DOI: http://dx.doi.org/10.20986/revesppod.2023.1663/2023
ORIGINAL
Treatment for plantar fasciitis with biomechanical socks. Preliminary results of a randomized clinical trial
Tratamiento para la fascitis plantar con calcetines biomecánicos. Resultados preliminares de un ensayo clínico aleatorio
Alfonso Martínez Nova1
María de los Reyes Cera Medrano2
Pedro V. Munuera3
1Departamento de Podología. Universidad de Extremadura. Cáceres, España
2Centro Universitario de Plasencia, Cáceres, España
3Departamento de Podología. Universidad de Sevilla, España
Abstract
Introduction: Plantar fasciitis is one of the main reasons in podiatric consultations. There are many treatments for this pathology, among which we highlight, orthopedic, physical and pharmacological treatments. In the market, biomechanical sock models has been discovered that could have a positive effect against the treatment of plantar fasciitis, but no results have yet been obtained. Therefore, the objective of this work was to verify the efficacy of the biomechanical sock in reducing pain or improving foot function people suffering from plantar fasciitis or heel pain.
Patients and methods: The sample consisted of 15 participants, included in an age range between 20 and 71 years. Two random groups were held, one of 8 participants (experimental group, Podoks® socks) and another of 7 participants (control group). The previous Foot Function Index questionnaire was carried out on all participants, and after 15 days of wearing the sock, it was carried out again, noting the subsequent Foot Function Index.
Results: After evaluating the results obtained, differences were found in the previous Foot Function Index, with women presenting a worse clinical state than men. After the 15-day follow-up period, a better score was found in the pain subscale of the Foot Function Index, with the Podoks® group presenting a mean of 28.6 ± 18.0 and the control group 39.4 ± 21.6 (p = 0.043).
Conclusions: Biomechanical socks can be a good alternative for the treatment of plantar fasciitis, as a support to other treatments, since they improve the perceived pain after 15 days. This could be related to the early establishment of the Windlass mechanism, which causes the internal arch of the foot to be more stable, thereby reducing excessive tensile stress on the plantar fascia, plantar ligaments, intrinsic muscles, and plantar flexor musculature.
Keywords: Plantar fasciitis, treatment, functional socks, Foot Function Index.
Resumen
Introducción: La fascitis plantar es uno de los principales motivos de las consultas podológicas. Hay multitud de tratamientos para esta patología, entre los que destacamos tratamiento ortopodológico, físico y farmacológico. Recientemente ha salido al mercado un modelo de calcetín biomecánico que podría tener un efecto positivo frente al tratamiento de la fascitis plantar, pero aún no se han obtenido resultados. Por lo tanto, el objetivo de este trabajo fue comprobar la eficacia en la reducción del dolor y aumento de la función que presenta el calcetín biomecánico en personas que padecen fascitis plantar o dolor en el talón.
Pacientes y métodos: La muestra se compuso de 15 participantes, comprendidos en un rango de edad entre 20 y 71 años. Se realizaron dos grupos al azar: uno de 8 participantes (grupo experimental, calcetín Podoks®) y otro de 7 participantes (grupo control). Se realizó a todos los participantes el cuestionario Foot Function Index previo, y después de los 15 días de la utilización del calcetín se le volvió a realizar, anotando el Foot Function Index posterior.
Resultados: Tras la evaluación de los resultados obtenidos, se encontraron diferencias en el Foot Function Index previo, presentando las mujeres un estado clínico peor que los hombres. Una vez realizado el periodo de 15 días de seguimiento, se encontró una mejor puntuación en la subescala de dolor del Foot Function Index, presentando el grupo Podoks® una media de 28.6 ± 18.0 y el grupo control 39.4 ± 21.6 (p = 0.043).
Conclusiones: Los calcetines biomecánicos pueden ser una buena alternativa para el tratamiento de la fascitis plantar, como apoyo a otros tratamientos, ya que mejoran el dolor percibido a los 15 días. Esto podría ser debido a la instauración temprana del mecanismo de Windlass, lo que provoca que el arco interno del pie sea más estable y reduciendo así un excesivo estrés tensil sobre la fascia plantar, ligamentos plantares, músculos intrínsecos y musculatura flexora plantar.
Palabras clave: Fascitis plantar, tratamiento, calcetines funcionales, Foot Function Index.
