10.20986/revesppod.2025.1719/2024
ORIGINAL
Winner Virginia Novel Award 2024
Comparative study of two conservative treatments for onychocryptosis: cotton packing vs. local corticosteroid injection
Estudio comparativo de dos tratamientos conservadores para la onicocriptosis, mechado de gasa vs. Infiltración local de corticoide
Angélica María Fernández Gómez1
Alfonso Martínez Nova1
María Teresa García Martínez2
1Universidad de Extremadura. Plasencia, Cáceres, España
2Universidad de Valencia, España
Abstract
Objectives: Although corticosteroid infiltrations have been employed in dermatology for various nail disorders, the efficacy of corticosteroid infiltration in improving clinical outcomes for patients with onychocryptosis remains unknown. Thus, the aim of this study was to evaluate the evolution of this disease with this treatment.
Patients and methods: A randomized clinical trial was conducted with a sample of 14 patients diagnosed with onychocryptosis. Participants were randomly assigned to either a control group (treated with spicule resection and gauze packing) or an experimental group (treated with spicule resection and corticosteroid infiltration). Baseline clinical status, pain, inflammation, and granuloma size were assessed before the intervention and at least one month after the procedure.
Results: One month post-treatment, the corticosteroid group showed a pain reduction of 6.5 ± 1.2 and an inflammation reduction of 1.4 ± 0.4 mm, whereas the gauze-wick group showed a pain reduction of 4.5 ± 2.5 and an inflammation reduction of 0.5 ± 0.3 mm, with statistically significant differences observed (p = 0.049 and p = 0.012, respectively).
Conclusion: Corticosteroid infiltration proved to be more effective than gauze-wick application in reducing pain and inflammation in patients with onychocryptosis. These findings support the clinical relevance of corticosteroid treatment as a therapeutic option for this condition.
Keywords: Onychocryptosis, foot, podiatry, spiculectomy, corticosteroid infiltration, conservative treatment
Resumen
Objetivos: Aunque las infiltraciones con corticoides se han empleado en dermatología para diferentes alteraciones ungueales, no se conoce la eficacia en pacientes con onicocriptosis. Por ello, el objetivo del estudio fue evaluar la evolución de la patología con este tratamiento.
Pacientes y métodos: Se llevó a cabo un ensayo clínico aleatorio con una muestra de 14 pacientes que padecían onicocriptosis, que fueron asignados al azar al grupo de control (espiculotomía y mecha de gasa) o grupo experimental (espiculotomía e infiltración de corticoide). Se valoró el estado clínico inicial, dolor, inflamación y tamaño del granuloma antes de la intervención y al menos un mes después de la misma.
Resultados: Tras un mes de tratamiento, el grupo corticoide presentó una reducción del dolor de 6,5 ± 1,2 y una reducción de la inflamación de 1,4 ± 0,4 mm, a la vez que, el grupo mechado presentó una reducción del dolor de 4,5 ± 2,5 y una reducción de la inflamación 0,5 ± 0,3 mm, presentando diferencias significativas (p = 0.049 y p = 0.012, respectivamente).
Conclusiones: La infiltración de corticoide mostró ser más efectiva que la aplicación de mecha de gasa en la reducción del dolor y la inflamación en pacientes con onicocriptosis. Estos hallazgos respaldan la importancia clínica del tratamiento con corticoide como opción terapéutica para esta afección.
Palabras claves: Onicocriptosis, pie, podología, espiculotomía, infiltración de corticoide, tratamiento conservador
Corresponding author
Alfonso Martínez Nova
podoalf@unex.es
Received: 14-11-2024
Accepted: 30-12-2024
Introduction
Onychocryptosis (ONC), commonly known as ingrown toenail, is a pathology affecting the nail apparatus, caused by compression of the nail plate onto the nail bed and/or the periungual fold, resulting in inflammation, hypersensitivity, erythema, and pain of varying intensity(1,2). The severity of the lesion is determined by the size and hypertrophy of the periungual folds, an important consideration as it guides the choice of treatment(1,3). Conservative treatments are typically employed in the early stages (Stages I and IIa), while surgical intervention—namely, the removal of the affected nail spicule along with the associated matrix portion—is recommended from Stage IIb onward, or when conservative approaches have failed(3,4).
The goal of conservative methods is to re-educate nail growth, with various techniques available, including spiculectomy, gauze wicking, acrylic nails, and plastic or metal orthonyxia, among others(5). Among these conservative techniques, one of the most commonly used by practitioners is the removal of the offending nail spicule, or spiculectomy, which involves excising the portion of the nail plate causing pain to relieve continuous pressure on the periungual fold. However, while this technique provides temporary pain relief, it does not resolve the underlying issue, with recurrence rates reported as high as 91.67 %(6). Gauze wicking may be added to spiculectomy, with the aim of separating the nail growth from its contact zone with the fold. Yet, this method also shows high recurrence rates, between 40-64 %, depending on the stage of the lesion6. Other conservative treatments, such as orthonyxia (plastic or metal) or acrylic nail application, appear to be more effective for onychocryptosis management but require good patient adherence to the treatment plan(4,6).
In recent years, a new conservative treatment option has emerged: intralesional corticosteroid injection into the affected hypertrophic canal. This approach aims to reduce inflammation in the periungual fold and support proper nail growth. This treatment has been tested in five cases with moderate lesion severity(7). In each case, an intralesional injection of triamcinolone was administered to the inflamed edge without spicule excision, with four patients requiring only a single injection to achieve satisfactory outcomes to avoid surgery, one patient underwent a total of 3 injections, successfully preventing surgical intervention. The outcomes were entirely positive and indeed avoided the need for surgical intervention(7). However, this study was limited to only 5 cases, making it insufficient to determine efficacy, as it lacked a control group. Therefore, the main objective of this research study is to verify whether the non-invasive treatment of spiculotomy combined with corticosteroid infiltration is clinically more effective than spiculotomy with gauze packing in the management of ingrown toenail pathology, aiming ultimately to avoid surgical treatment.
