DOI: http://dx.doi.org/10.20986/revesppod.2024.1694/2024
ORIGINAL
Association between degenerative changes of the first metatarsophalangeal joint with goniometric variables of the internal longitudinal arch: observational study
Asociación entre cambios degenerativos de la primera articulación metatarsofalángica con la alteración de las variables goniométricas del arco longitudinal interno: estudio observacional
Raquel Sánchez Sánchez1
Marta Nieto Cordero1
Raquel de la Cruz Moreno1
Raúl Molines Barrosos1
Ángel Manuel Orejana García1
Óscar Madruga Armada1
1Servicio de Patología y Ortopedia. Clínica Universitaria de Podología, Universidad Complutense de Madrid, España
Abstract
Introduction: Radiographically, an association has been shown between hallux rigidus and tMetatarsus Primus Elevatus. The objective of this article is to assess the association between degenerative changes of the first metatarsophalangeal joint with goniometric values of the internal longitudinal arch.
Patients and methods: Observational study on patients of the University Podiatry Clinic (UCM) from September 2022 to March 2023 who presented reduced mobility of first metatarsophalangeal joint of less than 60° in nonweightbearing. From a weight bearing lateral x-ray it was analyzed: joint space alteration, dorsal osteophytosis in proximal phalanx and in first metatarsal. inclination angle of first metatarsal, inclination angle of calcaneus, Meary-Tomeno line and internal Costa Bartani angle.
Results: 37 feet (37 patients) were analyzed with a mean age of 52 years (64.9 % women, 35.1 % men). Decreased joint space was associated with more plantar Meary-Tomeno line (8.4° ± 5.6 vs. 1.1° ± 5.4; p < 0.001), less calcaneal inclination (21.4° ± 4.8 vs. 25.5° ± 6.4; p = 0,032) and less inclination of first metatarsal (21.5° ± 2.5 vs. 23.8° ± 3.3; p = 0.018). Patients who presented dorsal osteophytosis of proximal phalanx had a lower calcaneal inclination (19.8° ± 4.4 vs. 24.5° ± 1.3; p = 0.021). Patients with any signs of hallux rigidus showed a Meary-Tomenon line with a more plantar apex (7.0° ± 7.0 vs. 2.7° ± 5.1; p = 0.041).
Conclusions: Goniometric measurements representing values compatible with flattening of the internal longitudinal arch are associated with signs of joint degeneration of the first metatarsophalangeal joint.
Key words: Hallux rigidus, internal longitudinal arch, radiography
Resumen
Introducción: Radiográficamente se ha demostrado una asociación entre el hallux rigidus y la presencia de metatarsus primus elevatus. El objetivo de este trabajo es valorar la asociación entre los cambios degenerativos de la primera articulación metatarsofalángica (1AMTF) con valores goniométricos del arco longitudinal interno.
Pacientes y métodos: Estudio observacional sobre pacientes de la Clínica Universitaria de Podología (UCM), de septiembre 2022 a marzo 2023, con una movilidad 1AMTF inferior a 60° en descarga. En radiografía lateral en carga se analizaron: alteración del espacio articular, osteofitosis dorsal en falange proximal y en cabeza del primer metatarsiano, ángulo inclinación de primer metatarsiano, ángulo inclinación de calcáneo, línea Meary-Tomeno y ángulo Costa Bartani interno.
Resultados: Se analizaron 37 pies (37 pacientes) con edad media de 52 (64.9 % mujeres y 35.1 % hombres). La disminución del espacio articular se asoció con línea Meary-Tomeno más plantar (8.4° ± 5.6 vs. 1.1° ± 5.4; p < 0.001), menor inclinación del calcáneo (21.4° ± 4.8 vs. 25.5° ± 6.4; p = 0.032) y menor inclinación del primer metatarsiano (21.5° ± 2.5 vs. 23.8° ± 3.3; p = 0.018). Pacientes con osteofitosis dorsal en falange proximal tuvieron menor ángulo de inclinación del calcáneo (19.8° ± 4.4 vs. 24.5° ± 1.3; p-valor = 0.021). Los pacientes con algún signo de hallux rígidos (n = 22; 60 %) mostraron una línea Meary-Tomenon con un vértice más plantar (7.0° ± 7.0 vs. 2.7° ± 5.1; p = 0.041).
Conclusiones: Las medidas goniométricas que representan valores compatibles con aplanamiento del arco longitudinal interno se asocian con signos de degeneración articular de la primera articulación metatarsofalángica.
Palabras clave: Hallux rigidus, arco longitudinal interno, radiografía
Correspondence: Raquel Sánchez Sánchez
address: raqsan09@ucm.es
Received: 04-15-2024
Accepted: 05-27-2024
Introduction
The term hallux rigidus (HR) refers to degenerative arthritis, or osteoarthritis, of the first metatarsophalangeal joint (1MTPJ). It presents with painful limitation to dorsiflexion of this joint, which is crucial dynamically as it bears approximately 119 % of body weight during the gait cycle(1).. HR is the second most common pathology of the 1MTPJ, surpassed only by Hallux Abductus Valgus. It is estimated that HR affects 2.5 % of the population over 50 years old and is less common in adolescence, in this latter case as an evolution of an osteochondral injury. Additionally, it has been observed that females are twice as likely as males to develop HR(2).
A weak association has been found in the literature between HR and some risk factors based on clinical findings, such as a history of trauma, or deformities like Hallux Abductus Valgus, Hallux Abductus Interphalangeus, alteration in the length of the first metatarsal or the proximal phalanx of the hallux. Radiographically, a significant association has been demonstrated between HR and the presence of Metatarsus Primus Elevatus (MPE) (3).
