doi.org/10.20986/revesppod.2025.1755/2025
CLINICAL CASE
Surgical management of intratendinous multinodular ganglion. A clinical case
Tratamiento quirúrgico de ganglión polinodular intratendinoso. Caso clínico
Ana M.ª Rayo Pérez1
Rafael Rayo Rosado1
Rafael Rayo Martín1
Alberto Rayo Martín2
Raquel García de la Peña1
1Departamento de Podología. Universidad de Sevilla, España
2Clínica Rayo. Arahal, Sevilla, España
Abstract
Ganglion cysts are the most common benign soft tissue tumors of the foot and ankle. Although often asymptomatic, they may cause pain, functional limitation, and difficulty wearing shoes depending on their location. We report the case of a 54-year-old male presenting with a painful mass on the dorsum of the right foot, along the course of the extensor digitorum longus tendon of the fourth toe, with a three-month evolution following local trauma. Ultrasonography revealed a hypoechoic mass arising from the tendon sheath, consistent with a synovial cyst, subsequently confirmed by histopathological examination. Initial management with ultrasound-guided percutaneous drainage, including aspiration and triamcinolone acetonide injection, proved ineffective, with persistent lesion and symptoms. Due to the lack of response, a complete outpatient surgical excision was performed, including the pedicle and associated portion of the tendon sheath, under regional anesthesia and prophylactic antibiotic coverage. Postoperative recovery was uneventful, with no complications or recurrence, full functional restoration, and resumption of wearing closed shoes at one-year follow-up. This case highlights the efficacy of complete surgical excision for symptomatic foot ganglia refractory to conservative treatment and emphasizes the importance of histopathological confirmation to exclude other lesions with similar clinical presentation.
Keywords: Ganglion, synovial cyst, benign tumor, surgical treatment, tendon sheath tumor
Resumen
Los gangliones son las tumoraciones benignas más frecuentes de las partes blandas del pie y el tobillo, y aunque suelen ser asintomáticos, pueden producir dolor, limitación funcional y dificultad para el uso de calzado según su localización. Se presenta el caso de un varón de 54 años con una tumoración dolorosa en el dorso del pie derecho, sobre el trayecto del tendón extensor largo del 4.º dedo, de 3 meses de evolución tras un traumatismo local. La ecografía reveló una masa hipoecoica dependiente de la vaina tendinosa, compatible con quiste sinovial, confirmada posteriormente mediante estudio histopatológico. El tratamiento inicial mediante drenaje percutáneo ecoguiado con aspiración del contenido e infiltración de acetónido de triamcinolona resultó ineficaz, persistiendo la lesión y la sintomatología. Ante la falta de respuesta, se realizó exéresis quirúrgica ambulatoria completa, incluyendo el pedículo y la porción de vaina sinovial, bajo anestesia regional y profilaxis antibiótica. La evolución postoperatoria fue favorable, sin complicaciones ni recidivas, con recuperación funcional completa y reincorporación al uso de calzado cerrado al año de seguimiento. Este caso destaca la efectividad de la exéresis quirúrgica completa en gangliones sintomáticos del pie refractarios a tratamientos conservadores, así como la importancia de la confirmación histopatológica para descartar otras lesiones de presentación clínica similar.
Palabras claves: Ganglión, quiste sinovial, tumor benigno, tratamiento quirúrgico, tumor vaina sinovial
Corresponding author
Alberto Rayo Martín
clinicarayo@gmail.com
Received: 04-09-2025
Accepted: 01-11-2025
Introduction
Ganglia are the most common benign soft-tissue tumors of the upper and lower extremities, although their exact incidence in the foot and ankle is relatively low compared with the wrist(1). They are characterized as synovial cysts filled with gelatinous content, frequently associated with joint capsules, tendon sheaths, or periarticular structures. Despite their benign nature, their location may produce significant symptoms, including pain, functional limitation, compression of neurovascular structures, and difficulty with footwear—factors that often prompt surgical intervention(2,3)..
Intratendinous ganglia represent a rare variant, with direct involvement of the affected tendon and potential to compromise digital function. These cysts may develop spontaneously or after repetitive trauma or previous surgical procedures, as described in cases following release of the trigger-finger pulley, in which multiple ganglia formed along the flexor tendon(4).. Diagnosis requires careful evaluation using imaging modalities, with ultrasound and magnetic resonance imaging being the most widel used tools to determine their relationship with tendon and joint structures and to guide surgical planning(5,6)..
