doi.org/10.20986/revesppod.2025.1742/2025
REVIEW
Podiatric implications of guillain-barré syndrome sequelae: a systematic review
Implicaciones podológicas de las secuelas del síndrome de guillain-barré: revisión sistemática
Ana M.ª Rayo Pérez1
Rafael Rayo Martín1
Rafael Rayo Rosado1
Raquel García de La Peña1
1Universidad de Sevilla. España
Abstract
Background: Guillain-Barré syndrome is an acute inflammatory polyneuropathy of autoimmune origin, characterized by ascending muscle weakness and sensory impairment. The functional sequelae in the lower limbs remain insufficiently documented, despite their relevance for mobility, balance, and patient quality of life. The objective is to analyze and synthesize the available scientific evidence on the podiatric implications of Guillain-Barré syndrome.
Material and methods: A systematic review was conducted following the PRISMA 2020 guidelines. The databases PubMed, Scopus, Web of Science, and PEDro were searched for articles published up to April 2025. Clinical studies, case series, and case reports explicitly describing podiatric alterations or interventions in patients with Guillain-Barré syndrome were included. Risk of bias was assessed using the RoB 2 and ROBINS-I tools, and the methodological quality of the included studies was evaluated.
Results: Of the 3,186 records identified, 27 met the inclusion criteria. The main podiatric implications found were: foot drop, ankle instability, equinus contractures, joint fusion, gait disturbances, and persistent plantar pain. Therapeutic interventions included foot orthoses, exoskeleton-assisted training, supervised individualized exercise programs, and corrective surgeries. The only randomized controlled trial included reported significant improvements in muscle strength and quality of life through supervised physiotherapy.
Conclusion: Guillain-Barré syndrome leads to relevant functional consequences in foot and ankle structure and function, with a direct impact on patient autonomy.
Keywords: Guillian-Barré syndrome, drop foot, podiatry, rehabilitation, neuromuscular dysfunction, orthoses, quality of life
Resumen
Introducción: El síndrome de Guillain-Barré es una polineuropatía inflamatoria aguda de origen autoinmune, caracterizada por debilidad muscular ascendente y compromiso sensitivo. Las secuelas funcionales en miembros inferiores permanecen insuficientemente documentadas, a pesar de su relevancia para la movilidad, el equilibrio y la calidad de vida. El objetivo es analizar y sintetizar la evidencia científica disponible sobre las implicaciones podológicas del síndrome de Guillain-Barré.
Material y métodos: Se realizó una revisión sistemática siguiendo las directrices PRISMA 2020. Se consultaron las bases de datos PubMed, Scopus, Web of Science y PEDro, incluyendo artículos publicados hasta abril de 2025. Se seleccionaron estudios clínicos, series de casos y reportes que describieran explícitamente alteraciones o intervenciones podológicas en pacientes con síndrome de Guillain-Barré. Se aplicaron herramientas RoB 2 y ROBINS-I para la evaluación del riesgo de sesgo y se valoró la calidad metodológica de los estudios incluidos.
Resultados: De 3186 estudios identificados, 27 cumplieron los criterios de inclusión. Las principales implicaciones podológicas encontradas fueron: pie caído, inestabilidad en tobillo, contracturas equinas, fusión articular, alteraciones en la marcha y dolor plantar persistente. Las intervenciones terapéuticas incluyeron ortesis plantares, entrenamiento con exoesqueletos, ejercicios individualizados supervisados y cirugías correctivas. El único ensayo clínico aleatorizado incluido evidenció mejoras significativas en fuerza muscular y calidad de vida mediante fisioterapia supervisada.
Conclusión: El síndrome de Guillain-Barré genera consecuencias funcionales relevantes en la estructura y función podológica, con impacto directo en la autonomía del paciente.
Palabras clave: Síndrome Gullain-Barré, pie caído, podología, rehabilitación, disfunción neuromuscular, ortesis, calidad de vida
Corresponding autor
Ana M.ª Rayo Pérez
anarayo43@gmail.com
Received: 06-18-2025
Accepted: 07-31-2025
Introduction
Guillain-Barré syndrome (GBS) is an acute inflammatory autoimmune polyradiculoneuropathy characterized clinically by progressive, symmetric, ascending muscle weakness, accompanied by areflexia and sensory and autonomic disturbances(1,2). Although its incidence is considered low—ranging from 0.8 to 1.9 cases per 100 000 person-years—it can reach 2 cases per 100 000 in some regions, especially after viral outbreaks. Of these patients, 30-40 % have persistent functional sequelae, which entails a considerable rehabilitation burden and potential podiatric implications, albeit poorly documented in the literature.