Received: 28-07-2023
Accepted: 24-09-2023
Correspondence: Alfonso Martínez Nova
podoalf@unex.es
Introduction
Plantar fasciitis is the inflammation of the band of tissue called the fascia, which originates in the calcaneus arriving to the proximal phalanxes, causing pain in the heel, which increases at the beginning and end of the day(1). It is one of the main reasons for primary care visits and is more common in individuals between 40 and 60 years of age, sometimes even hindering walking ability(2). Typically, plantar fasciitis is caused by stiffness in the calf muscles and Achilles tendon, and its occurrence is also increased when there are biomechanical abnormalities present(2).
There is a wide range of treatments for this condition, among which conservative treatments stand out: a) orthopedic treatment with foot orthoses(3); b) physical therapy involving taping, stretching, or the application of ultrasound, shockwave therapy, iontophoresis, laser, or magnetotherapy(4); and c) pharmacological treatments, such as oral anti-inflammatory drugs(5). If these types of treatments are not effective, infiltrations(6) or surgical treatments such as radiofrequency(7), coblation of the fascia, or total or partial fasciotomy may be considered(8).
Within conservative treatments, as an adjunct to foot orthoses, different types of functional socks with various configurations or equipped with different elements are known to provide beneficial effects for the patient’s health(9). Three-dimensional pieces located on the plantar surface of the forefoot have shown a reduction in plantar pressures during dynamic activities(10,11), with potential benefits for patients with metatarsalgia. There are also socks with tensioning elements that provide the patient with better proprioception balance, as well as a more efficient and comfortable gait, promoting overall stability during walking(12).
Currently, a new model of biomechanical sock is known, which potentially could have a positive impact on the treatment of plantar fasciitis. This sock consists of functional elements in the plantar area, which include: a) a cushioned zone in the heel area to provide extra cushioning in the painful area; b) an additional compression band in the midfoot at the level of the medial arch to provide greater support; c) an extra cushioning zone in the metatarsal heads from 2nd to 5th as a lateral expansion of the forefoot; and d) an individual compartment for the first toe with extra cushioning in its plantar area. These elements are designed to activate the Windlass mechanism early, thus improving the tension in the plantar fascia and, in turn, causing a sensation of pain relief in the sole of the foot, as well as relaxation of the musculature associated with plantar fasciitis(13). These socks have shown their effectiveness in reducing dynamic plantar pressures under the first metatarsal head and the hallux, which provides a promising perspective for their use in patients with fasciitis, as they are a daily-life item that we all or almost all use, easy to put on and take off, accessible to the general public in need, and could complement other existing treatments for plantar fasciitis.
However, although we have data on the reduction of pressure under the first metatarsal head produced by the socks, which in turn may be related to the early activation of the Windlass mechanism, there are no studies that demonstrate this. Therefore, the main objective of this work was to verify the effectiveness of a specific biomechanical sock in reducing painful symptoms and increasing functionality in patients with plantar fasciitis after a period of 15 days of continuous use.
Patients and methods
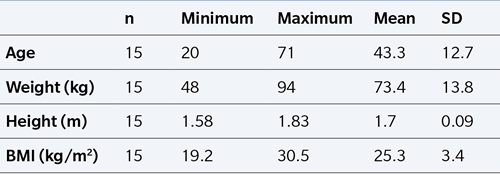
The study consisted of a randomized clinical trial. The sample included 15 participants, comprising 8 males and 7 females, aged between 20 and 71 years (mean age 43.3 ± 12.7 years), with a mean weight of 73.4 ± 13.8 kg, mean height of 1.7 ± 0.09 cm, and a mean body mass index of 25.3 ± 3.4 kg/m2 (Table 1). Participants volunteered and provided informed consent to participate in the study.
Table I. Anthropometric variables of the sample.
The inclusion criteria for participating in the study were as follows: a) having plantar fasciitis with a duration of 3 months or less; b) localized pain at the anteromedial aspect of the heel; c) not undergoing orthopedic, physical, or pharmacological treatment at the time; and d) committing to wearing the socks daily for a period of 15 days. Participants were excluded if: a) they did not adapt to the characteristics of the socks during the 15-day period; b) their pain significantly increased during that time; or c) they did not use the socks daily at the end of the 15 days.
Study protocol
Anthropometric data (gender, age, height in cm, and weight in kg) were collected from each participant. After conducting a physical examination to confirm the presence of plantar fasciitis, the Foot Function Index (FFI) questionnaire was administered to assess pain. The FFI is a tool that provides information about foot function and its impact on daily life. It consists of 23 items divided into three categories: pain (9 items), disability (9 items), and activity limitation (5 items).