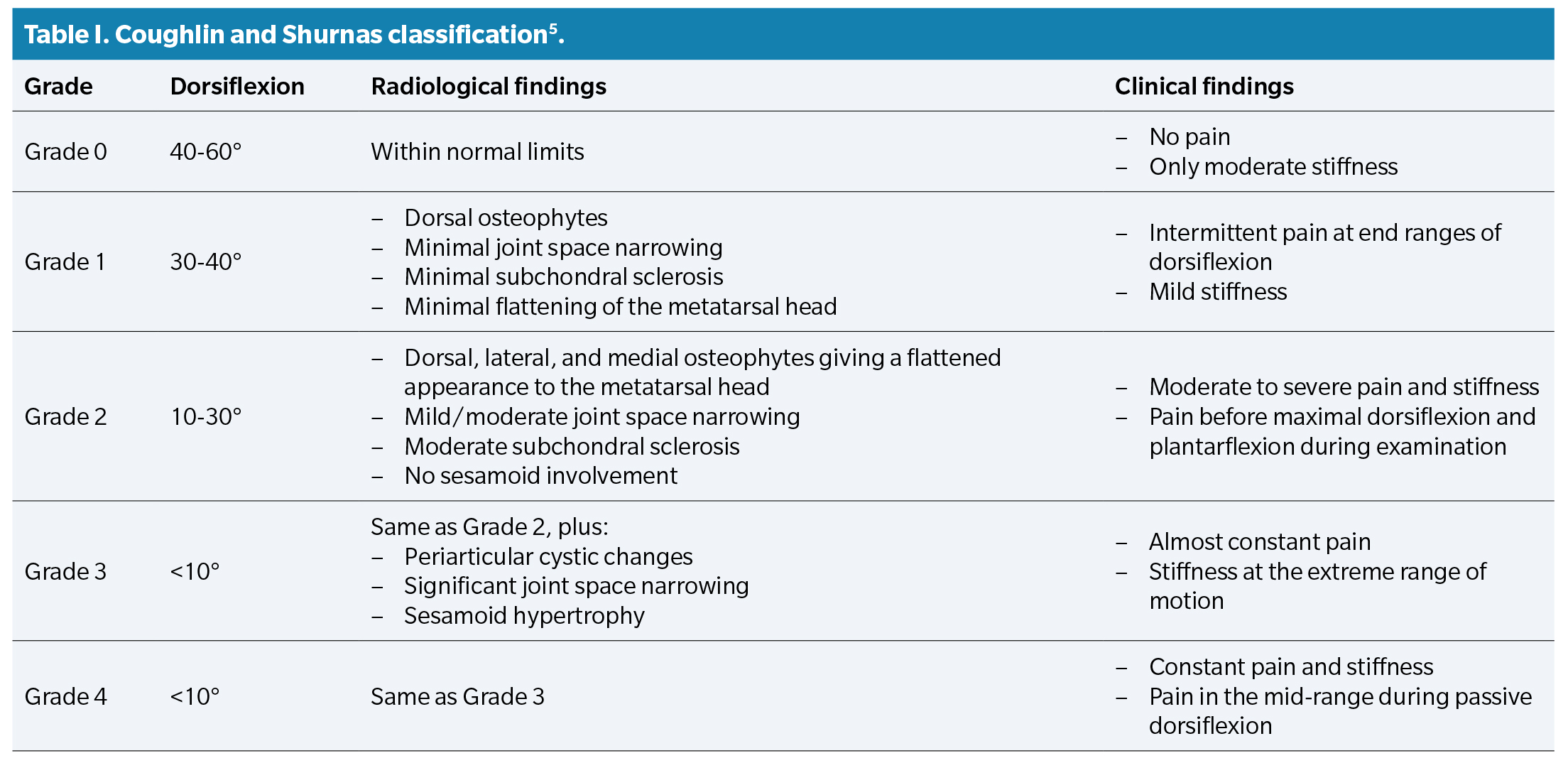
On the other hand, the diagnosis of HR disease is based on clinical and radiological findings. The most common clinical findings in the diagnosis of HR are pain and limited joint mobility of the 1MTPJ, and the radiological findings include the formation of dorsal osteophytes on the head of the first metatarsal, presence of cysts and subchondral geodes, existence of subchondral sclerosis, involvement of the joint space, sesamoid disorders (including avascular necrosis), or bone lesions following trauma(4).. Based on the results of reliability and validity studies, the literature recommends using the Coughlin and Shurnas classification as the gold standard for the diagnosis and classification of HR(2,5) (Table 1).
The term hallux limitus is used interchangeably with hallux rigidus in the literature to refer to the painful deformity in the sagittal plane of the 1MTPJ. Dananberg(6) described the term functional hallux limitus as the entity in which the range of motion of the 1MTPJ is free in non-weight bearing conditions, while the range of dorsiflexion of the hallux is limited during weight-bearing activities, in the absence of radiological structural changes. This entity would be equivalent to the initial stages of the hallux rigidus classification proposed by Coughlin and Shurnas.
Excessive pronation of the rearfoot, commonly observed in the routine clinical practice, has been suggested as one of the main causes of functional hallux limitus(7). It has been theorized that increased pronation in a closed kinetic chain produces an increase in tension in plantar aponeurosis(8).. Fuller suggested that excessive tension in the plantar fascia, as can be the case in a situation of maximum pronation, can counteract the dorsiflexor moment that the hallux supports at the beginning of the propulsive phase, thus preventing the proper establishment of the Windlass mechanism and, therefore, preventing the dorsiflexion of the hallux(9). This inadequate dorsiflexion of the proximal phalanx results in a restriction of dorsiflexion mobility of the 1MTPJ, repetitive microtraumas, and proliferation of marginal joints, leading to hallux rigidus. Harradine and Bevan(7) showed through static measurements of the patient that the maximum range of dorsiflexion of the hallux decreases with increased rearfoot eversion. For this, they used external elements such as rearfoot wedges to increase the eversion of the calcaneus and therefore the pronation of the rearfoot. However, we have not found studies that analyze the association between the presence of HR and the position of the foot, measured by differences in the radiographic angles of the internal arch.