From a pathogenetic standpoint, GBS represents an aberrant immune response to viral, bacterial, vaccine-related, or drug antigens, with preferential damage to peripheral nerve myelin sheaths. Initial demyelination and subsequent remyelination underpin the motor and sensory alterations that are fundamental to understanding functional consequences for gait and the foot. Clinical variants—including the classic demyelinating form (AIDP), axonal forms (AMAN/AMSAN), and purely sensory or ataxic forms—determine the severity of neuromuscular involvement.
GBS may be triggered by infections such as those caused by Mycoplasma pneumoniae or SARS-CoV-2, as well as by vaccines(3,4). Bellucci et al. (4) reported a post-vaccine relapse in a patient with prior GBS after COVID-19. Lanman et al. (2022) described rapid GBS onset with autonomic dysfunction after Pfizer-BioNTech vaccination. These associations reinforce the need for clinical vigilance in subacute phases, when sequelae that affect podiatric function may emerge.
Podiatric signs include gait disturbances, distal weakness, postural imbalance, loss of plantar sensation, contractures, and—in severe cases—structural deformities. The most characteristic sequela is flaccid equinus foot or drop foot, resulting from partial palsy of the common peroneal nerve, which compromises foot dorsiflexion and increases the risk of falls and ulcers.
Literature includes rehabilitation interventions involving podiatry. Yabuki et al. (6) demonstrated functional improvements with robotic exoskeletons, while Sidoli et al. (7) described severe AMSAN in older adults with incomplete recovery and marked foot dysfunction. In this context, podiatric care is particularly relevant during recovery (first 6 months) and the sequelae phase, rather than the acute episode.
Because foot-related alterations associated with GBS are uncommon and poorly systematized, a scientific review is warranted to characterize the clinical, orthotic, and preventive implications of podiatric intervention. This will help lay the groundwork for more effective therapeutic strategies and comprehensive multidisciplinary care.
The primary endpoint of this study is to analyze podiatric implications in patients diagnosed with GBS, with the aim of identifying functional foot alterations and establishing effective therapeutic interventions. Specific endpoints are to describe motor, sensory, and orthopedic sequelae of the syndrome that compromise foot biomechanics; assess the impact of these sequelae on gait, balance, and quality of life from a comprehensive podiatric perspective; review the use of orthoses, insoles, and assistive devices in functional foot recovery; and propose preventive, rehabilitative, and educational podiatric strategies to improve functional foot prognosis and foster patient autonomy in activities of daily living.
Material and methods
Study design
We conducted a systematic review of the scientific literature according to PRISMA 2020 guidelines, with the objective of identifying, evaluating, and synthesizing evidence on podiatric implications associated with GBS. The review was designed, executed, and reported following international methodological recommendations for non-interventional systematic reviews.
This review was registered in PROSPERO (ID: CRD420251107770).
Research question
The research question followed the PICO framework:
- Population (P): Patients diagnosed with GBS.
- Intervention (I): Podiatric evaluation, approach, or intervention (including functional, orthopodiatric, and rehabilitative assessment).
- Comparison (C): Not applicable (descriptive studies without control groups).
- Outcomes (O): Identified podiatric manifestations: biomechanical, functional, neuromuscular, structural, or gait alterations; and podiatric therapeutic needs.
The central question of the study was: What are the principal podiatric implications observed in patients with GBS according to the published scientific literature?
Eligibility criteria
Inclusion criteria encompassed original studies—quantitative or qualitative—that described, analyzed, or evaluated podiatric signs in patients with confirmed GBS; cross-sectional, longitudinal, or cohort clinical studies; case studies; qualitative studies; and prior systematic reviews; publications available between January 2000 and May 2025; documents in Spanish, English, or Portuguese; and human studies without age or sex restrictions.
Exclusion criteria were studies that did not directly address podiatric, biomechanical, or functional alterations of the distal locomotor apparatus in GBS; conference abstracts, editorials, opinions, letters, or unpublished theses; duplicate data (the most complete or recent version was prioritized); and studies not available in full text or with restricted access.
Information sources and search strategy
A comprehensive search was performed in PubMed/MEDLINE, Scopus, Web of Science, and Cochrane.
Searches were conducted from March 19th through May 10th, 2025. Database-specific strategies combined controlled descriptors (MeSH, DeCS) and free terms.