Each item in the different categories is scored on a scale of 0 to 10 points. The total score of the questionnaire, as well as the scores for each individual category, can be calculated. The total score can be expressed as a percentage by dividing the total value obtained from all items by 207 and multiplying the result by 100 (Index 1). A higher FFI score indicates a worst clinical state in the participant’s foot, while a lower score indicates better results(14).
Each participant was randomly assigned to either the experimental group (wearing Podoks® biomechanical socks, Fixtoe Device SL, Elda, Spain) or the control group (wearing regular socks with the same design but without biomechanical elements or compression band in the arch). The study was conducted as a double-blind trial, meaning that participants were unaware of their group assignment, thus avoiding potential placebo effects caused by information about the study with the biomechanical socks. The researcher responsible for collecting functional data was also blinded to the study, unaware of the participant’s group assignment. The experimental group consisted of 8 participants, while the control group consisted of 7 participants.
- Group 1 sock (Podoks® sock) is made of Coolmax® tissue (50 % polyester, 35 % polyamide, and 15 % elastane). This sock features various components, including padding and separation for the first toe in a separate compartment from the other toes, forefoot padding from the second to fifth metatarsals, an elastic compression band in the midfoot, and additional cushioning in the heel (Figure 1).
- The sock in group 2 (control sock) is made of Coolmax® tissue (50 % polyester, 35 % polyamide, and 15 % elastane). This sock has a separate compartment for the big toe, similar to the experimental sock, Podoks®, but it does not have the biomechanical elements in the sole (Figure 2). The thickness of the control sock is identical to the experimental sock, Podoks®.
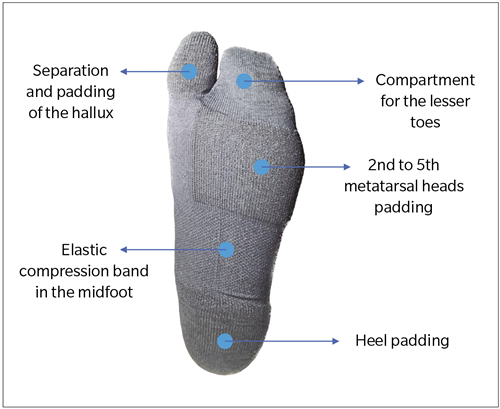
Figure 1. Podoks® sock.
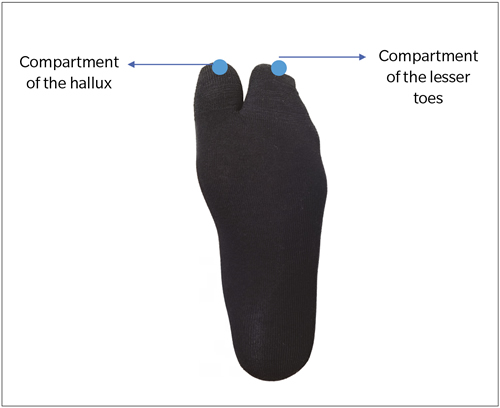
Figure 2. Control socks.
Regardless of the group they belong to, participants should wear the assigned sock for a period of 15 days, wearing it for as long as possible, for this we give patients at least two pairs of socks. It was recommended to put on the sock every morning and wear it throughout the day, while also monitoring any changes in the previously experienced pain (whether it increases, decreases, or remains unchanged).
After the 15-day period, participants are required to return for the final collection of the Foot Function Index questionnaire, affirming that they have used the socks as much as possible during that time.
Statistical analysis
The data analysis was conducted using SPSS version 22.0 software (UEX campus license). The statistical analysis was performed using descriptive statistics and dependent t test (pre-post) and independent samples t-test (gender). A significance level of 5 % (p < 0.05) was established.
Results
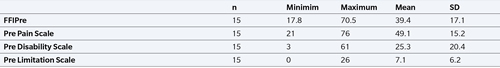
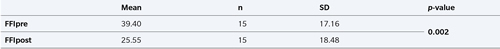
The participants reported an average duration of 36.8 ± 24.6 days experiencing pain caused by plantar fasciitis (range of 7 to 92 days). In the pre-evaluation of the Foot Function Index (FFI), the participants had an average score of 39.40 ± 17.16. The values for the different subscales of the FFI can be seen in Table 2.