Conservative treatment of ganglia includes percutaneous aspiration and, in some cases, corticosteroid injection. However, evidence indicates that these strategies show high recurrence rates due to persistence of the synovial pedicle or adjacent satellite lesions7-9. Recent studies have emphasized that complete surgical excision, including the pedicle and associated capsule, is essential to minimize recurrence and ensure clinical resolution(1,4,8). Open surgery remains the most widely used technique in distal or difficult-to-access locations, whereas endoscopic or arthroscopic approaches are reserved for ganglia with favorable locations and experienced surgeons, offering advantages such as lower invasiveness and faster functional recovery(6,8).
Although most published cases involve ganglia of the hallux, midfoot, and flexor tendons, intratendinous ganglia of the digital extensors—particularly in less frequent locations such as the fourth toe—are rarely reported, limiting the evidence available regarding specific surgical management and functional prognosis(6,7,8,10). This underscores the importance of reporting case reports and small series to consolidate safe and effective therapeutic strategies, improve understanding of surgical anatomy, and reduce postoperative recurrence and complications. The present report describes the case report of an intratendinous ganglion treated with surgical excision, with subsequent histopathologic confirmation.
Case report
A 54-year-old man presented with a mass on the dorsum of the right foot, painful when using closed footwear and appearing after direct trauma to the area. Symptoms had been present for 7 months, with mild mechanical pain, perceived more as pressure / discomfort than sharp pain, without erythema, warmth, or drainage.
The patient reported no known drug allergies and no relevant medical history. There was no family history of musculoskeletal disease.
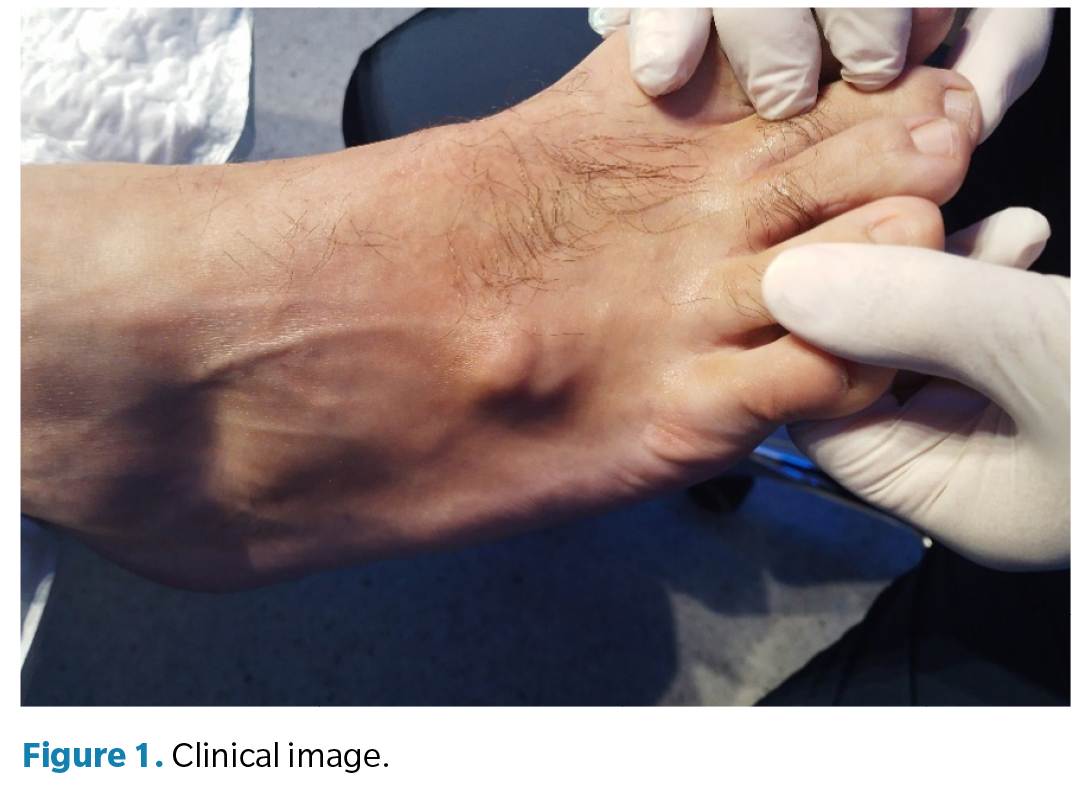
Inspection (Figure 1) revealed a 2/2.5-cm nodular mass on the dorsum of the right foot, over the course of the extensor digitorum longus tendon of the fourth toe, without inflammatory signs or skin changes. On palpation, the mass was elastic, fluctuant, mobile relative to the skin but fixed to deep planes, with mild tenderness. Joint mobility was preserved, with slight discomfort during forced dorsiflexion of the lesser toes. Pedal and posterior tibial pulses were present, and sensation was intact.