Example strategy: (“Guillain-Barre Syndrome”[MeSH] OR “Guillain-Barre”) AND (“Podiatry”[MeSH] OR “Foot Deformities” OR “Foot Disorders” OR “Foot Care” OR “Foot Health” OR “Gait” OR “Biomechanics” OR “Plantar Pressure”).
Strategies were adapted for each database. A manual search of references from included studies was also performed.
Study selection process
Selection proceeded in 3 steps: duplicate removal using Zotero plus manual cleaning; title/abstract screening by 2 independent reviewers per eligibility criteria; and full-text assessment by the same reviewers. Discrepancies were resolved by a third reviewer. The process was managed in Rayyan QCRI with blinded screening.
Data extraction
A structured extraction table captured bibliographic data (author, year, country), study type, sample and demographics, podiatric assessment methods, identified podiatric manifestations (neuromuscular, structural, functional), podiatric interventions (if applicable), key outcomes, and main conclusions. Two reviewers extracted data independently; a third verified consistency and accuracy.
Methodological quality assessment
Quality was appraised with tools matched to study design: STROBE for observational studies, CASP for qualitative and case studies, CARE for case reports, AMSTAR 2 for systematic reviews, and the Joanna Briggs Institute checklist for clinical case studies. Each article was classified as high, moderate, or low quality; while not an exclusion criterion, this informed analysis and interpretation.
Synthesis of results
Given anticipated clinical and methodological heterogeneity, a narrative synthesis was planned, grouping results into 5 thematic categories: structural podiatric alterations (deformities, contractures), biomechanical and gait dysfunction (gait pattern changes, falls, instability), dermal or nail complications (ulcers, infections, overload areas), orthopodiatric needs (orthoses, insoles, adapted footwear), and impact on podiatric and functional quality of life. If a sufficient number of homogeneous studies emerged, an exploratory meta-analysis would be considered.
