DOI: 10.20986/revesppod.2022.1624/2021
ORIGINAL
Treatment and evolution of diabetic foot ulcers with suspected osteomyelitis in a recently new diabetic foot unit: observational pilot study
Tratamiento y evolución de úlceras de pie diabético con sospecha de osteomielitis en una unidad de pie diabético de nueva creación: estudio piloto observacional
Mónica Arizmendi Pérez
Esther Bravo Ruiz
Raúl Torre Puente
Josu Mirena Baraia-Etxaburu Artetxe
Eider Etxeberria Martín
Javier Pascual Huerta
Diabetic Foot Unit. OSI Bilbao-Basurto (Vizcaya). Hospital Universitario Basurto, Bilbao, Spain
Abstract
Objectives: Treatment of diabetic foot ulcers complicated with osteomyelitis (OM) is still a controversial issue. This work presents a case series showing the experience with these patients in a newly formed diabetic foot unit.
Patients and methods: Patients with active foot ulcer and having the criteria of suspected OM (positive Probe to bone test with an image test, simple x-ray or MR, suggestive of OM) were analyzed retrospectively. Data of ulcer location, evolution time, soft tissue infection, peripheral arterial disease (PAD), treatments employed (antibiotics, dressings, offloading and/or revascularization) and final outcome (healed ulcer or not) were recorded and analyzed.
Results: Twelve ulcer cases in 8 patients were included. Nine cases (75 %) were located in forefoot and 3 (25 %) in rearfoot. Five cases (42 %) had soft tissue infection, 6 (50 %) moderate and 1 (8 %) severe. The 66,7 % (n = 8) healed with conservative treatment (6 cases with antibiotics and offloading and 2 cases with offloading and no antibiotic therapy). Four cases (33,3 %) did not resolved and underwent amputation (2 mayor cases and 2 minor cases). Seventy-five percent of amputated cases (n = 3) had PAD.
Conclusions: Despite the small sample size, this case series reflects that conservative treatment could be effective in these patients, it also shows the role of PAD in the final outcome of amputation and open new hypothesis about diagnoses and treatment for those patients.
Key words: Osteomyelitis, diabetic foot, diabetic foot ulcer, treatment, case series, diabetic foot unit.
Resumen
Objetivos: El tratamiento de úlceras de pie diabético complicadas con osteomielitis (OM) sigue siendo un aspecto controvertido actualmente. Este trabajo presenta una serie de casos que muestra la experiencia de una unidad de nueva creación en el tratamiento y evolución de estos pacientes.
Pacientes y métodos: Se analizaron retrospectivamente pacientes atendidos con ulceración activa y que cumplían criterios de sospecha de OM: Probe to Bone positivo junto con prueba de imagen (radiografía simple o RMN) sugestiva de OM. Se analizaron diversos datos de localización, tiempo de evolución, infección de partes blandas, enfermedad arterial periférica (EAP), tratamientos realizados (antibioterapia, curas, descarga y/o revascularización) y desenlace final del proceso entendido como curación de la úlcera o no.
Resultados: Se incluyeron 12 episodios ulcerosos en 8 pacientes. Nueve episodios (75 %) estaban localizados en antepié y 3 (25 %) en retropié. Cinco (42 %) casos presentaban infección de partes blandas leve, 6 (50 %) moderada y 1 (8 %) severa. El 66,7 % (n = 8) curaron con tratamiento conservador (6 casos con antibiótico más descarga y 2 casos con descarga, sin asociar antibioterapia). El 33,3 % (n = 4) no se resolvieron y requirieron amputación (dos casos mayores y dos casos menores). De los casos con amputación, el 75 % (n = 3) asociaba EAP.
Conclusiones: Pese a la limitación del tamaño muestral, esta serie refleja que el tratamiento conservador podría ser eficaz en este tipo de casos, señala la influencia de la EAP en el desenlace final de amputación y plantea nuevas hipótesis acerca del diagnóstico y tratamiento de estos pacientes.