Biomechanical assessment revealed mild rearfoot pronation. During gait, the patient completed stance and propulsion phases, but experienced pain when tensioning the extensor tendon of the fourth toe. He reported difficulty using closed footwear, with relief when using wide or open shoes.
Standardized functional questionnaires showed mild impairment in function and quality of life. The SF-36 demonstrated slight limitation in the bodily pain and physical function domains. The Foot Function Index (FFI) score was 32/100, indicating mild functional limitation mainly associated with wearing closed shoes.
Musculoskeletal ultrasound (Figure 2) revealed the presence of a homogeneous, hypoechoic, multinodular lesion with posterior acoustic enhancement, arising from the sheath of the extensor digitorum longus tendon of the fourth toe, compatible with a synovial ganglion. Plain radiographs (anteroposterior and lateral) showed no osseous abnormalities, calcifications, or erosions.
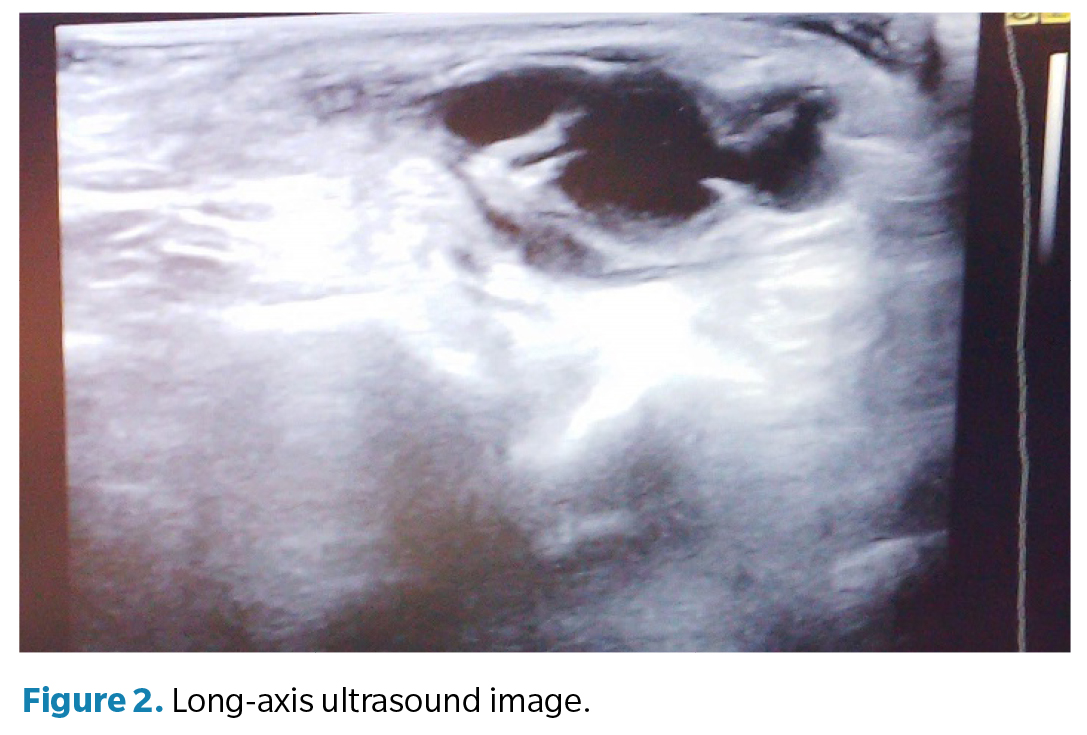
The suspected diagnosis was a ganglion arising from the synovial sheath of the extensor digitorum longus tendon of the fourth toe of the right foot, distal to the fourth metatarsocuboid joint. Ultrasound features ruled out associated joint connection or origin.