Given that currently no studies have been conducted that associate radiological variables compatible with pronation and the development of degenerative processes in the 1MTPJ, the main objective of this study was to assess the association between degenerative changes of the 1MTPJ and the goniometric values of the internal longitudinal arch in the sagittal plane.
Patients and methods
Study type and sample size
We conducted an observational study on a sample of 37 feet corresponding to 37 patients who visited the Pathology and Orthopedics service of the University Podiatry Clinic of Universidad Complutense de Madrid, Madrid, Spain during the period from September 2022 through March 2023. In individuals who showed bilateral HR symptoms, only the foot with the most severe symptoms was included in the study.
Inclusion criteria
The inclusion criteria for the study population were established as the presence of a maximum dorsiflexion (DF) mobility of the 1MTPJ of < 60° in non-weight-bearing conditions or a loss of ≥ 10 % of the degree of motion of the 1MTPJ vs the contralateral limb, and the patient’s ability to walk distances > 50 meters without the aid of walking support devices such as crutches or walkers.
Pregnant patients, those with a history of surgery localized to the 1MTPJ or other osteoarticular structures of the internal column, a history of diabetes mellitus, rheumatic diseases such as psoriatic arthritis, rheumatoid arthritis, and gouty arthritis, and/or having received a corticosteroid or hyaluronic acid injection in the 12 weeks prior to data collection were excluded.
Data mining
All patients included in the study underwent a weight-bearing lateral X-ray of the included foot. The following radiographic variables related to the presence of hallux rigidus according to the Coughlin and Shurnas classification were analyzed: alteration of the joint space (decrease or absence), dorsal osteophytosis in the proximal phalanx, and in the head of the first metatarsal. Additionally, the following clinical variables were recorded: joint stiffness (mild/moderate/severe), pain (with movement/intermittent/almost