Patients and methods
This was a pilot comparative study, with a sample of 14 pa-tients—9 females and 5 males—aged between 14 and 61 years, who visited the University Podiatry Clinic at UEX (Plasencia, Cáceres) seeking treatment for onychocryptosis.
Inclusion and exclusion criteria
The study included patients with onychocryptosis presenting inflammation at stages IIa, IIb, or III, who sought treatment for their condition at the University Podiatry Clinic in Plasencia and agreed to participate by signing informed consent. Exclusion criteria were as follows: 1) patients under pharmacological treatment that could interact with anesthesia or corticosteroids, 2) patients with trypanophobia, 3) patients allergic to anesthesia or corticosteroids, 4) patients with paronychia, or 5) patients with onychocryptosis caused by increased curvature of the nail plate but without inflammation of the periungual fold.
Procedure
After the initial examination and diagnostic confirmation, participants were randomly assigned to one of two groups: the control group, which received gauze packing + spiculotomy (n = 7), or the corticosteroid group, which received corticosteroid infiltration + spiculotomy (n = 7). This random assignment was performed by the study supervisor prior to treatment and data collection, by previously assigning a random number (generated using the Random Number Generator app) to each of the patients’ record sheets.
A custom data collection sheet was designed specifically for this study, which included the following information: patient number, personal data, weight, height, body mass index, type of technique used (gauze packing or corticosteroid), gender, affected foot, affected toe number, and the involved nail fold.
Pain assessment was conducted using the Visual Analog Scale (VAS) via the Visual Scale App. In this method, the patient described the intensity of their pain using a color gradient scale. The scale ranges from green, indicating mild pain, through yellow, representing moderate pain, to red, denoting severe pain. The patient selects the color that best reflects their pain experience by clicking on the corresponding section of the scale. This assessment was performed twice to obtain an average value quantifying the pain intensity associated with the condition (Figure 1).
Figure 1. Screenshot of the Visual Scale App to illustrate the assessment process.
Inflammation assessment was conducted using a digital caliper and a straight metal spatula. The spatula was carefully inserted between the periungual fold and the nail plate, with the precise distance measured from the edge of the spatula to the point covered by the periungual fold, thereby obtaining an exact measurement of the millimeters of periungual fold inflammation extending into the nail plate (Figure 2).
Treatment Application:
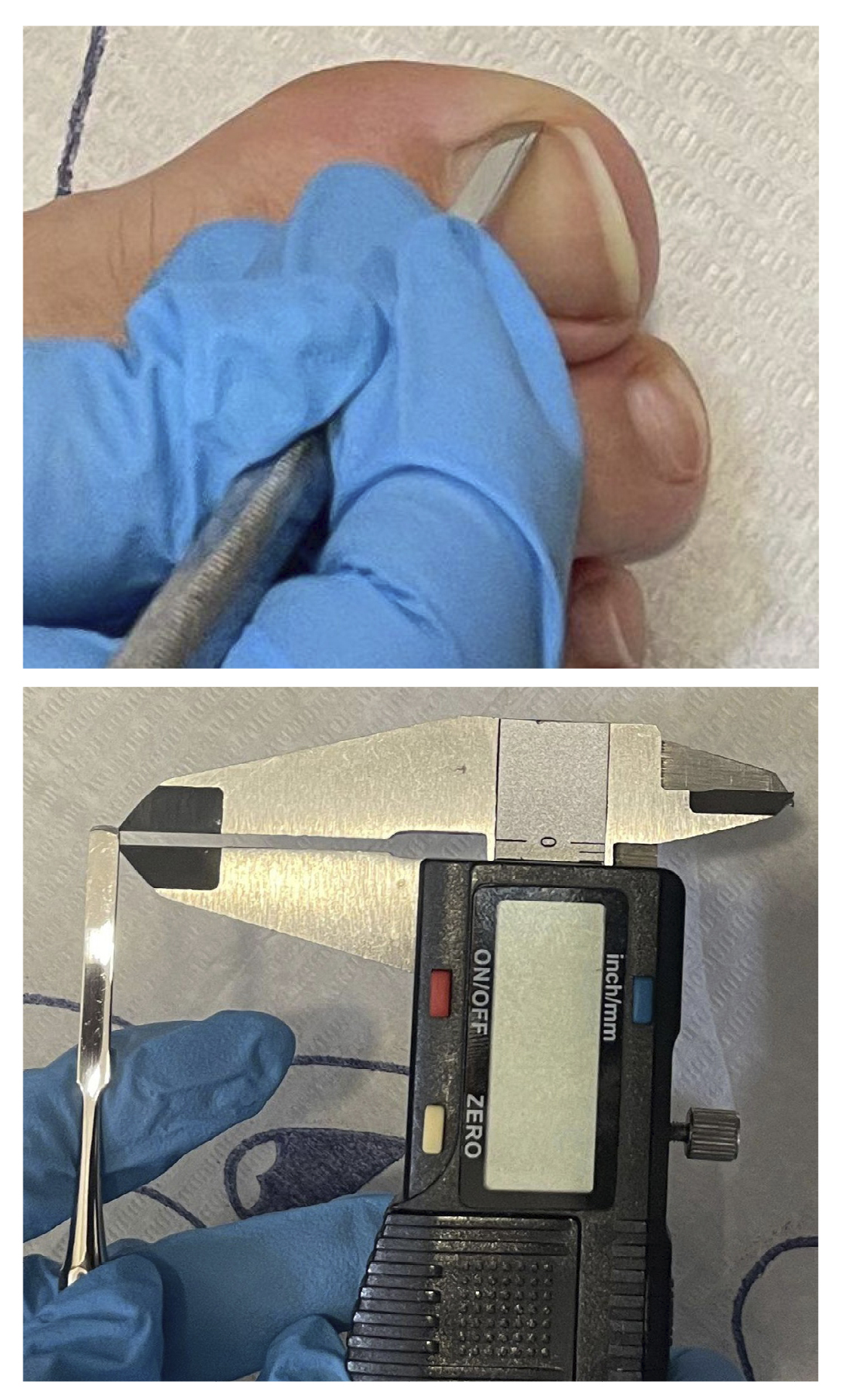
Figure 2. Visual representation of the measurement procedure of the fold affecting the nail plate.