When comparing the pre-intervention Foot Function Index (FFI) between the Podoks® group and the Control group, we observed a mean of 39.44 ± 14.5 in the Podoks® group and a mean of 39.36 ± 21.01 in the Control group, with no significant difference observed (p = 0.99).
Table II. Pre FFI and subescales.
Comparing the evolution of the overall group’s Foot Function Index (FFI), we observed a mean FFI score of 39.40 ± 17.16 at the initial assessment, compared to an FFI score of 25.55 ± 18.48 at the 15-day follow-up. The difference between the two time points was statistically significant (p = 0.002) (Table 3).
Table III. Comparison of overall Foot Function Index (FFI) before and after.
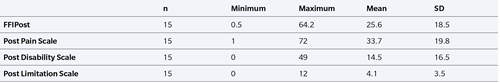
After using the socks in both groups for a period of 15 days and conducting the complete assessment of the post-intervention Foot Function Index (FFI), the study participants had a mean score of 25.6 ± 18.59. Regarding the FFI subscales, we can differentiate the following: 1) post-intervention pain scale with a mean of 33.7 ± 19.8, 2) post-intervention disability scale with a mean of 14.5 ± 16.5, and finally 3) post-intervention limitation scale with a mean of 4.1 ± 3.5 (Table 4).
Table IV. Post-intervention Foot Function Index (FFI) scores with subscales.
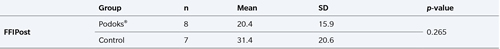
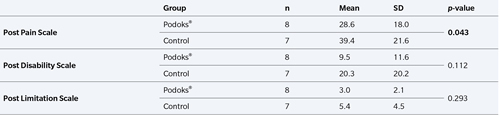
Comparing the post-intervention Foot Function Index (FFI) scores between the Podoks® and Control groups, the Control group had a higher score (31.4 ± 20.6) compared to the Podoks® group (20.4 ± 15.09), but the difference was not statistically significant (p = 0.265) (Table 5).
Table V. Post FFI by group (Podoks® and Control).
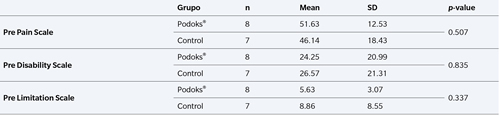
Regarding the differentiation of groups (Podoks® and Control) in the sub-scales of the Foot Function Index (FFI) at baseline, the Podoks® group had a mean score of 51.63 ± 12.53 in the pain scale, while the Control group had a mean score of 46.14 ± 18.43. However, no significant difference was found between the results of both groups (p = 0.507) (Table 6). There were also no significant differences in the disability (p = 0.835) or limitation (p = 0.337) sub-scales at baseline.
Table VI. Pre-treatment FFI Subscales by Group (Podoks® and Control).
In comparison to the post-treatment sub-scales of the FFI, a lower score was observed in the pain scale in the Podoks® group (28.6 ± 18.0) compared to the Control group (39.4 ± 21.6), and this difference was statistically significant (p = 0.043) (Table 7).
Table VII. Post-treatment FFI Subscales by Group (Podoks® and Control).
When evaluating the pre-treatment FFI, women had a higher score (50.5 ± 17.9) compared to men (29.7 ± 9.0), and these results were statistically significant (p = 0.012, Table 8). However, the results were not statistically significant for the number of days of previous pain (p = 0.190) and the post-treatment FFI (p = 0.084) based on gender.
Table VIII. FFI Pre and Post by gender.
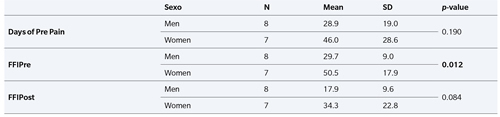
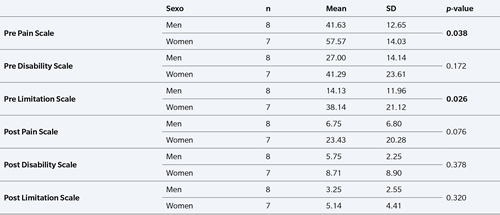
Analyzing the results obtained from the pre- and post-treatment FFI sub-scales by gender, women had a higher score in the pre-treatment pain scale (57.57 ± 14.03) compared to men (41.63 ± 12.65), and this difference was statistically significant (p = 0.038). In the pre-treatment disability scale, women also had a higher score (38.14 ± 21.12) compared to men (14.13 ± 11.96), and this difference was statistically significant as well (p = 0.026). However, no significant results were found in the other scales based on gender (Table 9).