constant/constant), and the maximum DF range of the 1MTPJ, following the protocol developed by López del Amo et al. (10) in which joint examination of the 1MTPJ in non-weight-bearing conditions is described. This involves placing the patient in a supine position on the examination table in a relaxed state, placing the goniometer fulcrum at the center of the head of the first metatarsal, the proximal arm parallel to the shaft of the first metatarsal, and the distal or movable arm parallel to the shaft of the proximal phalanx, moving the toe to its maximum extension.
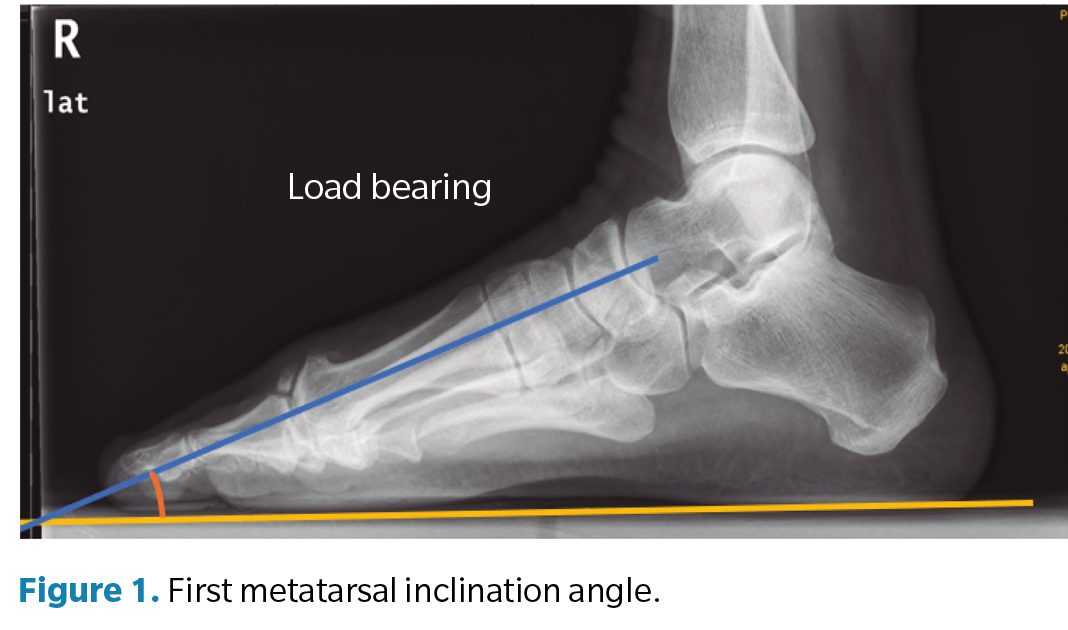
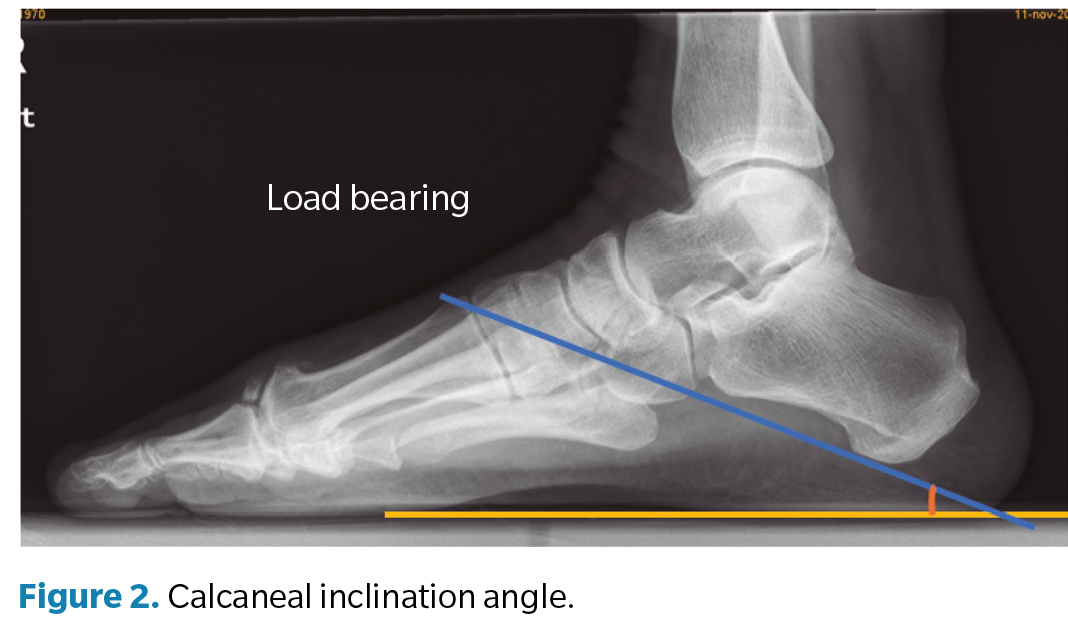
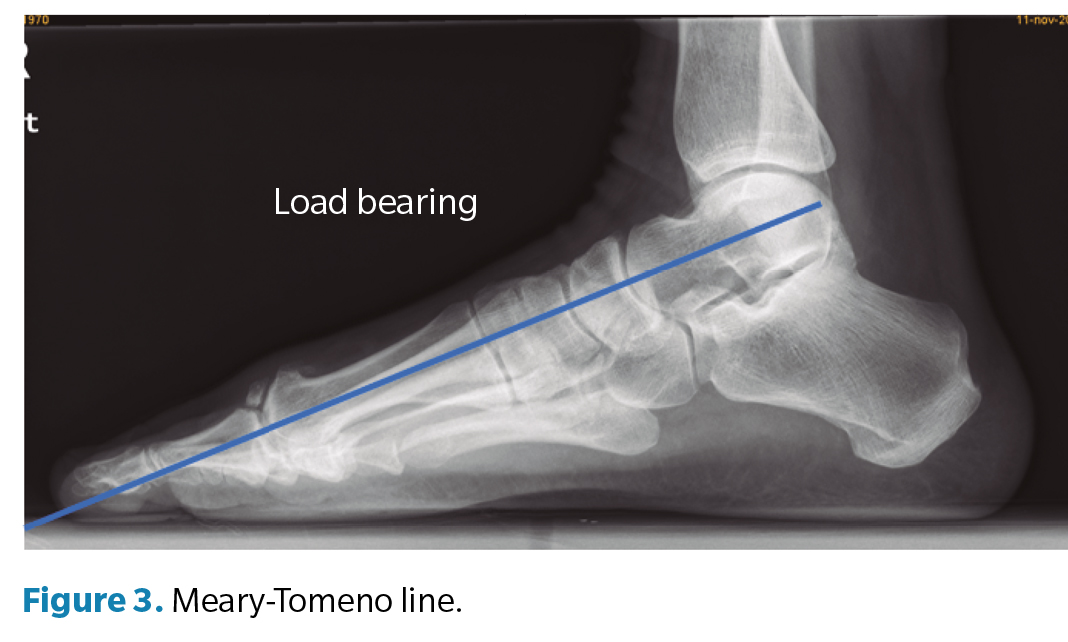
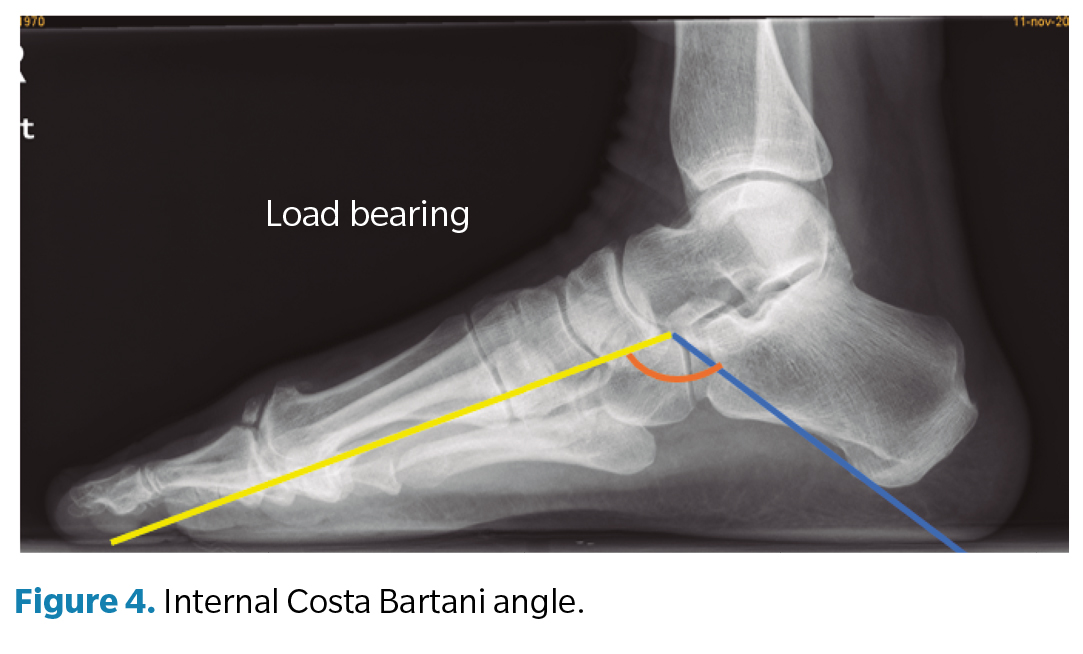
Regarding the goniometric variables in the lateral X-ray, the following angles were obtained: first metatarsal inclination angle, calcaneal inclination angle, Meary-Tomeno line, and internal Costa Bartani angle. The metatarsal inclination angle or Fick angle involves the inclination of the 5 metatarsals; however, for this study, only the inclination angle of the first metatarsal was considered (Figure 1), which was defined by the diaphyseal axis of the first metatarsal with the horizontal plane of the ground support11. The calcaneal inclination angle (Figure 2) is defined by the axis of the calcaneus, a line connecting the calcaneal tuberosity to the plantar margin of the anterior extension of the calcaneus near the calcaneocuboid joint, and the support plane (line formed by the proximal plantar tuberosity of the calcaneus and the head of the 5th metatarsal). A value of 20° is considered normal(12). The Meary-Tomeno line (Figure 3) is defined as the line passing through the axis of the talus (bisector of the angle formed by the tangent to the superior and inferior borders of the talus) and the axis of the diaphysis of the first metatarsal13). The internal Costa Bartani angle (Figure 4) is defined as the union of 3 points: the lowest point of the medial sesamoid, the lowest point of the posterior tuberosity of the calcaneus, and the lowest point of the talonavicular joint(14)..