Group 1 (control): Spiculotomy and gauze packing were performed. After disinfecting the area with povidone-iodine, the spicule was removed by cutting the nail plate segment embedded in the periungual fold. This procedure was conducted using a nail clipper, Adson forceps, and a #15 scalpel blade. Next, a small piece of gauze soaked in povidone-iodine or saline solution was placed under the nail using a gouge and forceps. If necessary, topical cryoanesthesia was applied before spicule removal to alleviate potential discomfort. Finally, the area was covered with gauze and Hypafix after applying povidone-iodine (Figure 3).
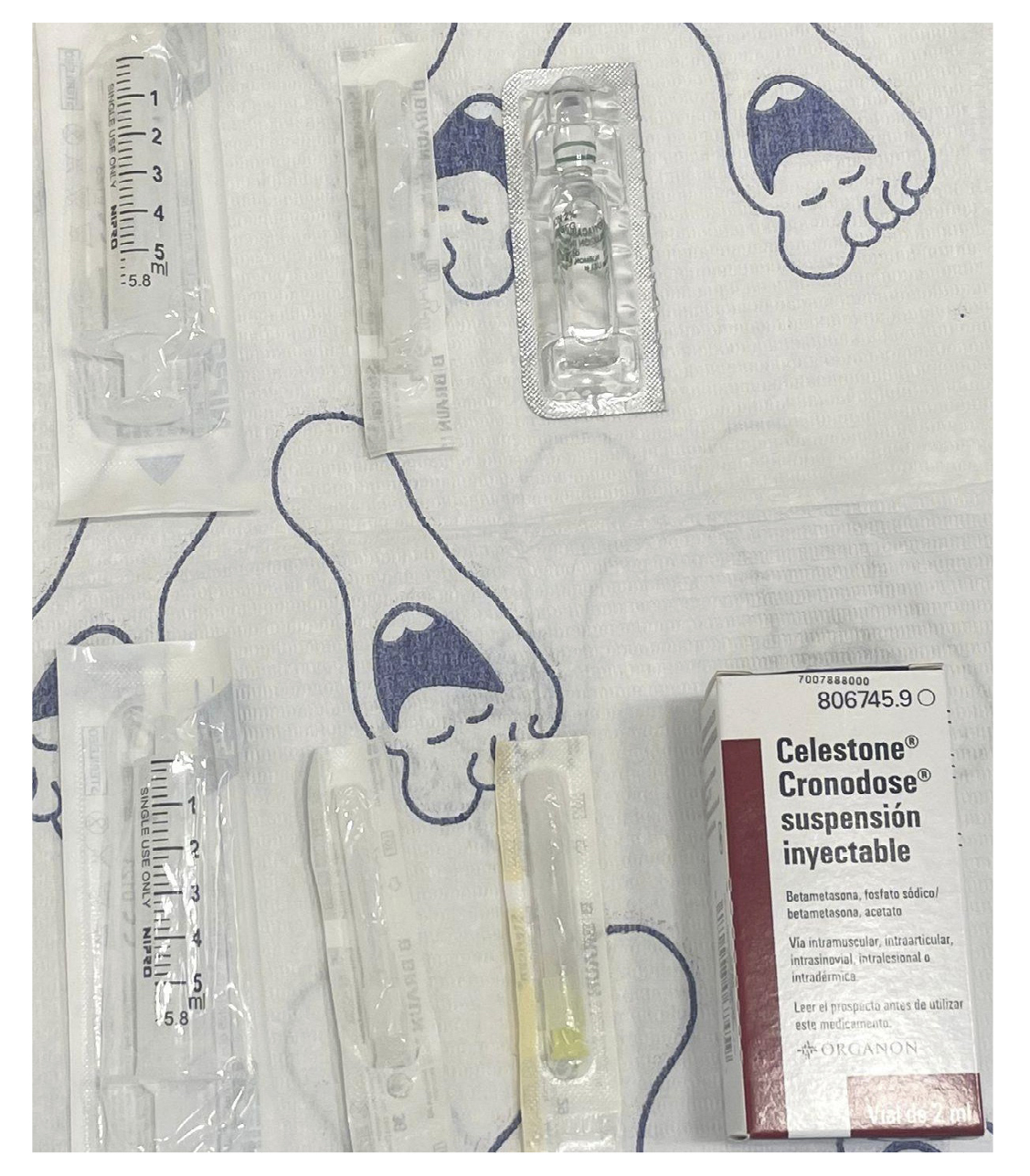
Figure 3. Visual representation of materials used in the corticosteroid injection procedure.
Group 2 (experimental): Spiculotomy and corticosteroid infiltration were performed. For this treatment, we used betamethasone (phosphate + acetate) , a medication suitable for intralesional administration and indicated for dermatological lesions and inflammatory and cystic disorders of the foot. After disinfecting the area, the affected canal was anesthetized with 1 cc of 2 % mepivacaine to prevent pain during the procedure. Once the anesthesia took effect, the embedded nail segment was removed using a nail clipper, Adson forceps, and a #15 scalpel blade. An intralesional corticosteroid injection was then administered to the area of maximum inflammation, consisting of 0.3 cc to 0.5 cc of betametasone (depending of the hallux size) combined with approximately 0.2 cc of 2 % mepivacaine (Figure 4). This injection was performed using an insulin needle, with a single puncture, depositing the corticosteroid-with anesthetic mix along the entire inflamed canal as the needle was gradually withdrawn. Lastly, povidone-iodine was applied, and the area was closed with gauze and hypafix.