Table IX. FFI Subscales Before and After by Gender (Male and Female).
Discussion
Currently, the use of compression socks or stockings is increasing, serving different therapeutic purposes. They can be used to improve venous return in individuals with blood circulation disorders(15) or to enhance physical performance and accelerate venous return in athletes(16). Therefore, exploring the potential benefits of socks with biomechanical elements is of great clinical and scientific interest.
In our study, both the experimental and control groups consisted of patients with similar clinical conditions (up to 3 months of pain) and a mild to mild/moderate FFI score (39 points in both groups). This score can be compared to those obtained in other studies investigating different treatments, where starting scores were much higher (around 70 points), indicating that our patients had a milder clinical condition(17). This difference could be related to the fact that our patients had a maximum of 3 months of clinical progression and did not exhibit high pain values. Since both groups started with the same FFI score, no biases can be attributed to the group assignment and their potential progress with the use of socks.
In the overall sample, an improvement in clinical status has been observed, with a significant reduction of up to 14 points in the FFI. This improvement could be attributed to the use of biomechanical socks, as this group showed the most significant differences in the FFI, especially in the pain scale (Table 5). This clinical improvement can be compared to other devices or taping methods, such as the Low Dye Type, that achieves reducing the pain associated with plantar fasciitis within a short period of 1 week of use(18). The main advantage lies in the fact that the reduction experienced by our patients in a similar timeframe is achieved with the use of daily clothing, which is accessible in terms of cost, does not require professional application, is not an external device, is comfortable to wear for long durations (> 8 hours per day), and does not lose its effectiveness with use.
While some studies do not find differences in the prevalence of plantar fasciitis or its clinical impact based on gender(19), in our study, women initially reported higher levels of pain. Therefore, the use of the socks also benefited women to a greater extent, resulting in a more positive outcome for them in both the pain and disability subscales. As a future research direction, we propose to explore this gender perspective in relation to the higher pain experienced by women.
Based on the evaluation of the results and the improvement observed in the post-treatment foot function index compared to the pre-treatment scores without distinguishing between groups, we can conclude that the biomechanical socks can be used as a treatment for plantar fasciitis, as they yield short-term improvement. This treatment can be compared to taping for plantar fasciitis, which is a functional taping technique that has shown promising results. And this is achieved with plantar biomechanical elements specific to the sock, which primarily generate kinetic changes during the second rocker of gait and consequently alter or improve the amount of stress developed and borne by the tissues of the plantar surface of the foot(20,21). During the third rocker, the plantar padding of the hallux, combined with the padding from the second to fifth metatarsal, tends to enhance the activation of the windlass mechanism due to the new rotational balance around the axis of rotation of the first metatarsophalangeal joint(20).
The results achieved with the use of biomechanical socks can also be compared to the use of night splints for the treatment of plantar fasciitis, as night splints may improve pain, especially in the morning, after using them for a period of 12 weeks. However, the improvement starts to be noticeable around the fourth week of use(22). In comparison to another study using custom insoles as treatment, after a 3-month follow-up, the FFI score reduced from 67 to 39 points(17). Similar to our study, this suggests that the use of biomechanical socks could improve the painful symptoms of plantar fasciitis. However, it eliminates the need for personalized orthopedic treatment, as the socks serve as a substitute.
Biomechanical socks could be an alternative to the use of night splints, as they are easier to use, more comfortable, and can be worn throughout the day as they are not exclusively for nighttime use. They are used during dynamic activities. Additionally, they can also be a good complementary treatment option for patients who already use custom insoles or similar treatments for clinical conditions. This includes patients who experience functional hallux limitus, a sensation of an open foot, or dorsal tarsal compression syndromes. Biomechanical socks can serve as a therapeutic complement to foot orthoses.
Our study has limitations, primarily due to the small sample size. A larger sample would be needed to provide more robust evidence of the effects in patients. Another limitation is the short follow-up period of only 15 days and the difference of age in our group. A longer-term follow-up could provide valuable insights into the use of biomechanical socks as a standalone or complementary treatment.
In conclusion, based on the results, based on the results, we can conclude that the use of biomechanical socks is beneficial in reducing pain associated with plantar fasciitis. This pain reduction could be related with the relaxation of plantar structures through the early activation of the Windlass mechanism. However, this improvement in pain does not appear to have a positive impact on disability level or activity limitation, as patients were performing the same activities as before within 15 days.