Regarding therapeutic management, in May 2024, a minimally invasive ultrasound-guided percutaneous drainage procedure was performed, with aspiration of the characteristic gelatinous material and intralesional corticosteroid injection (Trigon Depot®) to reduce recurrence. The course of the disease was unsatisfactory, with persistence of the mass and symptoms.
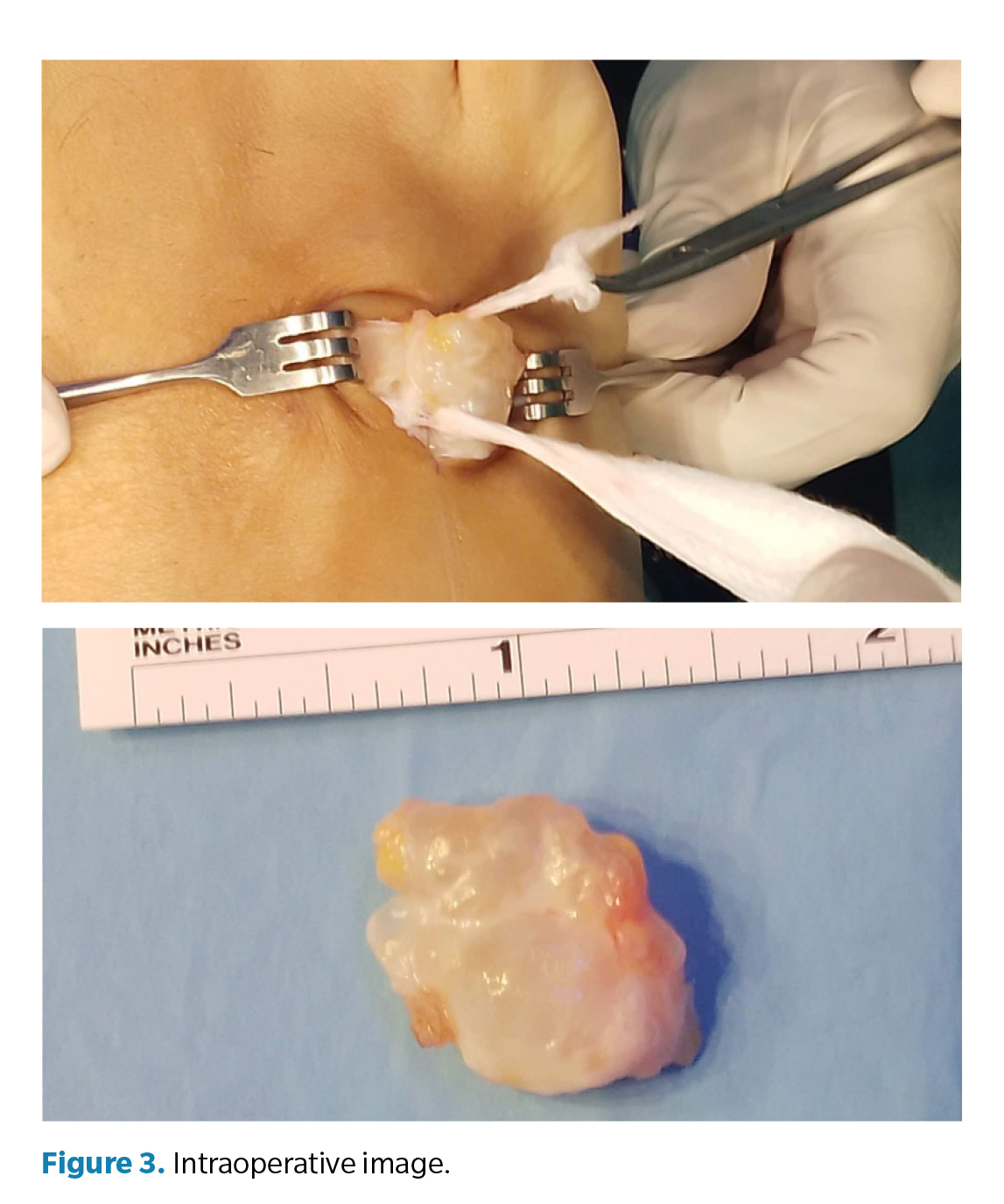
Given the failure of conservative treatment, outpatient surgical excision was performed in August 2025 (Figure 3). The procedure was conducted under local anesthesia using a peripheral nerve block (5 mL of 3% mepivacaine) and with pneumatic tourniquet ischemia at the distal third of the leg (250 mm Hg). Diazepam® 5 mg was administered for sedation, and intraoperative prophylaxis consisted of 2 g of IV cefazolin. A longitudinal incision was performed over the course of the extensor tendon of the 4th toe, followed by careful blunt dissection to identify the cyst capsule. Complete excision of the ganglion, including the pedicle and associated synovial sheath, was then performed while preserving adjacent tendon structures. Closure was achieved in layers: deep layers with absorbable suture (Vicryl 3/0®) and intradermal cutaneous closure with Monocryl 5/0®.