Figure 4. Corticosteroid infiltration procedure.
Follow-up and Review. The first follow-up review was scheduled approximately one week after the initial treatment. During this review, a visual assessment of the lesion was performed to monitor its progression. The final review was conducted approximately one month after the initial treatment, during which the same data as in the initial assessment (pain, inflammation, etc.) were collected to evaluate the treatment’s effectiveness.
Statistical analysis
Two new variables were created to enable comparisons between groups: Delta Pain (pre-post pain) and Delta Inflammation (initial-final inflammation). These variables reflect the reduction in both pain and periungual fold inflammation resulting from the treatment (indicating how much the inflammation in the lesion decreased). A descriptive analysis of the variables was performed (mean ± SD). To compare variables between groups (such as gender or treatment group), Student’s t-test for independent samples was applied. A contingency table with a chi-square test was used to compare estimated proportions between variables and their differences. Statistical analyses of the results were conducted using SPSS software, version 29.0 (UEX campus license). A significance level of 5 % was established.
Results
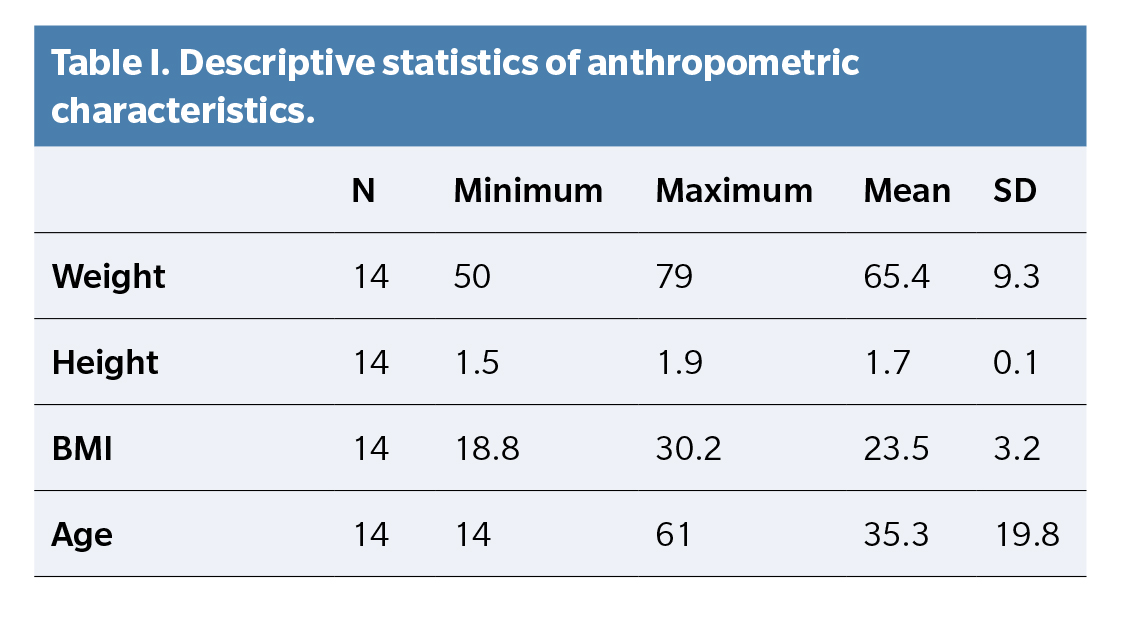
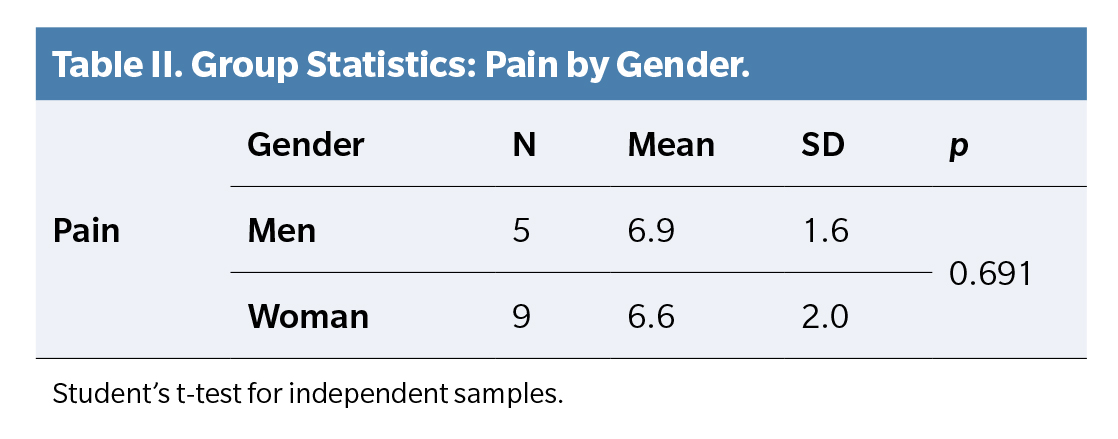
The inal sample consisted of 14 patients with a mean weight of 65.4 ± 9.2 kg, a mean height of 1.7 ± 0.1 m, a mean body mass index (BMI) of 23.5 ± 3.2 kg/m2, and an mean age of 35.3 ± 19.8 years. Minimum and maximum values of these variables are shown below (Table 1). Out of the 14 patients, 6 presented ONC in the right foot and 8 in the left. Nine patients had an affected peroneal fold, while five showed tibial fold involvement. The initial stages were distributed as follows: seven patients in stage IIa and another seven in stage IIb. The average pain level in the entire group was 6.6 ± 1.8, with a minimum of 2.1 and a maximum of 8.9. Pain analysis by gender showed a mean of 6.9 ± 1.6 in men and 6.6 ± 2.0 in women, with no statistically significant differences (p = 0.691) (Table 2).