Palabras clave: Osteomielitis, pie diabético, úlceras de pie diabético, tratamiento, serie de casos, unidad de pie diabético.
Received: 07-12-2021
Accepted: 24-03-2022
Correspondence: Javier Pascual Huerta
javier.pascual@hotmail.com
INTRODUCTION
Osteomyelitis (OM) of the diabetic foot remains a difficult and complex condition to diagnose, manage and treat. It is commonly accepted that the presence of osteomyelitis is possible in any diabetic foot ulcer, especially in those ulcers that have been present for many weeks, or that are wide, deep, located over bony prominences, have bony exposure or are accompanied by swollen or erythematous toes (sausage toes)1-3. Despite this, accurate screening for OM in the diabetic foot is particularly challenging due to the lack of a universally accepted standard definition or criteria4 and the low levels of concordance between the most commonly used diagnostic tests5. The latest update of the International Working Group of Diabetic Foot (IWGDF) guidelines on diabetic foot infections recommends that in people with diabetes and clinical suspicion of osteomyelitis of the foot, if plain radiography and clinical and laboratory findings are compatible with osteomyelitis, no further foot imaging tests should be performed to confirm the diagnosis1. However, to date, no studies have assessed the validity or success of this approach as a way to screen for OM in diabetic infectious foot pathology.
Bone resection accompanied by long periods of antibiotic therapy has traditionally been the treatment of choice in cases of osteomyelitis (OM) in the diabetic foot6,7. This approach is currently controversial as several studies in the last years have described that conservative treatment may be effective in a significant percentage of these cases. In this regard, the different updates of the International Working Group of Diabetic Foot (IWGDF) guidelines have varied their recommendations regarding treatment in this type of patient1,4,14. The latest update in 20191 advises in cases of uncomplicated OM to consider antibiotic therapy for a period of no more than 6 weeks without bone resection, although it does not establish definitive recommendations regarding the route of administration and/or the length of treatment required. Moreover, there is also no consensus as to whether offloading of the ulcer area could help to improve the overall process and shorten the antibiotic treatment time in these patients.
There is therefore, a clear need for further studies to provide more information and evidence regarding the diagnosis and optimal treatment of patients with OM in diabetic foot. Likewise, within conservative treatment, more studies are needed to better determine the duration of optimal antibiotic treatment in these patients and the need or not for adjuvant treatments such as offloading therapy. The aim of the present study is to report the experience of a newly established diabetic foot unit (DFU) in the conservative treatment of patients with diabetic foot OM using the diagnostic criteria of the IWGDF with a post treatment follow-up for at least 1 year. The study aims to describe in a sample of patients, which treatments were used with conservative approach and what was the evolution of the disease in terms of ulceration closure (healing), non-healing or major or minor amputation of these patients.
PATIENTS AND METHODS
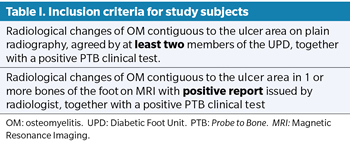
The present study corresponds to a retrospective observational study of the case series type. We retrospectively analyzed patients seen in the UPD of the OSI Bilbao-Basurto (Vizcaya) since its creation (from June 2019 and the full year 2020) with active ulceration and who met the following inclusion criteria (Table I): (a) Radiological changes compatible with OM contiguous to the focus of ulceration on plain radiographs, together with a positive clinical Probe to Bone (PTB) test, consisting of direct palpation of bone through the ulcer with a metallic, blunt and sterile instrument. The radiological changes in the plain X-ray were agreed by the podiatrist, the orthopedic surgeon and the vascular surgeon of the unit, and at least two of them had to agreed to classify the radiological changes as OM; b) Radiological changes of OM contiguous to a focus of ulceration in 1 or more bones of the foot in the Magnetic Resonance Imaging (MRI) study with a positive report for OM issued by the radiology service of the hospital. The exclusion criteria were the presence of a negative PTB test in the ulceration and in cases in which a positive PTB test did not reveal radiological changes compatible with OM or only one of the members of the unit classified the radiological changes as OM and not two members.
