DOI: http://dx.doi.org/10.20986/revesppod.2024.1678/2023
ORIGINAL
Surgical approach to rheumatic foot. Case series
Abordaje quirúrgico del pie reumático. Serie de casos
Ana M.ª Rayo Pérez1
Francisco Javier Rodríguez Castillo2
Rafael Rayo Rosado3
María Reina Bueno3
1Clínica Rayo. Arahal, Sevilla, España
2Clínica PieFit. Tomares, Sevilla, España
3Universidad de Sevilla, España
Abstract
Introduction: Rheumatoid arthritis is an autoimmune, inflammatory, chronic and progressive disease that affects the musculoskeletal system and can cause deformity, pain and decreased function of the foot, being able to observe the presence of a triangular forefoot and claw toes with decreased of mobility and pain. Its treatment can be conservative and/or surgical.
Patients and methods: 20 cases of patients with rheumatoid arthritis who underwent arthrodesis of the first metatarsophalangeal joint and metatarsal panresection, accompanied or not by digital alignment, are presented. Immediate post-surgical and post-surgical follow-up after one year of evolution are assessed.
Results: After the intervention, a Likert scale satisfaction mean of 9.10 and a visual analogue pain scale mean of 0.40 were achieved. Likewise, a considerable decrease in the hallux abductus valgus angles and intermetatarsal angle I-II is achieved.
Conclusions: The combination of arthrodesis of the first metatarsophalangeal joint with metatarsal pan-resection is the choice in this type of patient, since it increases the functionality of the foot and significantly reduces pain symptoms.
Keywords: Arthrodesis, rheumatoid arthritis, foot, metatarsophalangeal joint, surgical treatment
Resumen
Introducción: La artritis reumatoide es una enfermedad autoinmune, inflamatoria, crónica y progresiva, que afecta al aparato locomotor y que puede provocar deformidad, dolor y disminución de la función del pie, pudiéndose observar la presencia de un antepié triangular y dedos en garra con disminución de la movilidad y dolor. Su tratamiento puede ser conservador y/o quirúrgico.
Pacientes y métodos: Se presentan 20 casos de pacientes con artritis reumatoide intervenidos mediante artrodesis de la primera articulación metatarsofalángica y panresección metatarsal, acompañado o no de alineamiento digital. Se valora seguimiento postquirúrgico inmediato y postquirúrgico al año de evolución.
Resultados: Tras la intervención, se consigue una media de satisfacción de la escala Likert de 9.10 y una media de la escala visual analógica de dolor de 0.40. Asimismo, se consigue una disminución considerable de los ángulos hallux abductus valgus y ángulo intermetatarsal I-II.
Conclusiones: La combinación de artrodesis de la primera articulación metatarsofalángica con la panresección metatarsal es de elección en este tipo de pacientes, ya que permite aumentar la funcionabilidad del pie y disminuir significativamente la sintomatología dolorosa.
Palabras clave: Artrodesis, artritis reumatoide, pie, articulación metatarsofalángica, tratamiento quirúrgico
Corresponding author: Ana M.ª Rayo Pérez
anarayo43@gmail.com
Received: 11-11-2023
Accepted: 01-30-2024
Introduction
Rheumatoid arthritis is an autoimmune, inflammatory, chronic, and progressive disease that affects the musculoskeletal system. It usually appears from the age of 25, worsening with the onset of menopause. It is more common in women between 40 and 60 years old and affects more than 0.5 % of the world’s population. In Spain, the prevalence is estimated at 1.0 7%, with over 497 000 affected individuals1,2).
Rheumatoid foot refers to the involvement of the foot by rheumatoid arthritis, leading to deformity, pain, and decreased functionality. It manifests in 90 % of cases, with the involvement of the forefoot being more frequent in 20 % of cases, especially at the metatarsophalangeal joint of the hallux. There is also often a decrease in the capsuloligamentous complex of the first metatarsophalangeal joint, which increases the valgus displacement of the metatarsal, causing a transfer of load to the lesser rays. Similarly, there is synovitis and destruction of these joints, leading to progressive subluxation and resulting in a decrease and distal displacement of the plantar pad, causing prominence of the metatarsal heads with associated plantar hyperkeratosis(1,3,4,5,6).