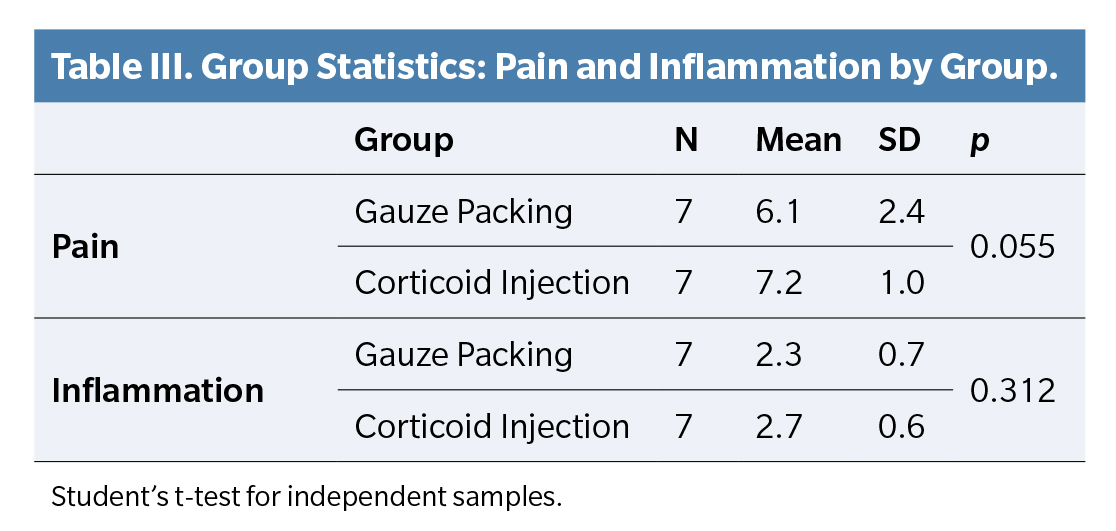
Comparing initial pain between groups, the gauze-packing group showed an average pain of 6.1 ± 2.4, while the corticosteroid group averaged 7.2 ± 1, with no statistically significant differences (p = 0.055). For inflammation, the gauze-packing group had a mean of 2.3 ± 0.7 mm, and the corticosteroid group averaged 2.7 ± 0.6 mm, also with no significant differences (p = 0.312) (Table 3).
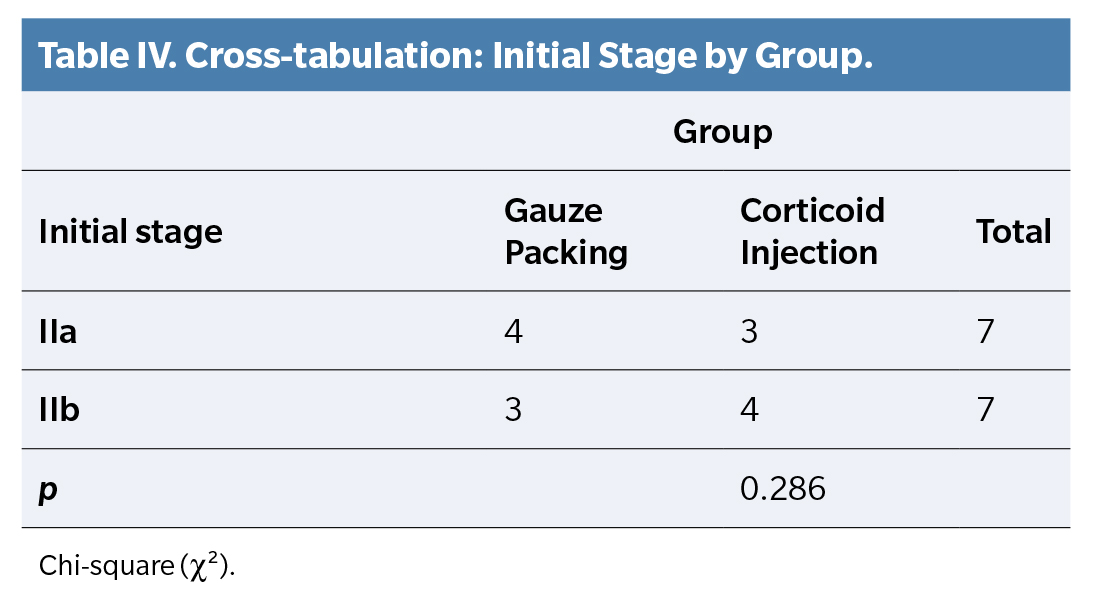
Among the seven patients with an initial IIa stage, four were assigned to the gauze-packing group and three to the corticosteroid group. For those in stage IIb, three were allocated to the gauze-packing group and four to the corticosteroid group. The initial stage results by group showed no statistically significant differences (p = 0.286) (Table 4).