Each episode of active ulceration was counted as a separate case for data analysis. So, those patients who presented with two ulceration processes on the same foot (e.g. toes and heel) or on different feet (right and left) and who met the inclusion criteria for the study were counted as separate cases for data analysis. Patients were followed up until September 2021, as part of the protocol carried out on patients in the unit to ensure that the follow-up time was not less than one year.
The variables of the selected cases were analyzed with respect to age, sex, type of diabetes, personal history, location and time of evolution of the ulcer, presence of soft tissue infection (according to the IDSA/IWGDF classification)1, peripheral arterial disease -PAI- (defined as absence of distal pulses and/or ankle-brachial index < 0.9), the treatments performed (including antibiotherapy regimen, dressings, offloading and/or re- vascularization), the final outcome of the process (understood as healing or non-healing of the ulceration), the follow-up time and the presence or absence of ulcer recurrence. Treatment was considered effective when there was complete healing of the ulceration and no recurrence at the same site during the entire follow-up period. However, treatment was considered to have failed in cases where the ulceration did not heal or the patient required amputation (major or minor). The occurrence of another episode of ulceration on the contralateral limb or in a different location on the same foot (e.g. hindfoot or another area of the forefoot) was not considered a recurrence of the lesion.
Statistical analysis was carried out by making a simple data table during retrospective data collection. Subsequently, the data were analyzed as simple percentages of the data and the open access software R was used [R Core Team (2021). R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. URL https://www.R-project.org/] to calculate the means and standard deviations of the continuous variables analyzed.
RESULTS
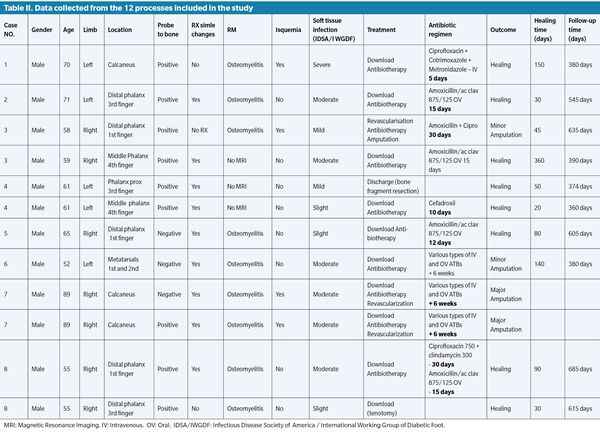
A total of 12 ulcer episodes with suspected OM that met the inclusion criteria were included in 8 patients. Table II shows all the relevant patient data and variables analyzed. All of the patients were male type 2 diabetics with a mean age of 65.41 ± 11.89 years. Nine episodes (75 %) were located in the forefoot and 3 (25%) in the rearfoot, specifically in the calcaneus. Five cases (42 %) had mild infection, 6 (50 %) had moderate infection and 1(8 %) severe, according to the IDSA/IWGDF classification. One third of the cases (33.3 %; n = 4) were associated with PAD.
Regarding the evolution of the ulcerations, 66.7 % (n = 8) healed with conservative treatment (6 cases with antibiotic plus offloading, and 2 cases with offloading only without antibiotic therapy), and 33.3 % (n = 4) did not resolve and required amputation (two major cases and two minor cases). The mean healing time was 99.5 ± 102.15 days, and the mean follow-up time was 496.9 ± 131.23 days. During the follow-up time, no recurrence of ulceration in the same anatomical location was observed of the 8 resolved cases. Of the 4 cases requiring amputation, 75 % (n = 3) were associated with PAD. The two major amputations were performed on the same patient (both limbs) who subsequently died. One of the minor amputations was associated with an hybrid revascularization procedure (open and endovascular), and the other case already had a previous lateral metatarsal amputation by the service of vascular surgery of the hospital.