Postoperative management included scheduled oral analgesia (1 g paracetamol and 575 mg metamizole), weekly dressing changes, and partial weight-bearing with a postoperative shoe for 2 weeks, progressing to full weight-bearing after adequate healing. Recovery was uneventful, with no infectious or mechanical complications.
Histopathologic examination confirmed a synovial cyst (ganglion), consisting of a whitish fragment measuring 2.3 cm × 1.8 cm, with a fibrous wall lacking epithelial lining and mucinous-gelatinous content.
At the 1-year postoperative follow-up (September 2025) (Figure 4), the patient showed no evidence of recurrence, with a stable scar, preserved mobility, and full return to normal activities, including use of closed footwear without discomfort. Functional scores showed significant improvement, with normalization of the SF-36 bodily pain and physical function domains and an FFI score of 5/100, indicating no functional limitation.

Discussion
Ganglia and synovial cysts are among the most common causes of benign soft-tissue masses in the foot and ankle, with prevalence varying widely among published series. It is estimated that 10–12 % of soft-tissue masses in this region correspond to ganglia, most frequently located on the dorsum of the foot and associated with tendon sheaths or joint capsules(11,12). Although benign, their clinical presentation varies widely—from asymptomatic incidental findings to painful, limiting lesions that may even cause compressive symptoms involving osseous or neural structures(13,14).
In the present case, the ganglion developed in the sheath of the extensor digitorum longus tendon of the 4th toe, an exceptional location that poses differential diagnostic challenges with other benign foot tumors such as angioleiomyomas or lipomas(16,15). Ultrasound is a highly useful initial tool due to its accessibility and ability to distinguish cystic from solid lesions, whereas magnetic resonance imaging is reserved for diagnostic uncertainty or complex surgical planning(17).
Therapeutic options described in the literature range from clinical observation to percutaneous aspiration with or without corticosteroid injection, as well as open or endoscopic surgical techniques(18,19,20). Aspiration and triamcinolone injection, as performed initially in this patient, are associated with high recurrence rates—reported between 50 and 70 %—due to persistence of the synovial pedicle and communication with the joint or tendon sheath(17,18). Muramatsu et al. (21) described persistence of satellite cysts after conservative treatment, underscoring the difficulty of eradicating the synovial origin without complete surgical excision.
Open surgical excision remains the treatment of choice in most symptomatic cases, with recurrence rates significantly lower than those reported with aspiration. Recent series of foot and ankle ganglia report recurrence rates of 5-15 % after complete excision, depending on location and technique(22,23). In the case described, excision included removal of the pedicle and associated synovial sheath, which we consider essential to minimize recurrence. Studies such as that by Papanastassiou et al. (23) confirm that complete excision of the cyst and pedicle is a key prognostic factor for reducing recurrence risk.
In recent years, endoscopic and arthroscopic techniques have gained relevance, particularly for midfoot and hallux ganglia. These techniques allow less invasive excision, with faster recovery and better cosmetic outcomes(24,25,26). However, they require surgical expertise and are not always feasible in distal locations or in close proximity to neurovascular structures. Harries and Lui19 reported good outcomes with endoscopic excision of complex horseshoe ganglia of the hallux but emphasized the importance of the learning curve and proper patient selection. In comparison, open surgery, as in the present case, provides direct visualization and greater safety in anatomically narrow areas such as the digital extensor sheath.
Postoperative complications reported in the literature are rare but may include superficial infection, dehiscence, joint stiffness, or nerve injury. No such complications occurred in our patient, consistent with the low rates reported in larger series(14,15,22). Postoperative pain management, progressive weight-bearing with a postoperative shoe, and regular wound care align with current recommendations for ambulatory foot surgery performed in an outpatient setting.