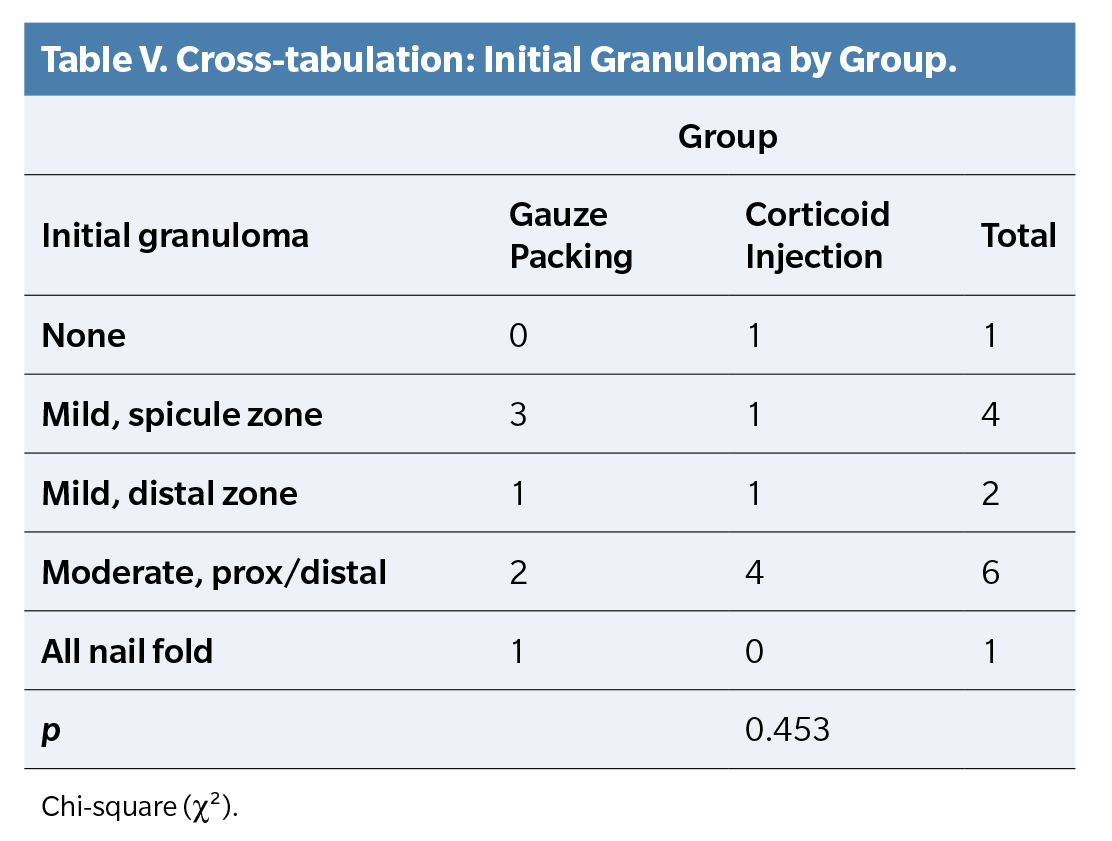
Regarding initial granuloma, mild granuloma was observed in the spicule area in three cases from the gauze-packing group and one case in the corticosteroid group. A moderate initial granuloma, both proximal and distal, was seen in two cases in the gauze-packing group and four cases in the corticosteroid group. The size of the initial granuloma showed no significant differences between groups (p = 0.453) (Table 5).
Clinical effectiveness evaluation: pain, inflammation, and granuloma
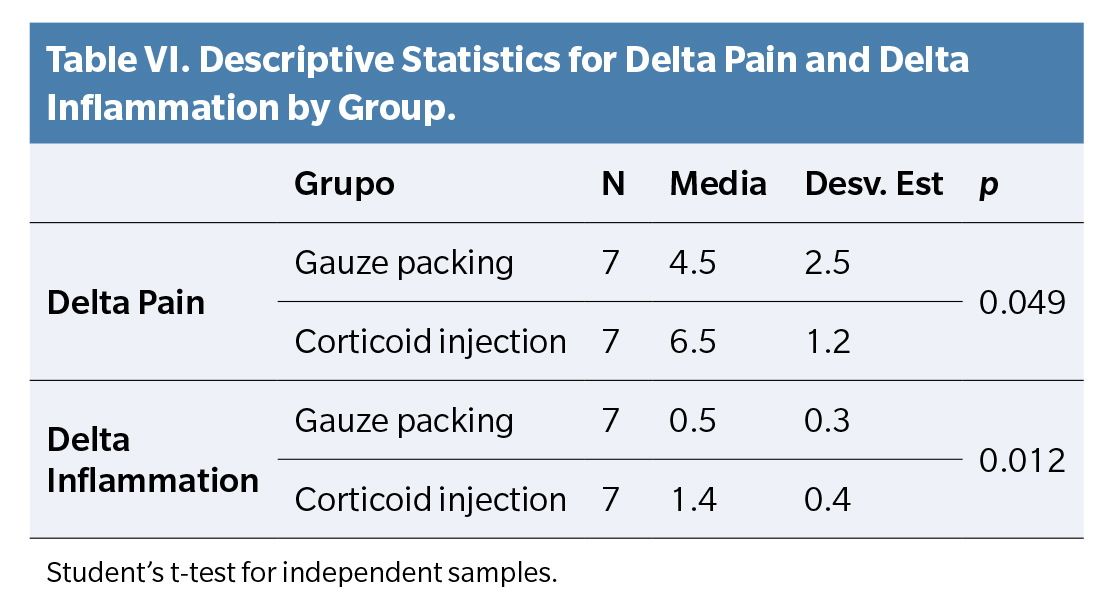
The variable Delta Pain (pre-post pain) showed a mean of 4.5 ± 2.5 in the gauze-packing group and 6.5 ± 1.2 in the corticosteroid group, with this difference being statistically significant (p = 0.049). For Delta Inflammation, the corticosteroid group showed a mean reduction of 1.4 ± 0.4 mm compared to 0.5 ± 0.3 mm in the gauze-packing group, indicating statistically significant differences (p = 0.012) (Table 6).