These angles were chosen because they best represent the alignment of the internal longitudinal arch, in which the decrease or inclination towards the plantar side is associated with flattening of the arch(15).
An initial training session was conducted among the research group for the evaluation of goniometric measurements. Subsequently, the signs and radiographic angles were evaluated by two podiatrists blinded to each other’s results using the Kodak POC 360 quality control software for measurements; both researchers performed 3 measurements of the radiographic angles to minimize bias, with the mean of the measurements being taken as the valid measurement.
Main study variable
The main variable of the study was the presence of HR defined as the existence of grade 0 or higher in the Coughlin and Shurnas classification². Additionally, to determine the study’s objective, each of the degenerative changes of the 1MTPJ in the classification was individually evaluated.
Statistical analysis
Statistical analysis was performed using SPSS for MacOS version 25.0 (SPSS, Inc. Chicago, IL, United States). Qualitative variables were expressed as frequency and percentage, and quantitative variables as mean and standard deviation. The Kolmogorov-Smirnov test was used to determine the normality of the sample. To determine the goniometric variables that best related to clinical signs and degenerative changes of the 1MTPJ a contrast hypothesis test was carried out by means of the t-test that was used for parametric samples and the Wilcoxon-Mann-Whitney U test for non-parametric samples. A p value < 0.05 was considered statistically significant.