As disease progresses and joint destruction leads to a decrease in the patient’s functionality and quality of life, surgical intervention is the best option. Techniques such as joint function preservation (if feasible), joint replacement techniques, or, in cases of severe joint destruction, arthrodesis techniques can be performed. Metatarsal fusion and pan-metatarsal resection, also known as the Clayton and Hoffman technique, are indicated in patients with functional impairment, severe deformity, and pain, i.e., it is indicated for the treatment of severe rheumatic forefoot deformities(7).
This technique allows for immediate ambulation with a flat postoperative shoe, rapid functional recovery, and pain-free walking in the short, medium, and long term. However, it results in a propulsive foot with slightly shorter forefoot than the contralateral one, but asymptomatic(8,9).
The objective of this study is to determine the influence of surgical intervention using the Clayton and Hoffman technique in a series of cases of patients with rheumatic foot.
Patients and methods
Study population
This study consists of a series of clinical cases of rheumatic patients who underwent surgical intervention at Centro Sanitario Clínica Rayo in Arahal, Seville.
Twenty clinical cases collected from January through December 2022 at the Centro Sanitario Clínica Rayo in Arahal, Seville, are presented in this article. The patients attended the clinic sequentially and consecutively, without randomization, during the months of January to December 2022. All patients diagnosed with rheumatoid arthritis and deformity and/or pain in the forefoot undergoing surgical intervention consisting of metatarsophalangeal joint arthrodesis along with pan-metatarsal metatarsal resection of 2nd to 5th metatarsals (Clayton and Hoffman techniques) were included. Cases of rheumatic patients operated on during this period who did not undergo this surgical technique and those patients who refused surgery and preferred other types of conservative approach for their condition were excluded.
Protocol and data collection
Prior to data collection, the medical history was reviewed to collect generic variables (height, weight, body mass index, and laterality), surgical risk categorization (ASA scale), deep vein thrombosis risk categorization (Autar scale), SF-36 scale, AOFAS scale, reason for consultation, and clinical assessment of pain (VAS scale). Preoperative assessment consisted of a clinical examination to observe the deformity, both in weight-bearing and non-weight-bearing, and various maneuvers were performed to assess joint ranges of motion, paying attention to the location of pain and/or different hyperkeratosis associated with the deformity. Additionally, a vascular study was conducted in which pedal and posterior tibial pulses were palpated accompanied by an echo-Doppler and ankle-brachial index (ABI) measurement. Furthermore, a gait biomechanical study, both baropodometric and dynamic, was performed, and finally, a radiological study (Figure 1) of the foot to be operated.

After obtaining informed consent for participation in the clinical study, basic preoperative blood tests were requested, including a complete blood count, biochemical study, coagulation study, rheumatoid factor, vitamin D, and glycated hemoglobin. All patients showed positive rheumatoid factor and increased erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) levels and were operated on in a hospital setting with proximal anesthetic blockade accompanied by sedation.
Analyzed variables
A Visual Analog Scale (VAS) ranging from 0 to 10 points was used to assess general foot pain, an AOFAS scale, a LIKERT scale was used to assess patient satisfaction, as well as the SF-36 health questionnaire in Spanish. These scales were administered both preoperatively and 1 year after surgery.
Along with these scales, a radiological analysis of the deformity on the Weight-Bearing Dorsoplantar X-ray was performed, assessing the following angles: intermetatarsal angle, hallux abductus valgus angle, Merchan angle, and hallux interphalangeal angle. This measurement was performed on preoperative x-rays and postoperative x-rays 1 year after surgery.