The antibiotic treatment regimen varied from patient to patient. All antibiotic treatments were based on the results of the microbiological culture and antibiogram performed on the ulcer. Empirical antibiotic treatment was initially prescribed with subsequent adjustment of treatment if the empirical treatment was not initially correct. Likewise, the duration of antibiotic treatment was determined by the evolution of the clinical soft tissue infection, without taking into account subsequent radiological controls or the presence of bone exposure in the duration of antibiotic treatment. Two cases with mild soft tissue infection did not receive antibiotic treatment and were cured with offloading alone, 5 cases (2 with mild infection, 2 with moderate infection and 1 with severe infection) received a short course of oral antibiotherapy (14 days or less), 1 case with mild infection and 1 case with moderate infection had prolonged antibiotic treatment for 4 weeks, and 3 cases with moderate infection received several intravenous and oral courses for more than 6 weeks (2 of these cases had an outcome of major and/or minor amputation). Table II lists the antibiotics, dosage and duration of treatment used in the study subjects.
DISCUSSION
This paper reports the results of a small case series on the experience, mainly with conservative treatment of patients with suspected diabetic foot OM who were followed up for at least 1 year after conservative treatment and in which the diagnostic criteria recommended by the IWGDF were followed.
The optimal treatment of patients with OM in diabetic foot is currently a real challenge. It is not clear which is the ideal approach in these cases (surgical vs. conservative) and there is no strong evidence about the optimal duration, dose and route of administration for antibiotic treatment in this type of patients. Surgical resection of the infected bone together with antibiotic therapy for a period of no less than 6 weeks has for many years been the gold standard for the treatment of OM in the diabetic foot6,7 but in recent years this approach has been questioned. International guidelines have been changing their recommendations regarding the treatment of this problem1,2,14,15. The latest guideline from 2019 recommends antibiotic treatment for no more than 6 weeks in cases of conservative treatment and if all infected bone has been removed, continued only a few days thereafter if there is no soft tissue infection1. In the present study, two of the cases in the series healed with offloading alone and without associated antibiotic treatment despite meeting the clinical-radiological diagnostic criteria for OM. In one case, resection of the head of the proximal phalanx exposed was performed in the office, and in the other case, percutaneous tenotomy of the long and short flexor of the 3rd toe was performed as way of offloading due to the presence of ulceration with signs of OM in the distal phalanx of the 3rd toe also diagnosed by MRI. None of these 2 cases had associated soft tissue cellulitis. Furthermore, in 5 of the cases, a short course of antibiotic therapy (equal to or less than 2 weeks orally) was administered, with which the infectious clinical picture of the soft tissue subsided and which, accompanied by offloading from the area and without resection of the bone fragment, healed the ulcerations without evidence of reulceration in a period of more than 1 year of follow-up time. We understand that these findings are confusing and could mean errors in the diagnosis of OM in the diabetic foot (false positives) despite following the currently accepted criteria for the diagnosis of this disorder. Furthermore, the data collected in the present study shows that many of these cases healed the ulceration simply by control of the soft tissue infection and offloading the area without the association of long-term antibiotic therapy or bone resection of the bone with OM. It is possible that effective offloading of ulcerative lesions in patients with suspected OM may help to improve the clinical picture and wound healing although there is no theoretical basis for this argument.
The literature considers the diagnosis of OM to be proven when one or more pathogens are cultured on a reliable bone specimen that in turn shows necrosis, acute or chronic inflammation and reparative response on histopathological examination4. Unfortunately, this criterion is rarely found in most published studies and clinical cases of patients treated with suspected OM, as clinicians rarely rely on double bone biopsy (microbiological culture and hitopathological analysis) for the diagnosis of OM, and focus more on the clinical presentation of the lesion (positive PTB) combined with radiological imaging findings and a variety of laboratory values11,13,16-20. This aspect is a limitation in the interpretation of the results of the different publications, and the present study has the same limitation as the cases presented were diagnosed as OM following the inclusion criteria set out in table I and in line with the most recent IWGDF recommendations for the diagnosis of OM1. This approach cannot rule out the presence of false positives in the sample. To increase the specificity of the inclusion criteria, in the present study it was established that radiological changes on plain radiographs should be consensual and at least 2 members of the UPD should categorize them as compatible with OM. This aspect is considered important as many of the radiological findings such as rarefaction, focal demineralisation, loss of trabecular pattern, demineralization, periosteal reaction or sclerosis may be subjective, especially in the early stages, constituting a subjective bias in interpretation. In fact, in the present study a significant number of cases were not included despite having positive PTB test because the radiological changes were only noted by one of the team members and not by 2 members. Despite all this, none of the cases included in the present series had a diagnosis by double bone biopsy consisting of microbiological culture together with anatomopathological analysis of the bone sample.