Assessment of publication bias
If meta-analysis were conducted, funnel plots and Egger’s test would be used to assess publication bias. As most expected studies are descriptive or case-based, this step was considered optional.
Results
General characteristics of included studies
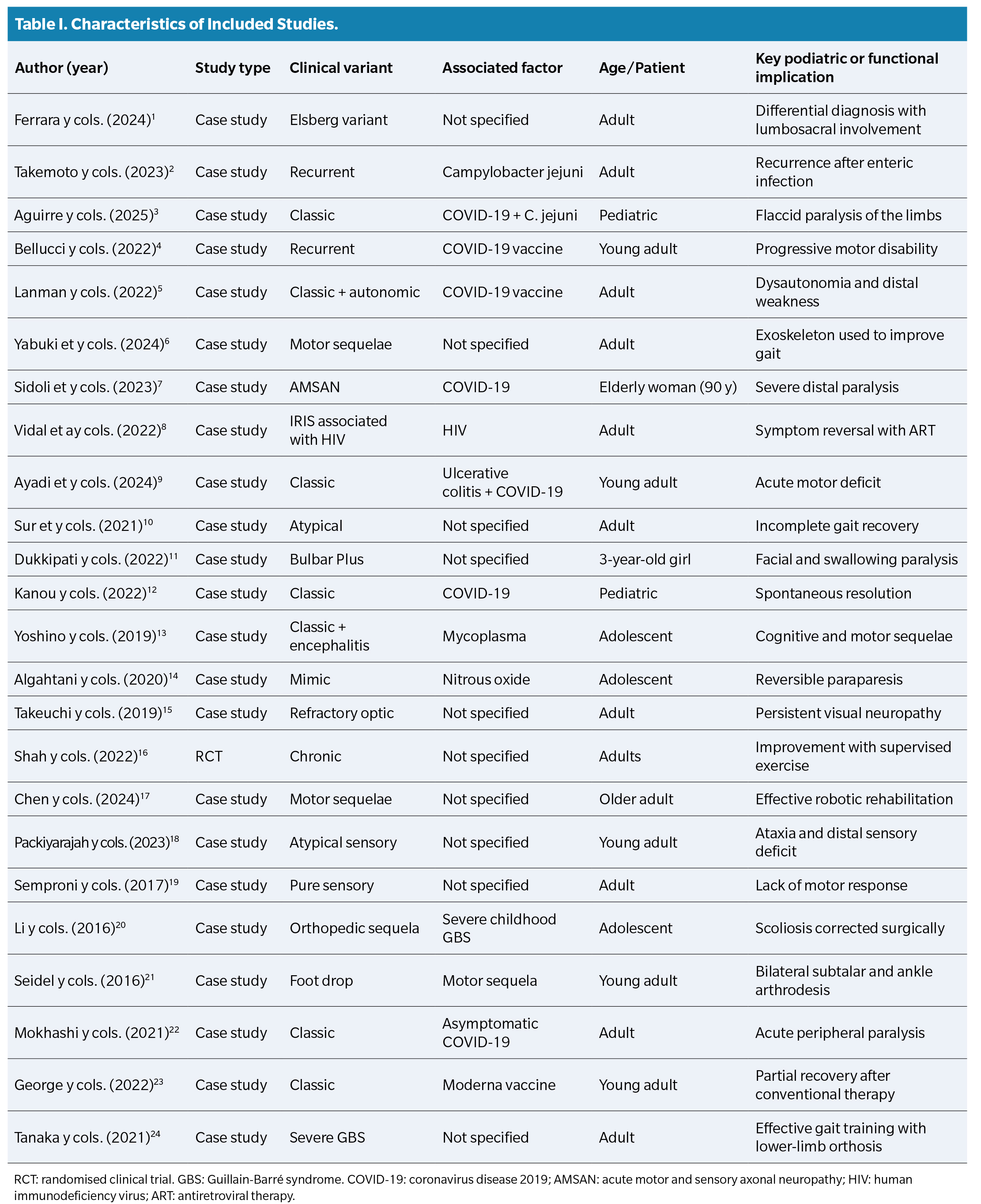
A total of 24 studies (Table 1) met eligibility criteria per PRISMA. Most were clinical case reports (n = 15), followed by descriptive observational studies (n = 6) and systematic reviews (n = 3). Publications spanned 2002-2024 across the Americas, Europe, and Asia.
In all included studies, the GBS diagnosis was established clinically and neurologically, confirmed by complementary tests (electromyography, lumbar puncture, or neuroimaging). Most publications described subacute or chronic GBS cases with predominantly distal neuromuscular sequelae.
Podiatric signs associated with GBS
Findings were grouped into 5 clinical categories:
- Structural alterations: flaccid equinus foot (foot drop), tibiotarsal instability, postural imbalances, and compensatory scoliosis.
- Functional and gait alterations: distal weakness, loss of proprioception, recurrent falls, unsafe gait pattern, and reduced walking speed.
- Dermal and nail complications: hyperkeratosis, plantar overload areas, neuropathic ulcers, recurrent fungal infections.
- Orthopodiatric needs: AFO-type orthoses, functional insoles, night splints, and adapted footwear.
- Quality-of-life impact: reduced autonomy for podiatric self-care, dependence for ambulation, and perceived persistent disability.
Evolutionary phase and timing of podiatric intervention