Surgical technique
Regarding the surgical procedure, first, fusion of the first metatarsophalangeal joint was performed through a dorsomedial approach, which required dissection through planes with subsequent “T” capsulotomy and resection of the articular surfaces of the head of the first metatarsal and the base of the proximal phalanx using bone rongeur forceps, “cup in ball” system, or reciprocal cuts with a pneumatic saw (authors’ preference). This surgical step was accompanied by drilling to accelerate the fusion process of both structures, followed by temporary fixation of both segments with three 1.4 mm Kirschner wires (crossing in the central area of the junction of these segments), which were removed 4 to 5 weeks later. We should mention that arthrodesis was performed with a dorsiflexion position of 10º to allow for subsequent patient propulsion, and according to other authors such as Koutsouradis et al. (10) and Myerson et al. (11), fixation is preferred using low-profile plates or two 2.5 mm conical screws.
Second, a pan-metatarsal resection was performed through a “golf club” incision via dorsal approach using the Clayton incision or via plantar approach using the Hoffman incision, sequentially by resecting the metatarsal heads from the 2nd to the 5th metatarsals. Additionally, in cases where it was necessary, digital alignment of the lesser toes was performed by arthrodesis of the 2nd and 3rd toes and arthroplasties of the 4th and 5th toes, all fixed with 1.2 mm Kirschner wires to the metatarsal diaphysis, which were removed at 3-4 weeks. This procedure may be accompanied by percutaneous tenotomies of the common flexor of the toes at the diaphysis level of the proximal phalanx of these toes.
After having performed all the procedures described above, closure was performed by planes with absorbable suture for deep planes and continuous festooned suture in the superficial plane of the skin. Subsequently, a postoperative intralesional infiltration was performed with 0.5 % bupivacaine and 4 mg dexamethasone phosphate to control postoperative pain and inflammation, and after that, a non-adherent absorbent dressing and a semi-compressive bandage were applied (Figure 2).

In this type of procedures, the expected pain is moderate, so tramadol with paracetamol (37.5/325 mg/8 hours) was chosen for the first two days, followed by an analgesic regimen consisting of the combined use of metamizole (575 mg/8 hours) and paracetamol (1 g/8 hours), alternated every 4 hours. Similarly, antibiotic prophylaxis with azithromycin (500 mg/24 hours for 3 days), vitamin D supplementation, and, in case of thromboembolic risk, low molecular weight heparin were administered.
Statistical analysis
A descriptive analysis of the data was performed. Qualitative variables were expressed as frequencies and their percentage, while the quantitative ones were expressed as mean and standard deviation (SD). A significance test of the null hypothesis was performed using the Student t test for paired samples of the means (preoperative and postoperative) of the scales used in data collection (EVA, Likert, AOFAS, and SF-36).
Results
A total of 20 women were included in the present study with a mean age of 61.65 ± 10.88 years and a diagnosis of rheumatoid arthritis, with pain and functional impairment in the foot accompanied by deformity to a greater or lesser degree with moderate to severe hallux valgus, claw toes, and metatarsal overload height of the sample was 1.64 ± 0.06 meters and mean weight of the sample was 72.5 ± 10.84 kg, resulting in a mean body mass index of 26.87 ± 3.84.