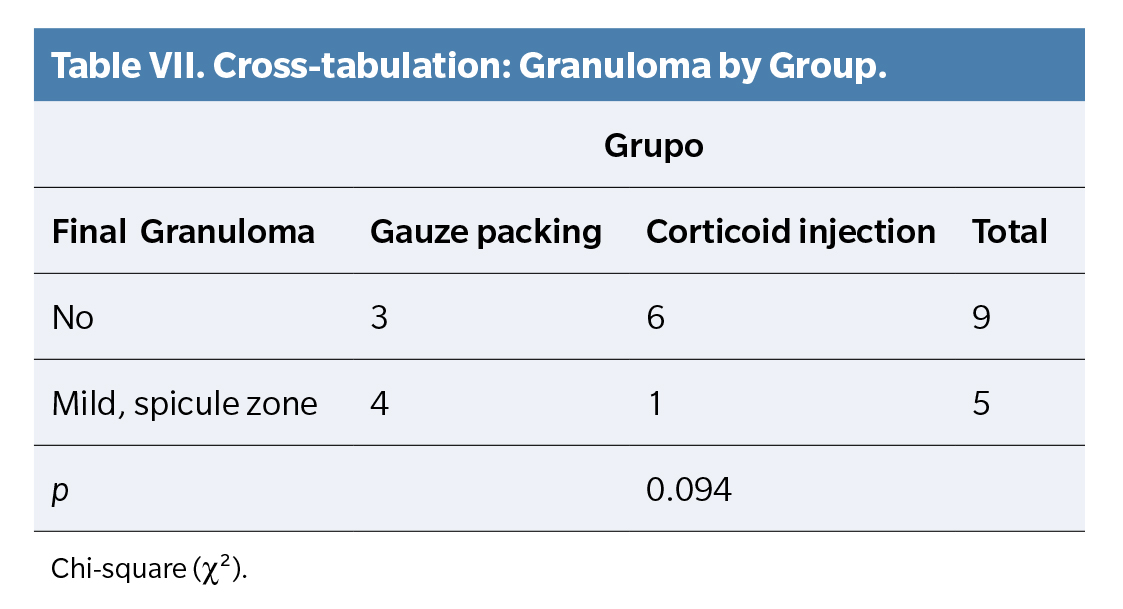
Final granuloma results showed either none or mild granuloma in the spicule area across both groups. No granuloma was observed in six cases from the corticosteroid group and three cases from the gauze-packing group, totaling nine cases. Mild granuloma in the spicule area was observed in four cases from the gauze-packing group and one case from the corticosteroid group, totaling five cases. Final granuloma results by group showed no significant differences (p = 0.094) (Table 7).
Satisfaction and recurrence
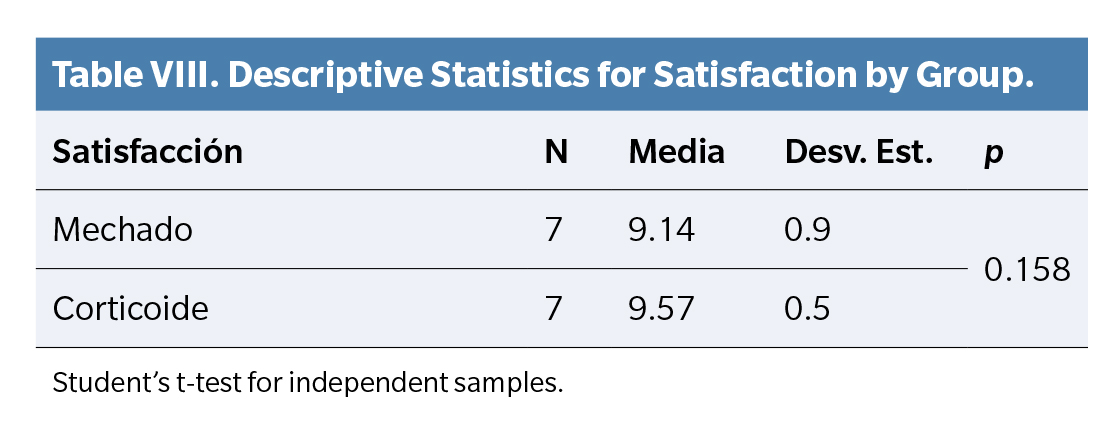
In satisfaction results by group, the gauze-packing group averaged 9.14 ± 0.90, while the corticosteroid group averaged 9.58 ± 0.54, with no statistically significant differences (p = 0.158) (Table 8).
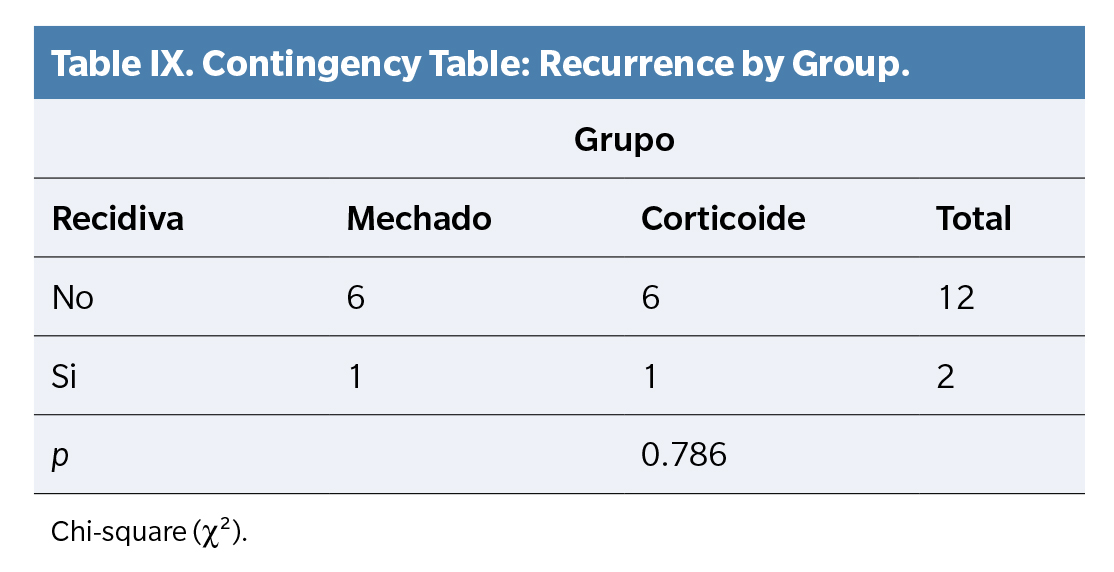
Recurrence results by group were as follows: six cases in the gauze-packing group and six in the corticosteroid group showed no recurrence, while one case in each group showed positive recurrence. In total, 12 patients did not experience recurrence, while two did. Recurrence results showed no significant differences (p = 0.786) (Table 9)
Discussion
Upon analyzing the results, we observe that the initial clinical condition of the patients was very similar across both groups. Although clinical improvements were seen in all patients, the group receiving corticosteroid infiltration demonstrated a greater reduction in both pain and inflammation compared to the group treated with gauze packing.