Histopathologic analysis is another essential aspect. As Gerstner Saucedo et al. (16) emphasize, lesions appearing clinically consistent with ganglia may correspond to other benign tumors or even rare entities such as angioleiomyomas. Therefore, histopathologic confirmation is indispensable to establish the definitive diagnosis and rule out differential diagnoses.
Prognosis following surgical excision of foot ganglia is generally favorable, with improvement in pain, reduced functional limitation, and low recurrence rates(24,25). In our case, clinical resolution was complete, with no recurrence in initial follow-up, consistent with evidence supporting the effectiveness of open excision in well-defined and accessible lesions.
In conclusion, this case illustrates that ganglia located in the tendon sheath of the digital extensors of the foot, although uncommon, may cause significant functional limitation and difficulty with footwear. Ultrasound-guided percutaneous drainage with corticosteroid injection is an initial therapeutic option but carries a high recurrence rate, as seen in this patient. Complete surgical excision, including the pedicle and associated synovial sheath, remains the most effective approach to resolve symptoms, minimize recurrence, and allow full functional recovery. Clinical follow-up and histopathologic confirmation are essential to ensure comprehensive management and rule out other lesions that may mimic ganglia.
Conflict of interest
None
Funding
None
Authors’ Contributions
Manuscript conception and design: ARM. Data collection: AMRP. Analysis and interpretation of results: RGP. Drafting and manuscript preparation: RRM. Final review: RRR
References
- Gioia di Chiacchio N, di Chiacchio N, Ocampo-Gaza J, Fonseca Noriega L, Freire Santos LA. Surgical treatment of digital mucous cysts with autografting of the overlying skin: A retrospective observational study of 29 cases. Skin Appendage Disord. 2025. DOI:10.1159/000547018.
- Cankurtaran D, Özer B, Çelikel F, Sökmen R, Ünlü Akyüz E. Peroneal nerve palsy due to synovial cyst: An unusual cause of foot drop in a nine-year-old child. Turk J Phys Med Rehabil. 2022;68(4):547-9. DOI: 10.5606/tftrd.2022.7685.
- Fitzsimmons P, Owens RP, Simoncini A, Haddad HW, Kazmi A, Rodriguez RF. Synovial cysts as a rare cause of tarsal tunnel syndrome discovered using ultrasound: A case report. Pain Med Case Rep. 2024;8(7):279-83.
- Lee YK. Formation of multiple ganglion cysts along the flexor tendon after open A1 pulley release for trigger finger: A case report. Medicine (Baltimore). 2022;101(29):e29663. DOI: 10.1097/MD.0000000000029663.
- Guzman A, Williams N, Dela Rueda T, Xiao E, Caliman A, Chen JL, et al. Atraumatic intra-articular, extra-synovial ganglion cyst of the lateral knee deep to the iliotibial band: a case report and review of the literature. Clin Case Rep. 2024;12(2):e8501. DOI: 10.1002/ccr3.8501.
- Chan CK, Lui TH. Endoscopic ganglionectomy of the extensor digitorum longus tendon: An extraganglionic approach. Arthrosc Tech. 2021;10(9):e2073-7. DOI: 10.1016/j.eats.2021.05.002.
- Park JJ, Seok HG, Yan H, Park CH. Recurrence of intratendinous ganglion due to incomplete excision of satellite lesion in the extensor digitorum brevis tendon: A case report. World J Clin Cases. 2022;10(36):13373-80. DOI: 10.12998/wjcc.v10.i36.13373.
- Hao YJ, Li J, Chang JC, Fan JQ, Lyu ZX, Chang BQ, et al. [Clinical efficacy of arthroscopic limited excision of flexor hallucis longus tendon sheath combined with open technique of posterior ankle joint capsule for hallucal ganglion cyst deriving from ankle joint]. Zhonghua Wai Ke Za Zhi. 2025;63(9):829-35.
- Graham JG, McAlpine L, Medina J, Jawahier PA, Beredjiklian PK, Rivlin M. Recurrence of ganglion cysts following re-excision. Arch Bone Jt Surg. 2021;9(4):387-90.