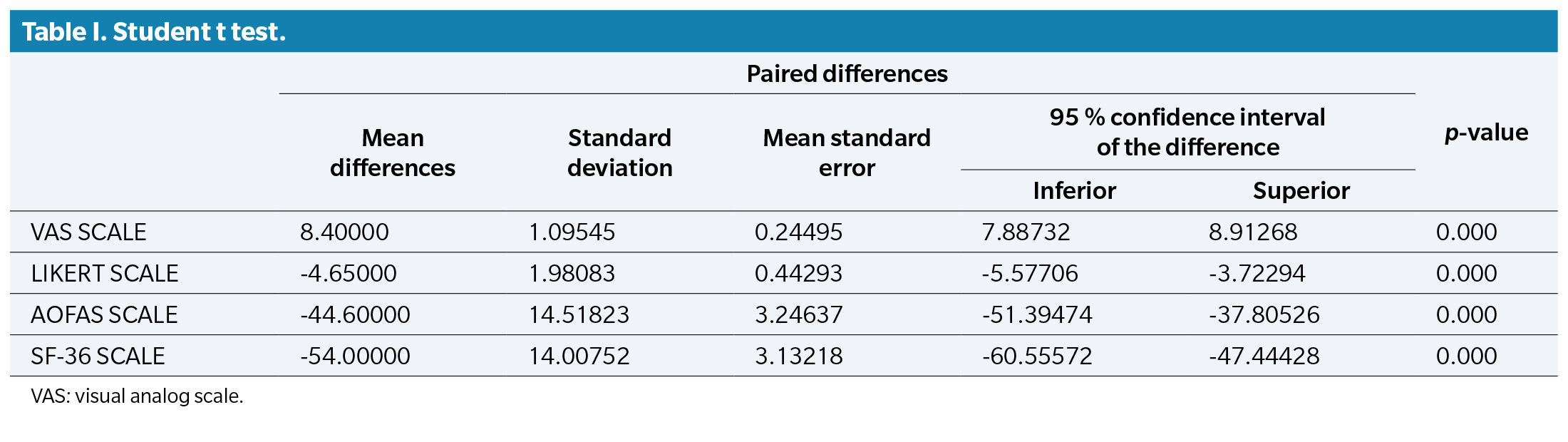
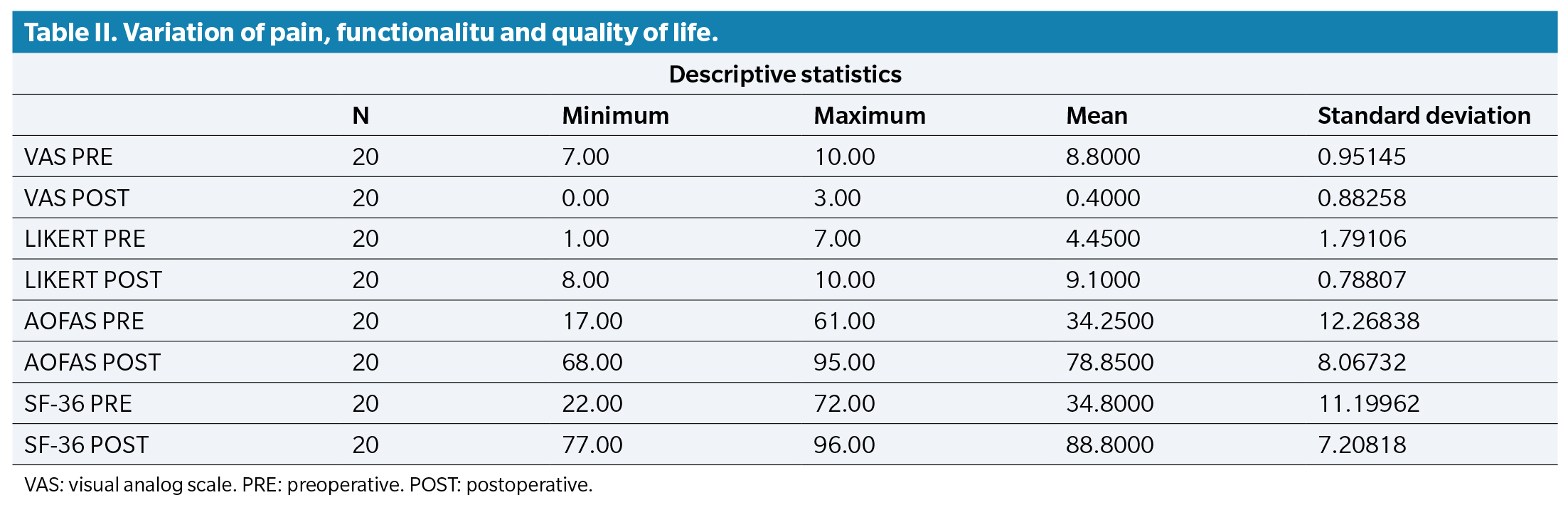
A total of 50 % of the patients had comorbidities such as hypertension, hypothyroidism, or type 2 diabetes mellitus, and a mean score of 8.80 ± 0.95 points on a visual analog scale regarding pain prior to surgery, as well as clinical and radiological signs consistent with joint destruction and deformity. This score decreased to a mean of 0.40 ± 0.88 points 1 year after surgery. Similarly, it was accompanied by a Likert Scale to assess patient satisfaction, obtaining a postoperative mean of 9.10 ± 0.78 points (Table 1. Table 2) illustrates the descriptive statistics of the assessments made.