The symptomatic improvement observed in the gauze-packing group may be attributed to the effect of spiculectomy and gauze strip placement, which helps to separate the nail from the periungual tissue, potentially providing mechanical relief from pain and inflammation. However, this treatment lacks the active pharmacological properties of corticosteroids in reducing inflammation and pain. The intralesional administration route of the corticosteroid injection may also explain the observed differences, as it directly delivers the medication to the affected periungual area, resulting in a more intense and rapid effect.
However, it is important to note that the corticosteroid group did not show a significantly lower recurrence rate compared to the control group. This suggests that a single injection may not be effective in preventing recurrent onychocryptosis. Our study’s results did not reach the same success level as a previously published study with five cases, in which the recurrence rate was zero(7). Unlike our approach, Vílchez(7) employed multiple injections based on need and extended the follow-up period beyond our study’s timeframe. In Vílchez’s study, a single infiltration sufficed in four cases, whereas consecutive infiltrations every three weeks were necessary in one case. The follow-up period in Vílchez’s study ranged from 6 months to 3 years, while our study was conducted over a shorter term.
A notable advantage of our study lies in the inclusion of a control group receiving standard treatment (spiculectomy and gauze packing), in contrast to the experimental group receiving corticosteroid infiltration along with spiculectomy. This strategy enabled a direct comparison between the effects of the experimental and conventional treatments, enhancing the value of our findings and offering a more comprehensive perspective on the intervention’s efficacy.
Several of our patients experienced significant clinical improvement, which, in the author’s opinion, was noticeably better in the corticosteroid group, although this was not reflected in the recurrence results (Figure 5). Additionally, as corticosteroids significantly reduce pain, we consider this a therapeutic advantage, particularly for patients experiencing acute and intense pain, who may require rapid relief.

Figure 5. Clinical Case Example from Corticosteroid Group.
This study has certain limitations, and the results should be interpreted with caution. The sample size was small, constrained by the limited time available for the study. Additionally, recurrence was defined as any patient requiring a return visit, even if their clinical condition was improved compared to the start of treatment. Another point to consider is that only one infiltration was administered per affected canal due to the short-term nature of the study. If a single injection with a one-month follow-up effectively reduced pain and inflammation, continuing with this regimen and extending the follow-up period could potentially eliminate symptoms and improve recurrence rates. The referenced bibliography is also limited due to the scarcity of articles published to date addressing this topic.
For future research, it would be beneficial to conduct long-term follow-ups to evaluate the durability of the results and to include a larger sample size to further validate the findings. Moreover, exploring additional treatment aspects, such as the incidence of side effects or comparisons with alternative treatments, could provide a more comprehensive view of the therapeutic options available for patients with onychocryptosis.
In conclussion, the patients in this study began with a similar clinical condition in both groups. Corticosteroid infiltration is more effective in reducing pain and inflammation in the periungual fold associated with onychocryptosis. Although corticosteroid treatment does not improve the recurrence rate, it emerges as a valid therapeutic option.
Ethics Declaration
Patients provided both oral and written consent (informed consent) to participate. The study was approved by the Bioethics and Biosafety Committee of the University of Extremadura with code 184//2023.
Author’s Contribution
Study conception and design: AMN, MTGM.
Data collection: AMFG.
Analysis and interpretation of results: AMN.
Drafting, writing, and preparation of the manuscript: AMFG.
Final review: AMN, MTGM.
Funding
None.
Conflicts of Interests
Authors declare no conflicts of interest related to the present paper.
References
- González-Hernández WC, Enríquez-Merino J, Alcalá-Pérez D, Medina-Bojórquez A, Torres-González S, Martínez-Estrada V, et al. Tratamiento quirúrgico de onicocriptosis con puente cutáneo. Presentación de tres casos. Rev Cent Dermatol Pascua. 2022;31(1-2):43-7. DOI: 10.35366/107801002E
- Sánchez Hernández S, Giralt de Veciana E. Vista do Bloqueo digital anestésico con técnica V versus técnica H en onicocriptosis infectadas del primer dedo del pie. Rev Iberoam Pod. 2020;2(2):190-5. DOI: 10.36271/iajp.v2i2.31. DOI: 10.36271/iajp.v2i2.31.
- López-Llunell C, Leal Canosa L, Garbayo-Salmons P, Gamissans-Cañada M, Ribera Pibernat M. La onicocriptosis y su tratamiento. Piel (Barc). 2022;37(1):47-55. DOI: 10.1016/j.piel.2021.04.023.
- Martínez MTG, Gómez-Gabriel B, Martínez-Nova A, Gil PN. Comparative study between nail retraining with gauze bandaging and the nail remodeling with acrylics as a conservative treatment for stage I and IIa onychocryptosis. J Cosmet Dermatol. 2023;22(3):916-20. DOI: 10.1111/jocd.15512.
- Chabchoub I, Litaiem N. Ingrown Toenails. StatPearls Publishing (Island); 2022.
- Márquez Reina S, Lafuente Sotillos G, Domínguez Maldonado G. Estudios conservadores de la onicocriptosis. Revisión bibliográfica. Rev Esp Podol. 2018;29(1);34-42. DOI: 10.20986/revesppod.2018.1504/2018. DOI: 10.20986/revesppod.2018.1504/2018.
- Vílchez-Márquez F, Morales-Larios E, del Río de la Torre E. Tratamiento no quirúrgico de las uñas encarnadas con infiltración local de triamcinolona. Actas Dermosifiliogr. 2019;110(9):772-3. DOI: 10.1016/j.ad.2018.02.042.