Results
A total of 37 feet out of 37 patients (n = 37) with a mean age of 52 (± 17.1) years were included, 64.9 % of whom were women (n = 24) and 35.1 % men (n = 13), with a mean BMI of 26 (± 4.8) kg/m², 38 % of which (n = 14) experienced pain. A total of 40.5 % (n = 15) of the entire sample belonged to stage 0 according to the classification described by Coughlin and Shurnas, 32.4 % (n = 12) to stage 1, 18.9 % (n = 7) to stage 2, and 8.1 % (n = 3) to stage 3. No patient met the clinical and radiological criteria consistent with stage 4.
Patients with dorsal osteophytosis of the proximal phalanx (n = 11; 30 %) had a smaller calcaneal inclination angle than those without osteophytosis (19.8° ± 4.4 vs. 24.5° ± 1.3; p = 0.021; CI [0.753 to 8.747]) (Table 2).
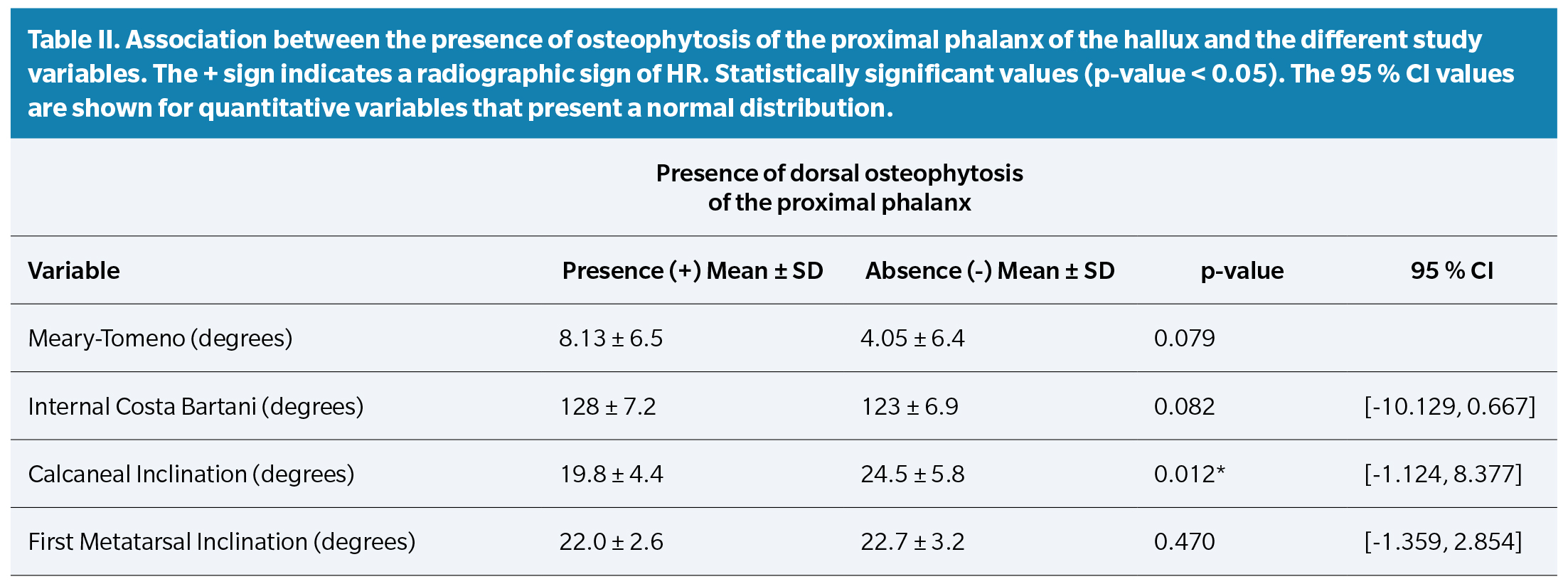
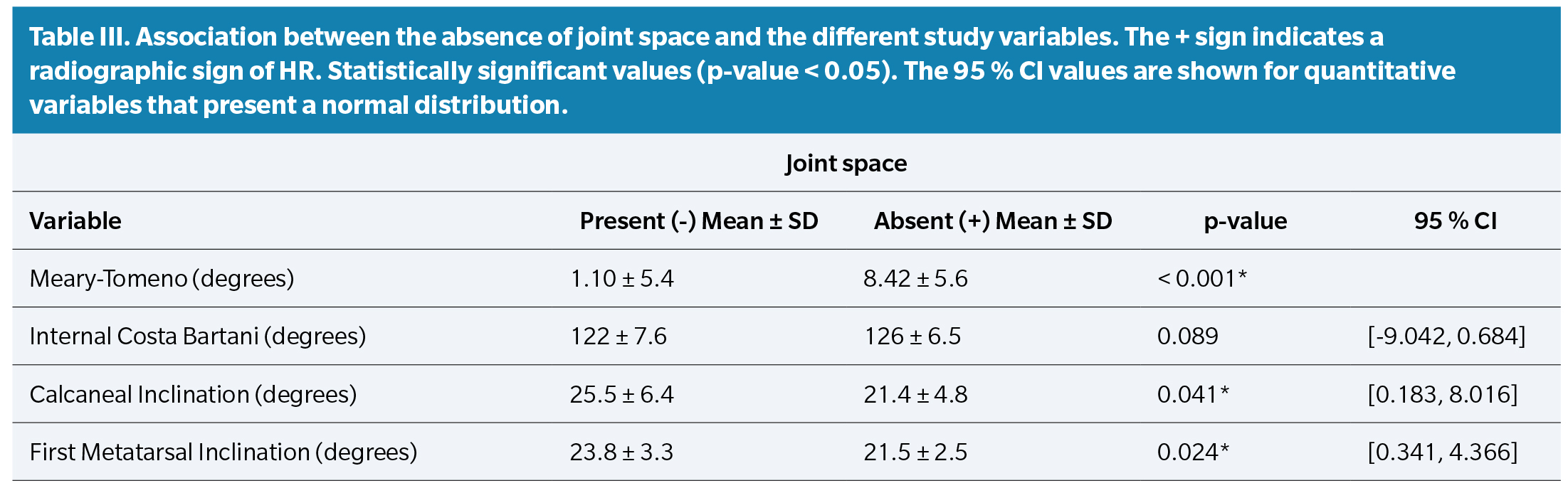
The presence of joint space narrowing was associated with patients with a more plantar-vertex Meary-Tomeno angle (8.4° ± 5.6 vs. 1.1° ± 5.4), a smaller calcaneal inclination (21.4° ± 4.8 vs. 25.5° ± 6.4), and a smaller first metatarsal inclination (21.5° ± 2.5 vs. 23.8° ± 3.3) (p < 0.05) (Table 3).
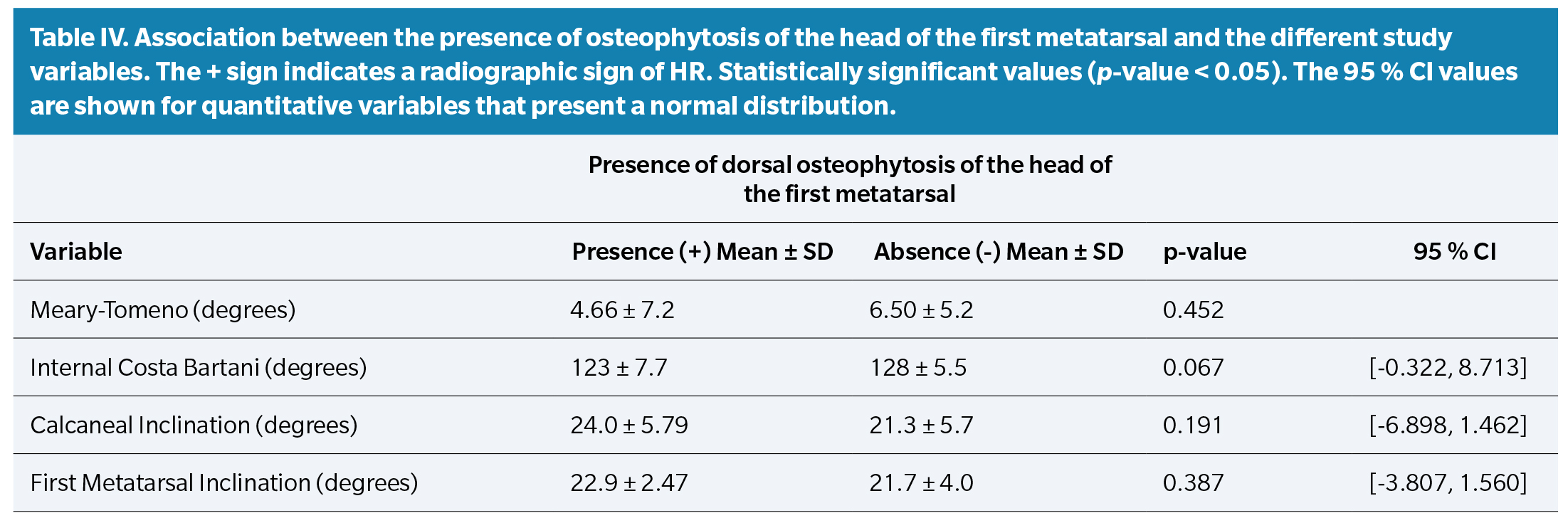
No significant associations were found between the goniometric variables and patients with dorsal osteophytosis of the first metatarsal head (Table 4).