It is well known that the presence of ischemia is a critical prognostic factor in patients with diabetic foot ulceration21-26 The EURODIALE study21 showed the importance of PAD in the prognosis and outcomes of diabetic patients with foot ulceration, with a significantly higher percentage of failed healing as well as major amputations and mortality in cases with associated ischaemia. Several subsequent studies have corroborated these findings in diabetic patients22-24, and especially in those with associated soft tissue infection25 and OM26. In the present study, 3 of the 4 cases that underwent amputation had PAD. The only two major amputations in the series were performed in the same patient with PAD who subsequently died, and another case with PAD that required minor amputation while associating a hybrid revascularization procedure (open and endovascular). These findings are in agreement with the data provided by Aragón- Sánchez et al. who showed that the presence of PAD is one of the most important prognostic values for amputation over and above the radiological changes of bone destruction observed in patients with a diagnosis of OM27.
The present study has certain limitations that must be taken into account. Some of these limitations have already been mentioned in the discussion, such as the absence of culture and/or anatomopathological analysis in the diagnosis of OM, which may increase the number of false positives in the sample, as well as the variable regimen of antibiotic therapy prescribed. The duration of the antibiotic treatments was marked by the evolution of the clinical picture of the patients, especially of the associated soft tissue infection, without considering the radiological evolution of OM. Because of this, it is impossible to draw any valid conclusions about the type of antibiotic, dosage and optimal route of administration in this series of cases, although we understand that this is not the aim of the study but the role that antibiotic therapy can play in the resolution of ulceration in these patients and that, according to the results extracted, it may not be the most relevant factor for bone healing. Although it is true that the main limitation of the study is the small number of patients used in the sample, which prevents reliable conclusions from being drawn from the results obtained, although they show a similar trend to that obtained in other series with a larger number of cases8,12,13,16.
In conclusion, the present study describes a small series of cases of diabetic patients with foot ulceration and a clinical-radiological diagnosis of OM who were treated in a recently created UPD using conservative treatment. Of the episodes, 66.7 % (n =8 ) were cured with conservative treatment including offloading and a variable antibiotic therapy regimen (3 with a short course of less than 14 days and 3 with a course of 2-4 weeks, and 2 cases were cured only with offloading treatment without antibiotics). Of the 4 cases that failed and required amputation, 75 % (n = 3) were associated with PAD and were those patients who received more prolonged antibiotic therapy. Despite having a small sample size, the findings of this series suggest that conservative treatment could be effective in this type of cases, which should be demonstrated in future research and raises new hypotheses about the role that unloading treatment could have in these patients.
ETHICS DECLARATION
As a retrospective observational study approval from an ethics committee was not applied for. The study was performed following the recommendations and standard care about security of patients of Helsinki declaration. The confidentiality of the data obtained for the study was respected in an anonymous and dissociated manner, following the guidelines of the Organic Law on Data Protection of Spain (Law 15/1999 of 13 December).
CONFLICT OF INTEREST
The authors declare that they have no relevant conflicts of interest in relation to this study.
FUNDING
This article did not present any funding
AUTHORS CONTRIBUTION
MAP, EBS, RTP and JPH participated in study conception and design; MAP, EBS, RTP did data collection; JPH performed data analysis and interpretation; MAP, EBS, RTP, JMBEA, EEM and JPH reviewed critically the manuscript and accepted the final version.
