10.20986/revesppod.2025.1718/2024
REVIEW
Effectiveness of the use of bone cement in the treatment of diabetic foot osteomyelitis
Efectividad del uso de cemento óseo en el tratamiento de osteomielitis en pie diabético
Alicia Fernández-Osuna1
Mateo López-Moral2
Marta García-Madrid2
Raúl J. Molines-Barroso2
Yolanda García-Álvarez2
José Luis Lázaro-Martínez2
1Estudiante Máster Formación Permanente en Pie Diabético. Facultad de Enfermería, Fisioterapia y Podología. Universidad Complutense de Madrid, España
2Unidad de Pie Diabético. Clínica Universitaria de Podología. Facultad de Enfermería, Fisioterapia y Podología. Universidad Complutense de Madrid, España
Abstract
The presence of osteomyelitis in the diabetic foot presents a significant challenge in terms of healing, increasing the risk of serious complications and potentially leading to amputations. Antibiotic bone cement has emerged as a promising alternative, offering favorable results in eradicating infections, accelerating healing, and preserving limbs. Its mechanism of action combines local and sustained release of antibiotics, filling of bone cavities, and stimulation of bone growth. The present paper is bibliographic review about studies that evaluate its efficiency in combination with other therapies, showing positive results in the eradication of infections, the reduction of hospitalization time and the preservation of limbs. Bone cement has been effective in treating forefoot infections and ulcers in Charcot‘s foot. In addition, it has proven to be an effective complement in surgery for the reconstruction and treatment of osteomyelitis.
Keywords: Osteomyelitis, diabetic foot, bone cement, diabetic foot ulcer, Charcot foot
Resumen
La presencia de osteomielitis en el pie diabético presenta un desafío significativo en términos de curación, aumentando el riesgo de complicaciones graves y pudiendo derivar en amputaciones. El cemento óseo con antibióticos ha surgido como una alternativa prometedora, ofreciendo resultados favorables en la erradicación de infecciones, aceleración de la curación y preservación de extremidades. Su mecanismo de acción combina la liberación local y sostenida de antibióticos, el relleno de cavidades óseas y la estimulación del crecimiento óseo. El presente trabajo realiza una revisión bibliográfica sobre los estudios que han evaluado su eficacia en combinación con otras terapias, mostrando resultados positivos en la erradicación de infecciones, la reducción del tiempo de hospitalización y la preservación de extremidades. El cemento óseo ha sido efectivo en el tratamiento de infecciones del antepié y úlceras en el pie de Charcot. Además, ha demostrado ser un complemento con resultados prometedores en la cirugía para la reconstrucción y tratamiento de la osteomielitis.
Palabras clave: Osteomielitis, pie diabético, cemento óseo, úlcera pie diabético, pie de Charcot
Corresponding author
Mateo López-Moral
matlopez@ucm.es
Received: 05-11-2024
Accepted: 15-01-2025
Introduction
Diabetic foot is a serious complication of diabetes mellitus (DM), affecting millions of people worldwide(1,2). It is characterized by the presence of ulcers and infections that can lead to amputations if not treated appropriately(3). Osteomyelitis, a bone infection, is one of the most common and severe complications in patients with diabetic foot4. This condition can result in significant loss of quality of life and high healthcare costs(5,6,7).
Bone cement, traditionally used in orthopedic surgery for the fixation of implants and fracture repair, has shown potential for treating bone infections associated with diabetic foot7,8. This material not only provides mechanical support to the compromised bone structures but also acts as a vehicle for the sustained release of antibiotics at the site of infection, which is crucial for fighting the infection and preventing its recurrence, especially in areas where blood flow is compromised due to peripheral arterial disease (PAD), common in these patients(9,10).
In addition to its role in antibiotic administration, bone cement helps stabilize the ulcer site and facilitates the growth of new bone tissue, accelerating healing(11,12). Some studies also suggest that bone cement can be integrated with other therapies, such as negative pressure therapy, to improve clinical outcomes(13,15).
The diagnosis of osteomyelitis in diabetic foot is based on clinical, radiological, and laboratory assessments, making timely identification of the infection crucial for appropriate treatment16. In cases where the infection is severe, combining surgery with antibiotic-impregnated bone cement has shown a high success rate in limb preservation, preventing amputations(17,18).
This paper aims to analyze the potential of bone cement to facilitate bone regeneration, promote angiogenesis, and release antibiotics locally in cases of osteomyelitis in diabetic foot by menas of a bibliographic review. It is expected that these properties will contribute to controlling the infection and accelerating healing, which could translate into improved quality of life for patients.
Material and methods
Bibliographic Search
A search was conducted across 3 electronic databases to find relevant studies on the effectiveness and use of bone cement for the healing of diabetic foot ulcers. The review was conducted from March 1st, 2024, to April 21st, 2024. Key terms used were “diabetic foot ulcer”, “osteomyelitis”, “bone cement”, and “diabetic foot”. These terms were combined using the Boolean operator “AND”, forming search strategies such as: “bone cement AND diabetic foot ulcer”, “bone cement AND osteomyelitis”, and “bone cement AND diabetic foot”. The flow diagram of the search method is presented in Figure 1.