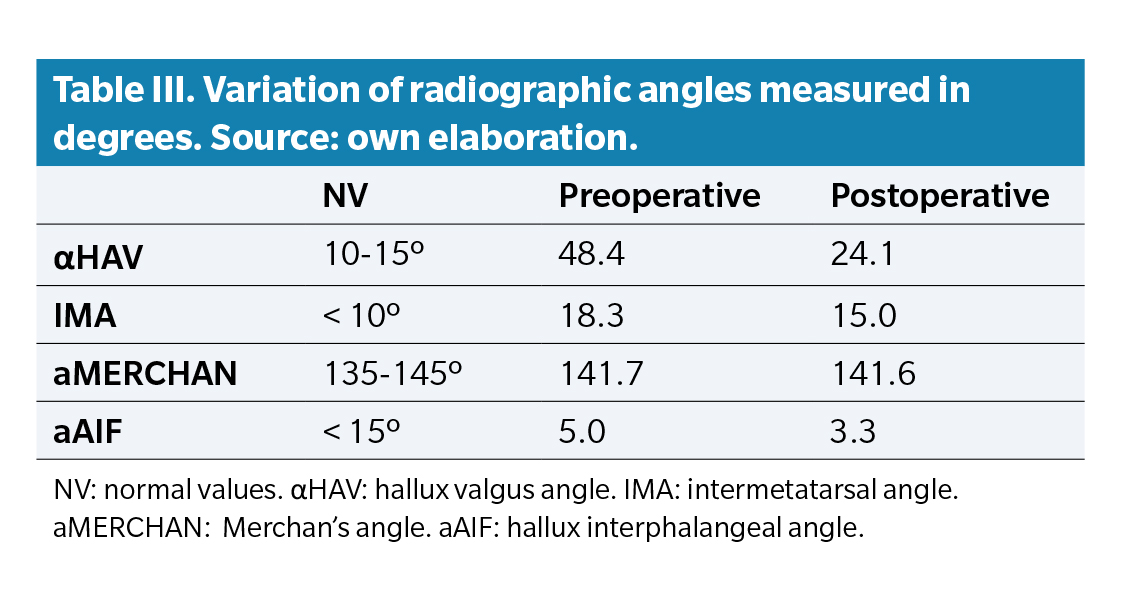
Regarding preoperative radiological angles, a mean of 18.3º was observed for the intermetatarsal I-II angle (IMA I-II) and 48.4º for the hallux abductus valgus angle (αHAV). After the intervention, the mean IMA I-II was 15º and the αHAV was 24.1º. Regarding the Merchan’s angle, mean preoperative and postoperative values of 141.7 and 141.6, respectively, were observed. In the case of the interphalangeal angle, mean preoperative and postoperative values of 5º and 3.3º, respectively, were seen (Table 3).
Discussion
One of the main topics of discussion is the variability of fixations in the fusion of the 1st metatarsophalangeal joint and its indications, as it is spared for cases where there is significant joint destruction. In 2021, Koutsouradis et al.10 reported the effectiveness of the 1st metatarsophalangeal joint fusion in cases of rheumatoid arthritis with severe deformity or first ray disorders with severe signs of joint degeneration, stating that it is a technique that allows pain relief and an increase in the patient’s quality of life. It also confirms the study conducted by Roukis(12) in 2017 that arthrodesis is the treatment of choice in cases of advanced hallux rigidus, rheumatoid arthritis, and revision surgery of the first ray, emphasizing the importance of segment angulation and different forms of fixation, opting in this case for temporary Kirschner wire osteosynthesis.