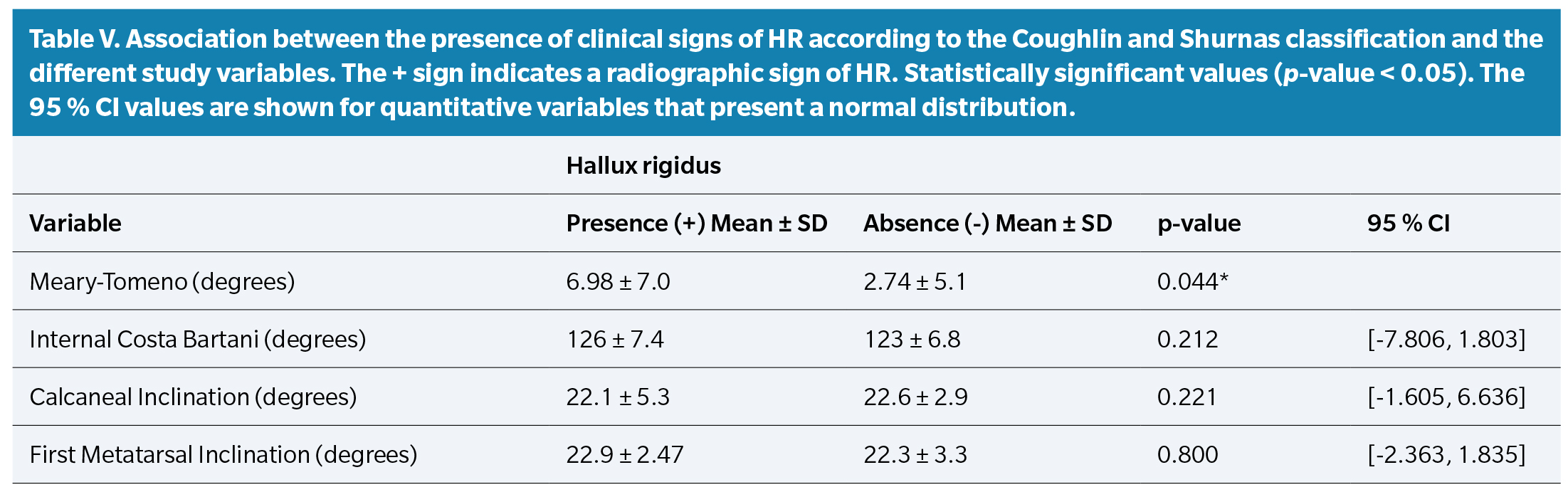
Finally, based on the Coughlin and Shurnas classification, patients with any sign of hallux rigidus (n = 22; 60 %) showed a more plantar-vertex Meary-Tomeno line than those without signs of hallux rigidus (7.0° ± 7.0 vs. 2.7° ± 5.1 respectively; p = 0.041; CI [-8.301 to -0.183]) (Table 5).
Discussion
The results of this study show that goniometric measures that represent values consistent with flattening of the medial longitudinal arch are associated with signs of joint degeneration of the 1MTPJ, with the Meary-Tomeno angle showing the best association with the clinical-radiographic diagnosis of HR.
We have not found studies comparing the radiological morphology in the midfoot or rearfoot with the presence of HR, so we cannot make direct comparisons with our results. However, some authors(16,17,18) have previously demonstrated that certain structural changes in the forefoot, such as HAV, are related to the presence of HR, suggesting that other deformities in the midfoot or rearfoot might be related to this pathology, which seems to be suggested by our findings.
Coughlin and Shurnas(5) did not find an association between HR and abnormal foot position. However, they analyzed rearfoot deformities based on clinical evaluation of calcaneal position and considered pathological values > 6° of valgus and arch height by the width of the arch measured in the plantar footprint. Radiographic goniometric values are more precise for detecting subtler changes in foot morphology, so we recommend further studies using this methodology to confirm our findings.
On the other hand, Anwander et al.(3) found a direct relationship with MPE. One reason could be the impact of pronation or flattening of the midfoot and/or rearfoot, which could favor deformation in a dorsiflexion position of the first metatarsal, thus contributing to the initial stages of HR(19).
Our results suggest that it is important to evaluate the position of the foot in a weight-bearing lateral X-ray to determine foot position, recommending the measurement of the Meary-Tomeno angle since the presence of a plantar vertex was associated with a higher presence of HR.
The results of this study should be interpreted with caution. Firstly, because a sample size calculation was not carried out, and therefore we consider the study sample to be small. Secondly, because the sample does not proportionally represent all HR stages, with milder stages of this disease being predominant. However, this could suggest that variations in goniometric angles are associated with the presence of HR in the early stages, although future studies are needed to prove this. The main strength of the study is that it is the first to evaluate the association between midfoot and rearfoot morphology in the sagittal plane via X-ray with 1MTPJ degeneration.