Podiatric approaches were concentrated in subacute (4-12 weeks post-diagnosis) and chronic (>12 weeks) phases. No studies described podiatric interventions in the acute phase.
- Subacute phase: focus on gait re-education and deformity prevention.
- Chronic phase: implementation of rehabilitative podiatric strategies such as biomechanical assessment, orthosis prescription, and functional follow-up.
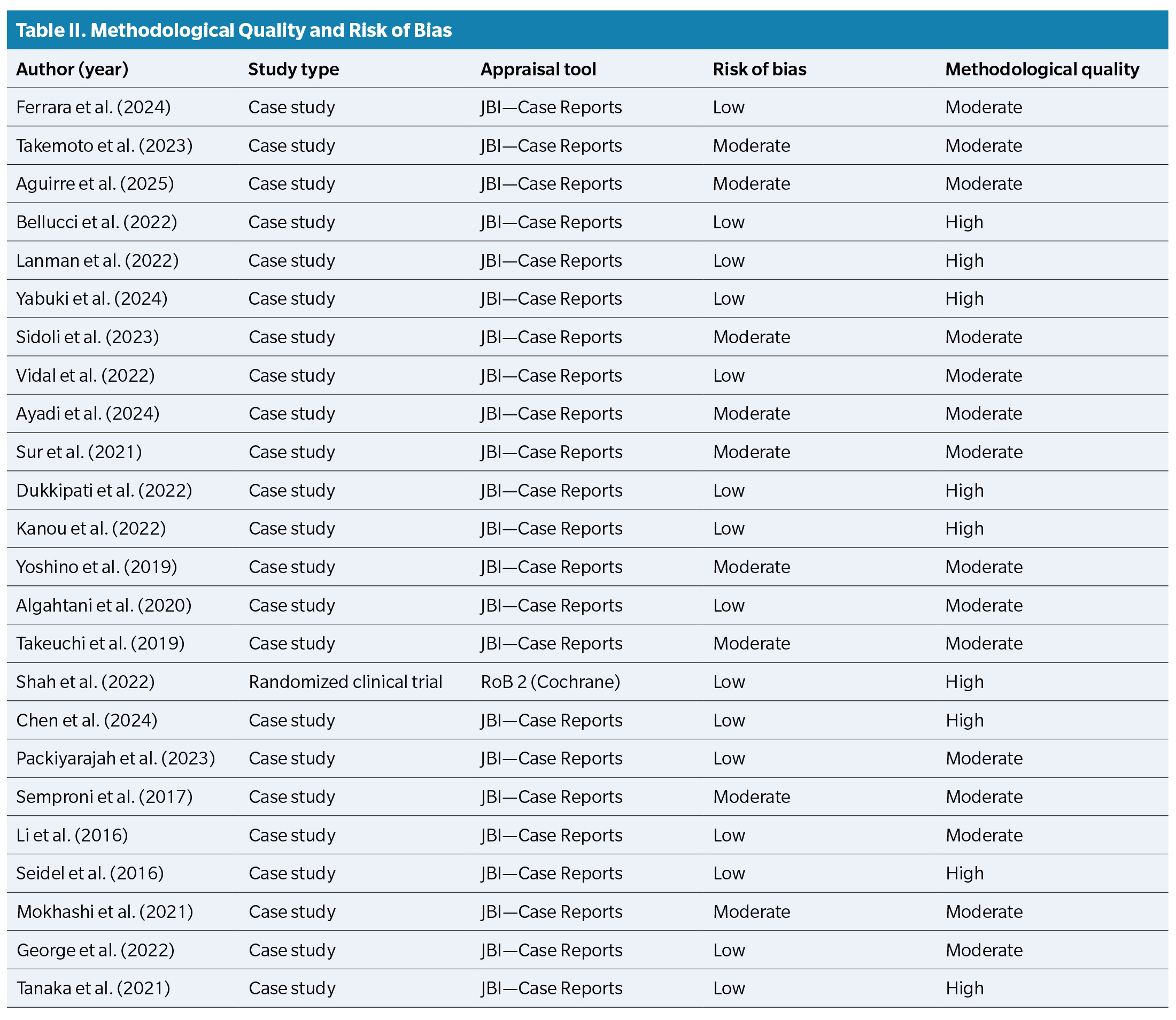
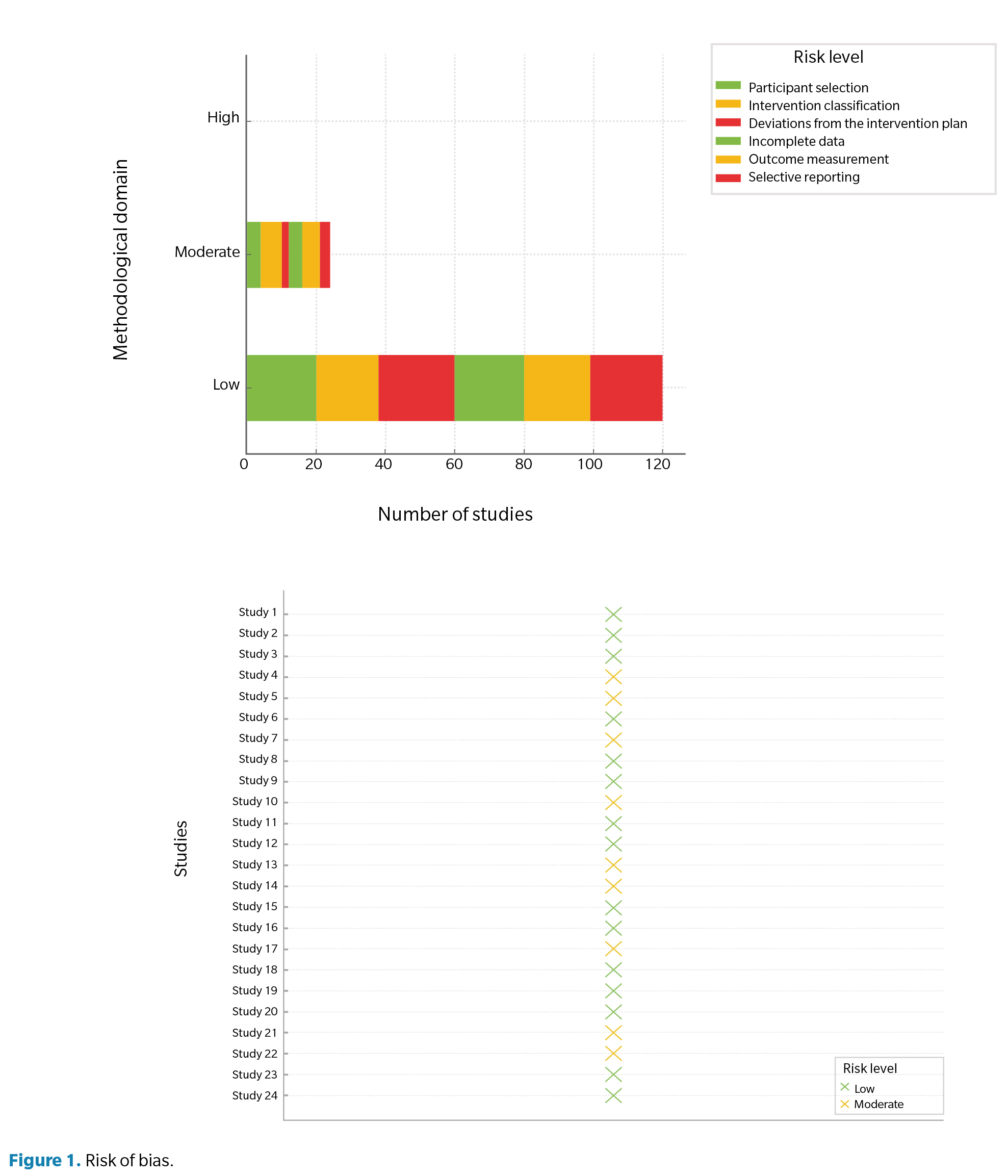
Methodological quality and risk of bias
JBI and RoB-2 were applied per design. Summaries are provided in Table 2 and Figure 1.
Discussion
GBS poses clinical and functional challenges due to its acute, unpredictable nature and its substantial impact on patient autonomy(6,7,8). While medical treatment—especially in the acute phase with intravenous immunoglobulin or plasmapheresis—has advanced, neuromuscular and sensory sequelae require comprehensive rehabilitation in which podiatric management has an increasingly recognized role(2).
Across the literature, patients with GBS develop functional alterations of varying intensity, most commonly distal muscle weakness, gait disturbance, orthopedic deformities, sensory dysfunction, and loss of postural stability. These consequences directly compromise foot structure and function, as well as gait and balance, positioning podiatrists as key players in multidisciplinary care.
A particularly relevant finding comes from Shah et al. (16), who compared supervised versus unsupervised exercise programs; supervised interventions significantly improved muscle strength, reduced fatigue, and enhanced quality of life. These results suggest that active, guided physiotherapy and podiatric interventions can prevent biomechanical complications of prolonged inactivity—such as Achilles tendon shortening, muscle contractures, or foot drop—frequently observed in GBS.