Ethical statement
Conducted under the approval of the Bioethics and Biosafety Committee of the University of Extremadura (ID: 19_2023).
Conflict of interests
Fixtoe Device SL, manufacturer of Podoks® socks, has provided the experimental and control socks to the authors. The second author (AMN) serves as a scientific advisor in the development of socks for Fixtoe Device SL, being established an economic link between the company and this author.
Funding
Fixtoe Device SL gave the experimental and control socks to the authors. No other finantial support was carried out.
Supplementary Information
Supplementary material contains the Foot Function Index used in the study. Foot Function Index:
Authors’ contribution
Conception and design of the study: A. M. N.
Creation, drafting and preparation of the initial outline of the work: M. R. C. M.
Data collection: M. R. C. M., P. V. M.
Final revision (critical review and comments) and final acceptance: A. M. N., P. V. M.
References
- Morrissey D, Cotchett M, Said J’bari A, Prior T, Griffiths IB, Rathleff MS, et al. Management of plantar heel pain: a best practice guide informed by a systematic review, expert clinical reasoning and patient values. Br J Sports Med. 2021;55(19):1106-18. DOI: 10.1136/bjsports-2019-101970.
- Siriphorn A, Eksakulkla S. Calf stretching and plantar fascia-specific stretching for plantar fasciitis: A systematic review and meta-analysis. J Bodyw Mov Ther. 2020;24(4):222-32. DOI: 10.1016/j.jbmt.2020.06.013.
- Xu R, Wang Z, Ma T, Ren Z, Jin H. Effect of 3D Printing Individualized Ankle-Foot Orthosis on Plantar Biomechanics and Pain in Patients with Plantar Fasciitis: A Randomized Controlled Trial. Med Sci Monit. 2019;25:1392-400. DOI: 10.12659/MSM.915045.
- Li X, Zhang L, Gu S, Sun J, Qin Z, Yue J, et al. Comparative effectiveness of extracorporeal shock wave, ultrasound, low-level laser therapy, noninvasive interactive neurostimulation, and pulsed radiofrequency treatment for treating plantar fasciitis: A systematic review and network meta-analysis. Medicine. 2018;97(43):e12819. DOI: 10.1097/MD.0000000000012819.
- Akram MR, Yousaf MN, Waseem M, Chaudhary FS. Comparison of mean pain score of oral non-steroidal anti-inflammatory agents and locally injectable steroid for the treatment of plantar fasciitis. J Pak Med Assoc. 2022;72(2):231-5. DOI: 10.47391/JPMA.1029.
- López AMD, Carrasco PG. Efectividad de distintas terapias físicas en el tratamiento conservador de la fascitis plantar: revisión sistemática. Rev Esp Salud Publica. 2014;88(1):157-78. DOI: 10.4321/S1135-57272014000100010.
- Caicedo Gutiérrez L, Moreno Martínez D. Reporte de caso: radiofrecuencia de nervio de Baxter en paciente con fascitis plantar refractaria a manejo convencional. Rev Esp Anestesiol Reanim. 2022;69(5):306-9. DOI: 10.1016/j.redar.2021.02.003.
- Iglesias M, Sperone E, Macklin Vadell A, Bigatti A. Fascitis plantar: análisis de opciones terapéuticas. Rev Asoc Argent Ortop Traumatol. 2022;87(3):413-21. DOI: 10.15417/issn.1852-7434.2022.87.3.1359.
- Zwaard B. Foot Function Index. In: Encyclopedia of Quality of Life and Well-Being Research. Springer Netherlands; 2014. p. 2328-30.
- Caracuel López JM, Sánchez Rodríguez R, Gómez-Martín B, Escamilla-Martínez E, Martínez Nova A, Jiménez Cano VM. Reducción de las presiones plantares dinámicas en un calcetín experimental. Un estudio preliminar. Rev Esp Podol. 2021;32(2):86-92. DOI: 10.20986/revesppod.2021.1619/2021. DOI: 10.20986/revesppod.2021.1619/2021.
- Jiménez-Cano V, Martínez-Nova A, Caracuel-López JM, Escamilla-Martínez E, Gómez-Martín B, Sánchez-Roríguez R. Socks with an U-shaped 3D discharge element are capable to reduce dynamic plantar pressures under the central forefoot. J Tissue Viability. 2022;31(2):309-14. DOI: 10.1016/j.jtv.2021.11.005.