- Aldairi AS, Alsaedi F, Bundagji Y, Al-Zaidi R, Alotaibi H. Ganglion cyst at the lateral aspect of the first metatarsophalangeal joint: Dermatological management with punch biopsy excision. Cureus. 2025;17(3):e80987. DOI: 10.7759/cureus.80987.
- Tay AYW, Tay KS, Thever Y, Hao Y, Yeo NEM. An epidemiological review of 623 foot and ankle soft tissue tumours and pseudo-tumours. Foot Ankle Surg. 2021;27(4):400-4. DOI: 10.1016/j.fas.2020.05.004.
- Ajit Singh V, Sandhu V, Tze Yong C, Yasin NF. Tumours of the foot: A 10 years retrospective analysis. J Orthop Surg (Hong Kong). 2024;32(1):10225536241248706. DOI: 10.1177/10225536241248706.
- Shimozono Y, Mizuno Y, Funakoshi N, Kobayashi M, Matsuda S, Yamashita F. Ganglion cyst of the foot causing second and third metatarsal stress reactions and fractures: A case report. Cureus. 2024;16(7):e65387. DOI: 10.7759/cureus.65387.
- Koketsu K, Kim K, Tajiri T, Isu T, Morimoto D, Kokubo R, et al. Ganglia-induced tarsal tunnel syndrome. J Nippon Med Sch. 2024;91(1):114-8. DOI: 10.1272/jnms.JNMS.2024_91-203.
- Fritzsche H, Weidlich A, Schaser KD, Mehnert E, Winkler D, Rammelt S. Benign tumours of foot and ankle. EFORT Open Rev. 2023;8(6):397-408. DOI: 10.1530/EOR-22-0098.
- Gerstner Saucedo J, Coriat N, Tamayo Y, Moreno J, Gerstner JB, Cardoso FN. Angioleiomyoma of the foot presenting as a ganglion cyst: a case of mistaken identity. Cureus. 2025;17(8):e90980. DOI: 10.7759/cureus.90980.
- Gregush RE, Habusta SF. Ganglion cyst. En: StatPearls. Treasure Island (FL): StatPearls Publishing; 2025.
- Arshad Z, Iqbal AM, Al Shdefat S, Bhatia M. The management of foot and ankle ganglia: A scoping review. Foot (Edinb). 2022;51:101899. DOI: 10.1016/j.foot.2021.101899.
- Harries RJ, Lui TH. Endoscopic resection of horseshoe ganglion of the great toe. Arthrosc Tech. 2024;13(10):103084. DOI: 10.1016/j.eats.2024.103084.
- Chan SY, Lui TH. Endoscopic resection of horseshoe ganglion of the lateral midfoot. Arthrosc Tech. 2024;13(8):103002. DOI: 10.1016/j.eats.2024.103002.
- Muramatsu K, Tani Y, Kobayashi M, Sugimoto H, Iwanaga R, Mihara A, et al. Refractory satellite ganglion cyst in the hallux and finger. Mod Rheumatol Case Rep. 2023;7(1):257-60. DOI: 10.1093/mrcr/rxac036.
- Bak GG, Lee HS, Choi YR, Kim TH, Kim SH. Excision with temporary interphalangeal joint pin fixation for toe ganglion cysts. Clin Orthop Surg. 2023;15(4):653-8. DOI: 10.4055/cios22321.
- Papanastassiou ID, Tolis K, Savvidou O, Fandridis E, Papagelopoulos P, Spyridonos S. Ganglion cysts of the proximal tibiofibular joint: Low risk of recurrence after total cyst excision. Clin Orthop Relat Res. 2021;479(3):534-42. DOI: 10.1097/CORR.0000000000001329.
- Fukushima H, Kimura T, Saito M, Kubota M. Ganglion cysts in the hallux: A report of two cases. Cureus. 2024;16(2):e54423. DOI: 10.7759/cureus.54423.
- Walls RC, Ubillus HA, Azam MT, Kennedy JG, Walls RJ. Intra-tendinous ganglion cyst of the peroneus tertius: A case report and literature review. Am J Case Rep. 2023;24:e938498. DOI: 10.12659/AJCR.938498.
- Zhang QL, Chen L, Han MT, Xu BQ, Hu Y, Li ZX. Clinical efficacy analysis of arthroscopic treatment for hallux ganglion cyst deriving from ankle joint. Zhonghua Wai Ke Za Zhi. 2023;61(11):982-8.