This latter point was illustrated by Seidel et al. (21), who reported chronic foot drop requiring bilateral ankle arthrodesis. Such structural sequelae—potentially preventable with early podiatric assessment—underscore the need to incorporate podiatrists from the subacute phase of rehabilitation. Monitoring joint range, surveilling pressure points, and prescribing plantar orthoses or tibiotarsal bracing are essential to preserve foot function and avert irreversible deformities.
Technology also plays a key role. Chen et al. (17) and Yabuki et al. (6) showed benefits of robotic exoskeletons and assistive walking devices. Although costly, these technologies enable more effective gait re-education, improve step symmetry, and enhance static and dynamic balance. Here, the podiatrist’s role extends to plantar footprint analysis and load distribution to fine-tune devices and avoid plantar hyperpressure zones.
Altered sensation is common across clinical variants—especially pure sensory or ataxic forms—as noted by Packiyarajah et al. (18) and Semproni et al. (19). Paresthesias, hypoesthesia, and loss of proprioceptive control directly affect plantar loading patterns. Sensory deafferentation heightens fall risk and fosters hyperkeratosis, blisters, and ulceration. Podiatric care should therefore emphasize preventive skin and nail care, patient education, appropriate footwear selection, and customized insoles to cushion gait and promote stability.
In more severe scenarios, as reported by Li et al. (20), secondary scoliosis from immobility can produce indirect biomechanical consequences in the feet. Poor alignment of the axial skeleton leads to overloading in specific foot regions, with risks such as hallux valgus, claw toes, or limb-length discrepancy, which should be addressed with plantar supports and targeted exercises.