The fixation using 3 Kirschner wires was first described in 2009 by Mah and Banks(13), who established that this type of fixation is the gold standard because it reduces the risk of complications and allows a good joint fusion. However, there are other fixation systems, such as compression screws or low-profile plates. In 2008, Sharma et al.(14) studied that the choice of fixation depends on the surgeon’s preferences, since results when comparing compression screws and low-profile plates are similar. On the contrary, Hyer et al.(15) established that compression screws are more cost-effective vs low-profile plates and do not change1 clinical results. Other authors, such as Kang and Bridgen(16) report a lower percentage of cases developing pseudarthrosis with the use of plates, although since the analysis did not show any significant differences, they argue the need for trials with larger samples.
Regarding postoperative radiological study, Hoveidaei et al.(17) reported a reduction of the αHAV down to 34.4° and the IMA I-II down to 8.4°. Similarly, they established that the patients’ mean age was 56.3 years, with this type of interventions being more common in women (91.3 %).
Currently, there are few articles analyzing a series of cases of 1st metatarsophalangeal joint arthrodesis and metatarsal pan-resection in rheumatic feet cases. Only Párra-Téllez et al.(18) have analyzed 31 patients operated on using this technique, establishing a mean age of 49.59 years, while our sample establishes 61.3 years. The data they provide on radiological variations are interesting, in which they report a decrease in the αHAV 1 year after intervention of 31.89° and in the IMA I-II of 10.18°. Regarding pain, they show a preoperative mean of 6.24 points and a postoperative mean of 1.65 points at 1 year.
For the analysis of the quality of life of patients with rheumatoid arthritis, generic scales such as the Quality of Life Profile in Chronic Diseases (PECVEC), the SF-36 Questionnaire, or the Nottingham Health Profile (NHP) can be used. However, authors such as Ballina(19) recommend the use of specific questionnaires such as the Arthritis Impact Measurement Scales (AIMS). This questionnaire assesses the physical, social, and psychological dimensions of patients affected by rheumatoid arthritis. Authors such as Zhang et al.(20) analyzed 207 cases, where they report scores < 69.9 points on the SF36 questionnaire and 7.8 points on the RA-QoL. However, authors such as Van Wissen et al.(21) obtained scores of 34.5 on the PROMIS PF-10 scale in 316 patients. In our case, we obtained an initial score of 33.4 on the SF-36 questionnaire, reaching a postoperative mean of 88.80 points at 12 months.
In conclusion, based on the results of the present study, the fusion of the 1st metatarsophalangeal joint along with metatarsal pan-resection is the technique of choice in patients with rheumatic feet presenting with moderate-to-severe hallux valgus and metatarsal overload. This technique is effective in improving foot functionality and significantly reducing painful symptoms.
Conflict of interest
The authors declare no conflicts of interest regarding this paper.
Funding
None.
Authors contribution
Conception and design: AMPR.
Data collection: AMPR, RRR.
Results analysis: AMPR, FJRC.
Creation and redation of initical draft: FLRC.
Final Review: AMRP, RRR, FJRC, MRB.
References
- Osipova D, Janssen R, Martens HA. Rheumatoid arthritis: more than a joint disease. Ned Tijdschr Geneeskd. 2020;164:D4166.
- Figus F, Piga M, Azzolin I, McConnell R, Iagnocco A. Rheumatoid arthritis: extra-articular manifestations and comorbidities. Autoimmun Rev. 2021;20(4):102776. DOI: 10.1016/j.autrev.2021.102776.
- Lin Y, Anzaghe M, Schülke S. Update on the pathomechanism, diagnosis, and treatment options for rheumatoid arthritis. Cells. 2020;9(4):880. DOI: 10.3390/cells9040880.
- Cugno M, Gualtierotti R, Meroni P, Marzano A. Inflammatory joint disorders and neutrophilic dermatoses: a comprehensive review. Clin Rev Allergy Immunol. 2018;54(2):269-81. DOI: 10.1007/s12016-017-8629-0.