In conclusión, the results of the present study have shown that goniometric measures that represent values consistent with flattening of the MLA are associated with signs of joint degeneration of the 1MTPJ, with the Meary-Tomeno angle showing the best association with the clinical-radiographic diagnosis of HR, suggesting a possible association between HR and tarsal pronation or flatfoot.
Ethics declaration
The study was conducted and completed in full compliance with the ethical standards of the responsible committee, and ethical approval was obtained (Ethics Committee of Hospital Clínico San Carlos [IdISSC], with internal code: 22/355-E). Informed consent was obtained from all patients included in the study. The authors declare that the study complied with the ethical code of the Declaration of Helsinki.
Conflicts of interest
None declared.
Funding
None declared.
Authors’ contributions
Study idea and design: RSS, MNC, RCM, and OMA.
Data collection: RSS, MNC, and OMA.
Analysis and interpretation of results: RSS, MNC, RMB, AMOG, and OMA.
Drafting, writing, and preparation of the initial manuscript: RSS, MNC, RCM, RMB, AMOG, and OMA.
Review and approval of the final version prior to publication: RSS, MNC, RMB, AMOG, and OMA.
References
- Jacob HA. Forces acting in the forefoot during normal gait--an estimate. Clin Biomech (Bristol, Avon) 2001;16(9):783-92. DOI: 10.1016/S0268-0033(01)00070-5.
- Di Caprio F, Mosca M, Ceccarelli F, Caravelli S, Vocale E, Zaffagnini S, et al. Hallux Rigidus: Current Concepts Review and Treatment Algorithm with Special Focus on Interposition Arthroplasty. Acta Biomed [Internet]. 2022;93(5):e2022218.
- Anwander H, Alkhatatba M, Lerch T, Schmaranzer F, Krause FG. Evaluation of Radiographic Features Including Metatarsus Primus Elevatus in Hallux Rigidus. J Foot Ankle Surg. 2022;61(4):831-5. DOI: 10.1053/j.jfas.2021.11.027.
- Bro NK, Lange J, Kabel JF. Diagnostik og behandling af hallux rigidus. Ugeskr Laeger. 2021;182(14):1-8.
- Coughlin MJ, Shurnas PS. Hallux rigidus: Demographics, etiology, and radiographic assessment. Foot Ankle Int. 2003;24(10):731-43. DOI: 10.1177/107110070302401002.
- Dananberg HJ. Functional hallux limitus and its relationship to gait efficiency. J Am Podiatr Med Assoc. 1986;76(11):648-52. DOI: 10.7547/87507315-76-11-648.
- Harradine PD, Bevan LS. The Effect of Rearfoot Eversion on Maximal Hallux Dorsiflexion. A Preliminary Study. J Am Podiatr Med Assoc. 2000;90(8):390-3.
- Scherer PR. Heel spur syndrome. Pathomechanics and nonsurgical treatment. Biomechanics Graduate Research Group for 1988. J Am Podiatr Med Assoc. 1991;81(2):68.
- Fuller E. The windlass mechanism of the foot. J Am Podiatr Med Assoc. 2000;90(1):35-46. DOI: 10.7547/87507315-90-1-35.
- López del Amo-Lorente A, Cintado-Reyes R, Munuera-Martínez PV, González-Úbeda R, Salcini-Macías JL. ¿Cuál es el protocolo de exploración más adecuado a la hora de valorar la primera articulación metatarsofalángica? Rev Esp Podol. 2013;(1):25-9.
- Ogalla JM, Zalazain A. Goniometría. Rev Esp Podol. 1991;2(5):247-53.
- Westberry DE, Davids JR, Roush TF, Pugh LI. Qualitative versus quantitative radiographic analysis of foot deformities in children with hemiplegic cerebral palsy. J Pediatr Orthop. 2008;28(3):359-65. DOI: 10.1097/BPO.0b013e3181653b51.
- Liu W, Chen Y, Zeng G, Yang T, Ma M, Song W. Individual Surgical Treatment of Stage IV Müller-Weiss Disease According to CT/MRI Examination: A Retrospective Study of 12 Cases. Front Surg. 2022;9(March):1-10.
- Bobi?ski A, Tomczyk ?, Reichert P, Morasiewicz P. Short-Term and Medium-Term Radiological and Clinical Assessment of Patients with Symptomatic Flexible Flatfoot Following Subtalar Arthroereisis with Spherus Screw. J Clin Med. 2023;12(15):5038. DOI: 10.3390/jcm12155038.
- Alsaidi FA, Moria KM. Flatfeet Severity-Level Detection Based on Alignment Measuring. Sensors. 2023;23(19):1-16.
- D’Arcangelo PR, Landorf KB, Munteanu SE, Zammit G V., Menz HB. Radiographic correlates of hallux valgus severity in older people. J Foot Ankle Res. 2010;3(1):1-9. DOI: 10.1186/1757-1146-3-20.
- Roddy E, Zhang W, Doherty M. Prevalence and associations of hallux valgus in a primary care population. Arthritis Care Res. 2008;59(6):857-62. DOI: 10.1002/art.23709.
- Cho NH, Kim S, Kwon DJ, Kim HA. The prevalence of hallux valgus and its association with foot pain and function in a rural Korean community. J Bone Joint Surg Br. 2009;91(4):494-8. DOI: 10.1302/0301-620X.91B4.21925.
- Nubé VL, Molyneaux L, Yue DK. Biomechanical risk factors associated with neuropathic ulceration of the hallux in people with diabetes mellitus. J Am Podiatr Med Assoc. 2006;96(3):189-97. DOI: 10.7547/0960189.