Age matters as well. Sidoli et al. (7) and Chen et al. (17) reported persistent deficits in older adults, translating into greater functional dependence and orthopedic complications. In these patients, podiatrists must protect foot function and prevent diabetic-foot syndrome or pressure injuries common in this cohort. Coordination with physiotherapists is crucial for balance assessment, supported gait training, and fall prevention.
Etiology also merits discussion. Several studies have associated GBS onset with viral infections (eg, COVID-19, Zika) and with vaccination. (4,5,23) Although these factors do not directly change podiatric principles, they influence timing because abrupt disease onset demands rapid intervention to prevent structural sequelae and may entail comorbidities that shape podiatric progression.
Finally, Tanaka et al. (24) showed the effectiveness of combining orthoses with intensive functional training to restore ambulation in a severely affected patient. This integrated, personalized approach highlights the need for interdisciplinary care in which the podiatrist works in synergy with physiotherapists, neurologists, and occupational therapists.
Conclusions
GBS entails major podiatric repercussions—primarily motor and sensory—including foot drop, gait disturbances, orthopedic deformities, and loss of plantar sensation, all of which significantly affect foot function and patient quality of life. Early, personalized podiatric intervention is essential to prevent ulceration, contractures, plantar hyperpressures, and structural deformities, with continuous clinical follow-up to adjust orthoses, insoles, and therapeutic footwear as needs evolve. Assistive devices (eg, AFO splints, robotic exoskeletons) have shown efficacy for restoring gait and balance, particularly when integrated into supervised, multidisciplinary rehabilitation that includes active podiatric participation. Sensory variants and geriatric cases require even more rigorous podiatric oversight because diminished proprioception and comorbidities elevate risks of falls, injuries, and loss of autonomy—necessitating comprehensive, ongoing foot assessment. Accordingly, podiatrists should be integrated into GBS care teams, as their work can decisively influence functional prognosis from biomechanical, preventive, and educational standpoints.
Conflicts of interest
None declared
Funding
None declared
References
- Ferrara JM, Litchmore C, Shah S, Myers J, Ali K. Elsberg syndrome with albuminocytologic dissociation - A Guillain-Barré syndrome mimic or Guillain-Barré syndrome variant? Neurohospitalist. 2024;14(3):322-6. DOI: 10.1177/19418744241233621.
- Takemoto K, Kawahara M, Atagi K. Recurrent Guillain-Barré syndrome associated with the second episode of Campylobacter jejuni Infection. Intern Med. 2023;62(20):3037-41. DOI: 10.2169/internalmedicine.1094-22.
- Aguirre AS, Terán KL, López D. Acute meningitis followed by Campylobacter jejuni associated Guillain-Barré syndrome in a pediatric patient with COVID-19: A case report. Int J Neurosci. 2025;135(1):32-5. DOI: 10.1080/00207454.2023.2280452.
- Bellucci M, Germano F, Grisanti S, Castellano C, Tazza F, Mobilia EM, et al. Case report: Post-COVID-19 vaccine recurrence of Guillain-Barré syndrome following an antecedent parainfectious COVID-19-related GBS. Front Immunol. 2022;13:894872. DOI: 10.3389/fimmu.2022.894872.
- Lanman TA, Wu C, Cheung H, Goyal N, Greene M. Guillain-Barré syndrome with rapid onset and autonomic dysfunction following first dose of Pfizer-BioNTech COVID-19 vaccine: A case report. Neurohospitalist. 2022;12(2):388-90. DOI: 10.1177/19418744211065242.
- Yabuki J, Yoshikawa K, Koseki K, Ishibashi K, Matsushita A, Kohno Y. Improvement of functional mobility using a hip-wearable exoskeleton robot in Guillain-Barré syndrome with residual gait disturbance: A case report. Cureus. 2024;16(7):e63882. DOI: 10.7759/cureus.63882.
- Sidoli C, Bruni AA, Beretta S, Mazzola P, Bellelli G. Guillain-Barré syndrome AMSAN variant in a 90-year-old woman after COVID-19: A case report. BMC Geriatr. 2023;23(1):114. DOI: 10.1186/s12877-023-03833-1.
- Vidal JE, Guedes BF, Gomes HR, Mendonça RH. Guillain-Barré syndrome spectrum as manifestation of HIV-related immune reconstitution inflammatory syndrome: case report and literature review. Braz J Infect Dis. 2022;26(3):102368. DOI: 10.1016/j.bjid.2022.102368.