- Gormaz López G, Painagua Muñoz L, Martínez Nova A. Efectos en el equilibrio y confort de un calcetín estabilizador en pacientes con diferentes alteraciones neurológicas. Rev Esp Podol. 2020;31(1):38-45. DOI: 10.20986/revesppod.2020.1566/2020.
- Martínez Nova A, González-Alonso A, Fernández-Miranda Gastón M, Morán Cortés JF. Reducción de presiones plantares dinámicas en el antepié plantar medial con calcetines biomecánicos. Rev Esp Podol. 2022;33(2):110-4. DOI: 10.20986/revesppod.2022.1646/2022.
- Budiman-Mak E, Conrad KJ, Roach KE. The Foot Function Index: a measure of foot pain and disability. J Clin Epidemiol. 1991;44(6):561-70. DOI: 10.1016/0895-4356(91)90220-4.
- Azcona L. Insuficiencia venosa. Prevención y tratamiento. Farmacia Profesional. 2008;22(10):36-40.
- Zaleski AL, Pescatello LS, Ballard KD, Panza GA, Adams W, Hosokawa Y, et al. The Influence of Compression Socks During a Marathon on Exercise-Associated Muscle Damage. J Sport Rehabil. 2019;28(7):724-8. DOI: 10.1123/jsr.2018-0060.
- Longo G, Denaro V, Ribeiro AP, Maria S, João A. The Effect of Short and Long-Term Therapeutic Treatment with Insoles and Shoes on Pain, Function, and Plantar Load Parameters of Women with Plantar Fasciitis: A Randomized Controlled Trial. Medicina (Kaunas). 2022;58(11):1546. DOI: 10.3390/medicina58111546.
- Castro-Méndez A, Palomo-Toucedo IC, Pabón-Carrasco M, Ortiz-Romero M, Fernández-Seguín LM. The Short-Term Effect of Dynamic Tape versus the Low-Dye Taping Technique in Plantar Fasciitis: A Randomized Clinical Trial. Int J Environ Res Public Health. 2022;19(24):16536. DOI: 10.3390/ijerph192416536.
- García Vidal JA, Baño Alcaraz A, Sánchez Martínez MP, Belmonte Albaladejo A, Martín San Agustín R. Relación entre el sexo, edad e índice de masa corporal y el Foot Function Index en pacientes con fascitis plantar. Rev Int Ciencias Podol. 2019;13(1):33-40. DOI: 10.5209/RICP.62342. DOI: 10.5209/RICP.62342.
- Harutaichun P, Vongsirinavarat M, Pakpakorn P, Sathianpantarit P, Richards J. Can orthotic wedges change the lower-extremity and multi-segment foot kinematics during gait in people with plantar fasciitis? Gait Posture. 2022;97:174-83.
- Kogler GF, Veer FB, Solomonidis SE, Paul JP. The influence of medial and lateral placement of orthotic wedges on loading of the plantar aponeurosis. J Bone Joint Surg Am. 1999;81(10):1403-13. DOI: 10.2106/00004623-199910000-00005.
- Lim AT, How How C, Tan B. What is plantar fasciitis? Management of plantar fasciitis in the outpatient setting. Singapore Med J. 2016;57(4):168-71. DOI: 10.11622/smedj.2016069.
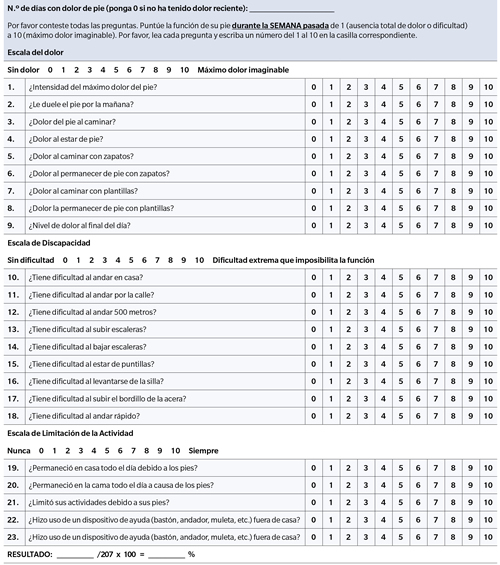
Index 1. Foot Function (FFI) Index.