BIBLIOGRAFÍA
- Lipsky BA, Senneville É, Abbas ZG, Aragón-Sánchez J, Diggle M, Embil JM, et al. Guidelines on the diagnosis and treatment of foot infection in persons with diabetes (IWGDF 2019 update). Diabetes Metab Res Rev. 2020;36(S1):e3280. DOI: 10.1002/dmrr.3280.
- Lipsky BA, Berendt AR, Deery HG, Embil JM, Joseph WS, et al. Diagnosis and Treatment of Diabetic Foot Infections. Clin Infect Dis. 2004;39(7):885-910. DOI: 1058-4838/2004/3907-0001. DOI: 10.1086/424846.
- Lázaro-Martínez JL, Tardáguila-García A, García-Klepzig JL. Diagnostic and therapeutic update on diabetic foot osteomyelitis. Endocrinol Diabetes y Nutr. 2017;64(2):100-8. DOI: 10.1016/j.endinu.2016.10.008.
- Berendt AR, Peters EJ, Bakker K, Embil JM, Eneroth M, Hinchliffe RJ, et al. Diabetic foot osteomyelitis: a progress report on diagnosis and a systematic review of treatment. Diabetes Metab Res Rev. 2008;24(suppl 1):S145-S161. DOI: 10.1002/dmrr.836.
- Meyr AJ, Seo K, Khurana JS, Choksi R, Chakraborty B. Level of Agreement With a Multi-Test Approach to the Diagnosis of Diabetic Foot Osteomyelitis. J Foot Ankle Surg. 2018;57(6):1137-9. DOI: 10.1053/j.jfas.2018.05.010.
- Lipsky BA. Osteomyelitis of the foot in diabetic patients. Clin Infect Dis. 1997;25(6):1318-26. DOI: 10.1086/516148.
- Norden CW. Lessons learned from animal models of osteomyelitis. Rev Infect Dis. 1988;10(1):103-9. DOI: 10.1093/clinids/10.1.103.
- Acharya S, Soliman M, Egun A, Rajbhandari SM. Conservative management of diabetic foot osteomyelitis. Diabetes Res Clin Pract. 2013;101(3):e18-20. DOI: 10.1016/j.diabres.2013.06.010.
- Lesens O, Desbiez F, Theis C, Ferry T, Bensalem M, Laurichesse H, et al. Staphylococcus aureus-Related Diabetic Osteomyelitis: Medical or Surgical Management? A French and Spanish Retrospective Cohort. Int J Low Extrem Wounds. 2015;14(3):284-90. DOI: 10.1177/1534734614559931.
- Lázaro-Martínez JL, Aragón-Sánchez J, García-Morales E. Antibiotics versus conservative surgery for treating diabetic foot osteomyelitis: a randomized comparative trial. Diabetes Care. 2014;37(3):789-95. DOI: 10.2337/dc13-1526.
- Senneville E, Lombart A, Beltrand E, Valette M, Legout L, Cazaubiel M, et al. Outcome of diabetic foot osteomyelitis treated nonsurgically: a retrospective cohort study. Diabetes Care. 2008;31(4):637-42. DOI: 10.2337/dc07-1744.
- Tardáguila-García A, Sanz-Corbalán I, García-Alamino JM, Ahluwalia R, Uccioli L, Lázaro-Martínez JL. Medical Versus Surgical Treatment for the Management of Diabetic Foot Osteomyelitis: A Systematic Review. J Clin Med. 2021;10(6): 1237. DOI: 10.3390/jcm10061237.
- Lesens O, Desbiez F, Vidal M, Robin F, Descamps S, Beytout J, et al. Culture of perwound bone specimens: a simplified approach for the medical management of diabetic foot osteomyelitis. Clin Microbiol Infect. 2011;17(2):285-91. DOI: 10.1111/j.1469-0691.2010.03194.x.
- Lipsky BA, Aragón-Sánchez J, Diggle M, Embil J, Kono S, Lavery L, et al. International Working Group on the Diabetic Foot (IWGDF). IWGDF guidance on the diagnosis and management of foot infections in persons with diabetes. Diabetes Metab Res Rev. 2016;32(Suppl 1):45-74. DOI: 10.1002/dmrr.2699.