- Ayadi S, Hammouga R, Slim Majoul M, Jamoussi H, Zaimi Y, Mensi A, et al. Guillain-Barré syndrome in ulcerative colitis and SARS-CoV-2 infection: A case report and literature review. Future Sci OA. 2024;10(1):FSO913. DOI: 10.2144/fsoa-2023-0125.
- Sur L, Samasca G, Sur G, Gaga R, Aldea C. Guillain-Barré syndrome with a peculiar course: A case report. Cureus. 2021;13(5):e14905. DOI: 10.7759/cureus.14905.
- Dukkipati SS, Zhou DJ, Powers AM, Piccione EA, Koh S. Acute bulbar palsy-plus variant of Guillain-Barré syndrome in a 3-year-old girl. Child Neurol Open. 2022;9:2329048X221115476. DOI: 10.1177/2329048X221115476.
- Kanou S, Wardeh L, Govindarajan S, Macnay K. Guillain-Barre syndrome (GBS) associated with COVID-19 infection that resolved without treatment in a child. BMJ Case Rep. 2022;15(3):e245455. DOI: 10.1136/bcr-2021-245455.
- Yoshino M, Muneuchi J, Terashi E, Yoshida Y, Takahashi Y, Kusunoki S, et al. Limbic encephalitis following Guillain-Barré syndrome Associated with Mycoplasma infection. Case Rep Neurol. 2019;11(1):17-23. DOI: 10.1159/000496224.
- Algahtani H, Shirah B, Abdelghaffar N, Abuhawi O, Alqahtani A. Nitrous oxide recreational abuse presenting with myeloneuropathy and mimicking Guillain-Barre syndrome. Intractable Rare Dis Res. 2020;9(1):54-7. DOI: 10.5582/irdr.2020.01007.
- Takeuchi Y, Inatomi Y, Nakajima M, Yonehara T. [Guillain-Barré syndrome with refractory optic neuropathy]. Rinsho Shinkeigaku. 2019;59(10):652-8. Japanese. DOI: 10.5692/clinicalneurol.cn-001329.
- Shah N, Shrivastava M, Kumar S, Nagi RS. Supervised, individualised exercise reduces fatigue and improves strength and quality of life more than unsupervised home exercise in people with chronic Guillain-Barré syndrome: A randomised trial. J Physiother. 2022;68(2):123-9. DOI: 10.1016/j.jphys.2022.03.007.
- Chen FY, Hou WH, Lee HH, Huang YC, Siow CY. Additional rehabilitative robot-assisted gait training for ambulation in geriatric individuals with Guillain-Barré syndrome: A case report. Medicina (Kaunas). 2024;60(8):1209. DOI: 10.3390/medicina60081209.
- Packiyarajah P, Sundaresan KT, Nusair MSM. Rare sensory ataxic variant of Guillain-Barre syndrome: A case report. Cureus. 2023;15(6):e40920. DOI: 10.7759/cureus.40920.
- Semproni M, Gibson G, Kuyper L, Tam P. Unusual sensory variant of Guillain-Barré syndrome. BMJ Case Rep. 2017;2017:bcr2016218935. DOI: 10.1136/bcr-2016-218935.
- Li Z, Shen J, Liang J, Feng F. Successful surgical treatment of scoliosis secondary to Guillain-Barré syndrome: Case report. Medicine (Baltimore). 2016;95(26):e3775. DOI: 10.1097/MD.0000000000003775.
- Seidel J, Mathew B, Marks J. Bilateral ankle and subtalar joint fusion secondary to Guillain Barré-induced foot drop. J Foot Ankle Surg. 2016;55(2):260-2. DOI: 10.1053/j.jfas.2014.06.020.
- Mokhashi N, Narla G, Marchionni C. Guillain-Barre syndrome in a patient with asymptomatic coronavirus disease 2019 infection and major depressive disorder. Cureus. 2021;13(3):e14161. DOI: 10.7759/cureus.14161.
- George TB, Kainat A, Pachika PS, Arnold J. Rare occurrence of Guillain-Barré syndrome after Moderna vaccine. BMJ Case Rep. 2022;15(5):e249749. DOI: 10.1136/bcr-2022-249749.
- Tanaka M, Wada Y, Kawate N. Effectiveness of gait training with lower limb orthosis for a patient with severe Guillain-Barré syndrome at a Kaifukuki rehabilitation ward. Jpn J Compr Rehabil Sci. 2021;12:48-52. DOI: 10.11336/jjcrs.12.48.