- De Cock D, Hyrich K. Malignancy and rheumatoid arthritis: Epidemiology, risk factors and management. Best Pract Res Clin Rheumatol. 2018;32(6):869-86. DOI: 10.1016/j.berh.2019.03.011.
- Littlejohn E, Monrad S. Early diagnosis and treatment of rheumatoid arthritis. Prim Care Clin Off Pract. 2018;45(2):237-55. DOI: 10.1016/j.pop.2018.02.010.
- Kadambande S, Debnath U, Khurana A, Hemmady M, Hariharan K. Rheumatoid forefoot reconstruction: 1st metatarsophalangeal fusion and excision arthroplasty of lesser metatarsal heads. Acta Orthop Belg. 2007;73(1):88.
- Matcham F, Scott I, Rayner L, Hotopf M, Kingsley G, Norton S. The impact of rheumatoid arthritis on quality-of-life assessed using the SF-36: a systematic review and meta-analysis. Semin Arthritis Rheum. 2014;44(2):123-30. DOI: 10.1016/j.semarthrit.2014.05.001.
- Duan X, Yang L, Dai G, Peng X. Rheumatoid forefoot reconstruction with first metatarsophalangeal fusion and arthroplasty of lesser metatarsal heads. Chinese J Reparative Reconstr Surg. 2012;26(4):445-8.
- Koutsouradis P, Stamatis ED, Savvidou OD. Arthrodesis of the first metatarsophalangeal joint: The “when and how”. World J Orthop. 2021;12(7):485-94. DOI: 10.5312/wjo.v12.i7.485.
- Myerson MS, Schon LC, McGuigan FX, Oznur A. Result of arthrodesis of the hallux metatarsophalangeal joint using bone graft for restoration of length. Foot Ankle Int. 2000;21(4):297-306. DOI: 10.1177/107110070002100405.
- Roukis T. First metatarsal-phalangeal joint arthrodesis: primary, revision, and salvage of complications. Clin Podiatr Med Surg. 2017;34(3):301-14. DOI: 10.1016/j.cpm.2017.02.002.
- Mah C, Banks A. Immediate weight bearing following first metatarsophalangeal joint fusion with Kirschner wire fixation. J Foot Ankle Surg 2009;48(1):3-8. DOI: 10.1053/j.jfas.2008.09.005.
- Sharma H, Bhagat S, DeLeeuw J, Denolf F. In vivo comparison of screw versus plate and screw fixation for first metatarsophalangeal arthrodesis: does augmentation of internal compression screw fixation using a semi-tubular plate shorten time to clinical and radiologic fusion of the first metatars. J Foot Ankle Surg 2008;47(1):2-7. DOI: 10.1053/j.jfas.2007.10.006.
- Hyer C, Glover J, Berlet G, Lee T. Cost comparison of crossed screws versus dorsal plate construct for first metatarsophalangeal joint arthrodesis. J Foot Ankle Surg 2008;47(1):13-8. DOI: 10.1053/j.jfas.2007.08.016.
- Kang Y, Bridgen A. First metatarsophalangeal joint arthrodesis/fusion: a systematic review of modern fixation techniques. J Foot Ankle Res. 2022;15(1):1-11. DOI: 10.1186/s13047-022-00540-9.
- Hoveidaei A, Roshanshad A, Vosoughi A. Clinical and radiological outcomes after arthrodesis of the first metatarsophalangeal joint. Int Orthop. 2021;45:711-9. DOI: 10.1007/s00264-020-04807-3.
- Parra-Téllez P, López-Gavito E, Vázquez-Escamilla J. Artrodesis metatarsofalángica del primer dedo y resección artroplástica de la cabeza del segundo al quinto metatarsiano en pie reumático. Acta Ortopédica Mex. 2013;27(2):78-86.
- Ballina-García FJ. Medición de la calidad de vida en la artritis reumatoide. Rev Esp Reumatol. 2002;29(2):56-64.
- Zhang J, Jin Y, Wei H, Yao Z, Zhao J. Cross-sectional study on quality of life and disease activity of rheumatoid arthritis patients. J Peking Univ Heal Sci. 2022;54(6):1086-93.