of falling in women with and without fibromyalgia: A cross-sectional study. Int J Environ Res Public Health. 2022;19(14):8257. DOI: 10.3390/ijerph19148257.
- Nagai K, Yamada M, Uemura K, Tanaka B, Mori S, Yamada Y, et al. Effects of fear of falling on muscular coactivation during walking. Aging Clin Exp Res. 2012];24(2):157-61. DOI: 10.1007/BF03654794.
- Denche-Zamorano Á, Pereira-Payo D, Collado-Mateo D, Adsuar-Sala JC, Tomas-Carus P, Parraca JA. Physical function, self-perceived physical fitness, falls, quality of life and degree of disability according to fear and risk of falling in women with fibromyalgia. J Funct Morphol Kinesiol. 2024;9(3):174. DOI: 10.3390/jfmk9030174.
- Collado-Mateo D, Dominguez-Muñoz FJ, Adsuar JC, Merellano-Navarro E, Gusi N. Exergames for women with fibromyalgia: A randomised controlled trial to evaluate the effects on mobility skills, balance and fear of falling. PeerJ. 2017;2017(4):e3211. DOI: 10.7717/peerj.3211.
- Marrero Centeno J, Moreno Velásquez I, Sánchez Cardona I. Fibromialgia en trabajo: explorando su Impacto en el desempeño laboral. Revista Interamericana de Psicología Ocupacional (RIPO). 2017;36(1):9-22.
- Sueiras AS, Souto-Gómez AI, Talavera-Valverde MÁ. Analysis of occupational performance for the promotion of health in people with fibromyalgia. A phenomenological study. Revista Colombiana de Reumatología (Engl Ed). 2019;26(4):227-35.
- Ertem U, Alp A. Kinesiophobia and related factors in fibromyalgia syndrome. Turk J Osteoporos. 2023;29(1):27-32. DOI: 10.4274/tod.galenos.2022.59375.