- Lipsky BA; International consensus group on diagnosing and treating the infected diabetic foot. A report from the international consensus on diagnosing and treating the infected diabetic foot. Diabetes Metab Res Rev. 2004;20(Suppl. 1):S68-77. DOI: 10.1002/dmrr.453.
- Tardáguila-García A, García-Álvarez Y, García-Morales E, López-Moral M, Sanz-Corbalán I, Lázaro-Martínez JL. Long-Term Complications after Surgical or Medical Treatment of Predominantly Forefoot Diabetic Foot Osteomyelitis: 1 Year Follow Up. J Clin Med. 2021;10(9):1943. DOI: 10.3390/jcm10091943.
- Mutluoglu M, Lipsky BA. Non-surgical treatment of diabetic foot osteomyelitis. Lancet Diabetes Endocrinol. 2017;5(8):668. DOI: 10.1016/S2213-8587(16)30141-3.
- Loupa CV, Meimeti E, Voyatzoglou E, Donou A, Koutsantoniou E, Lafoyanni S. Successful nonsurgical therapy of a diabetic foot osteomyelitis in a patient with peripheral artery disease with almost complete radiological restoration. BMC Res Notes. 2018;11(1):579. DOI: 10.1186/s13104-018-3694-x.
- Lipstick BA. Bone of Contention: Diagnosing Diabetic Foot Osteomyelitis. Clin Infect Dis. 2008;15:47(4):528-30. DOI: 10.1086/590012.
- Ugwu E, Adeleye O, Gezawa I, Okpe I, Enamino M, Ezeani I. Predictors of lower extremity amputation in patients with diabetic foot ulcer: findings from MEDFUN, a multicenter observational study. J Foot Ankle Res. 2019;12:34. DOI: 10.1186/s13047-019-0345-y.
- Prompers L, Schaper N, Apelqvist J, Edmonds M, Jude E, Mauricio D, et al. Prediction of outcome in individuals with diabetic foot ulcers: focus on the differences between individuals with and without peripheral arterial disease. The EURODIALE Study. Diabetologia. 2008;51(5):747-55. DOI: 10.1007/s00125-008-0940-0.
- Baba M, Davis WA, Norman PE, Davies TME. Temporal changes in the prevalence and associates of diabetes-related lower extremity amputations in patients with type 2 diabetes: the Fremantle Diabetes Study. Cardiovasc Diabetol. 2015;14:152. DOI: 10.1186/s12933-015-0315-z.
- Gershater MA, Löndahl M, Nyberg P, Larsson J, Thörne J, Eneroth M, et al. Complexity of factors related to outcome of neuropathic and neuroiscaemic/ischaemic diabetic foot ulcers: a cohort study. Diabetologia. 2009;52(3):398-407. DOI: 10.1007/s00125-008-1226-2.
- Sen P, Demirdal T, Emir B. Meta-analysis of risk factors for amputation in diabetic foot infections. Diabetes Metab Res Rev. 2019;35(7):e3165. DOI: 10.1002/dmrr.3165.
- Aysert YP, Ozdil T, Dizbay M, Guzel TO, Hizel K. Peripheral arterial disease increases the risk of multidrug-resistant bacteria and amputation in diabetic foot infections. Turk J Med Sci. 2018;48(4):845-50. DOI: 10.3906/sag-1803-217.
- Barshes NR, Mindru C, Ashong C, Rodriguez-Barrdas M, Trautner BW. Treatment Failure and Leg Amputation Among Patients With Foot Osteomyelitis. Int J Low Extrem Wounds. 2016;15(4):303-12. DOI: 10.1177/1534734616661058.
- Aragón-Sánchez J, Lázaro-Martínez JL, Campillo-Vilorio N, Quintana-Marrero Y, Hernández-Herrero MJ. Controversies regarding radiological changes and variables predicting amputation in a surgical series of diabetic foot osteomyelitis. Foot Ankle Surg. 2012;18(4):233-6. DOI: 10.1016/j.fas.2012.01.005.