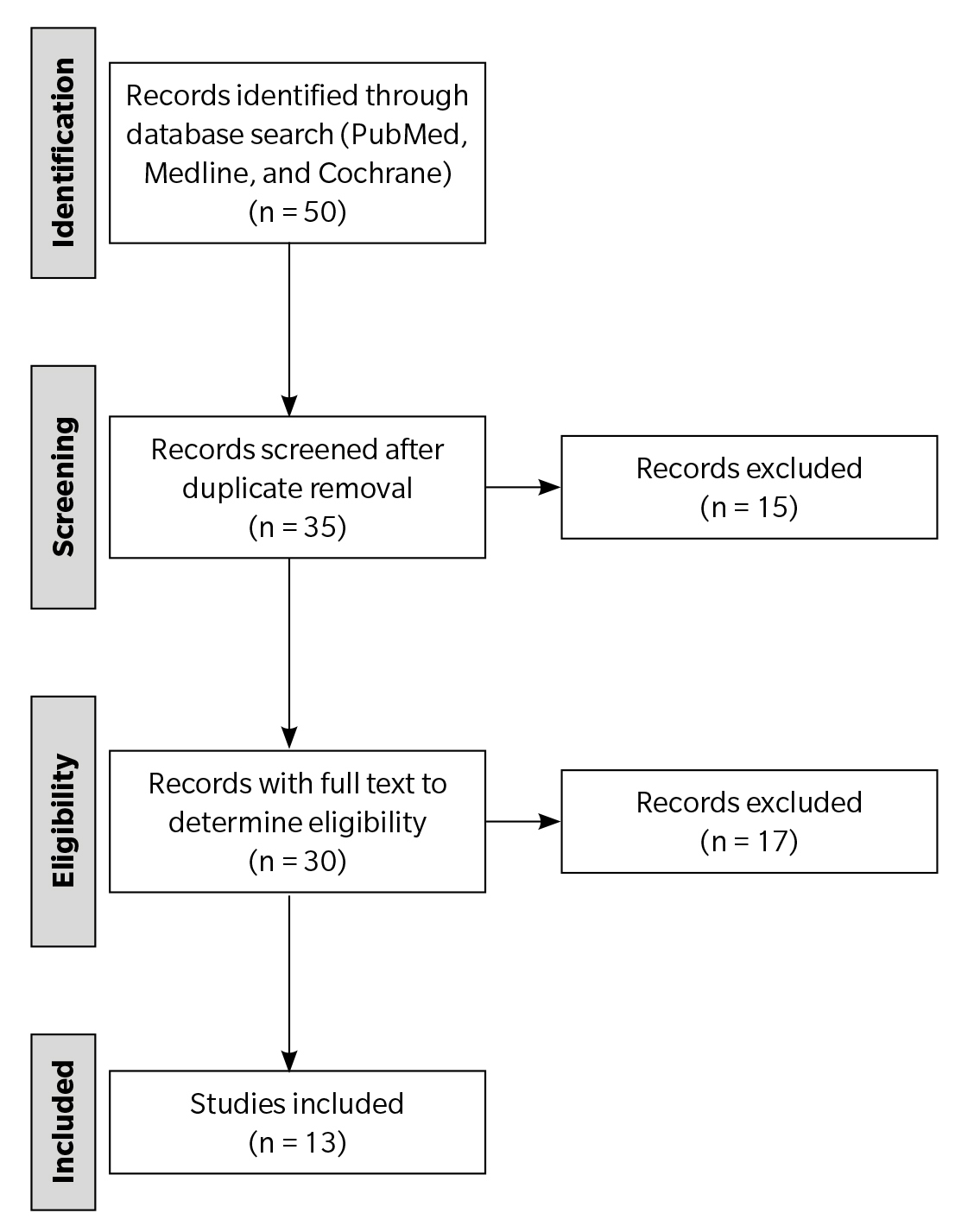
Figure 1. Flowchart of the selection, classification, and validation of the chosen articles.
Selection criteria
Inclusion criteria
Inclusion criteria were articles published between 2010 and 2024 in spanish, english, chinese, german, Italian, and portuguese. The types of articles included were meta-analyses, randomized controlled trials, journal articles, comparative studies, and case studies related to the use of bone cement in the treatment of complications and/or injuries of the diabetic foot, studies that combined bone cement with other treatment methods, such as flaps or vacuum-assisted closure and studies where the subjects had ulcers with osteomyelitis.
Exclusion criteria
Exclusion criteria were studies focused on venous pathology and not directly related to the use of bone cement for the treatment of diabetic foot, letters to the editor, editorials, comments, or reports. documents published before 2010 and studies where treatments for osteomyelitis did not involve bone cement.
Literature selection and data extraction
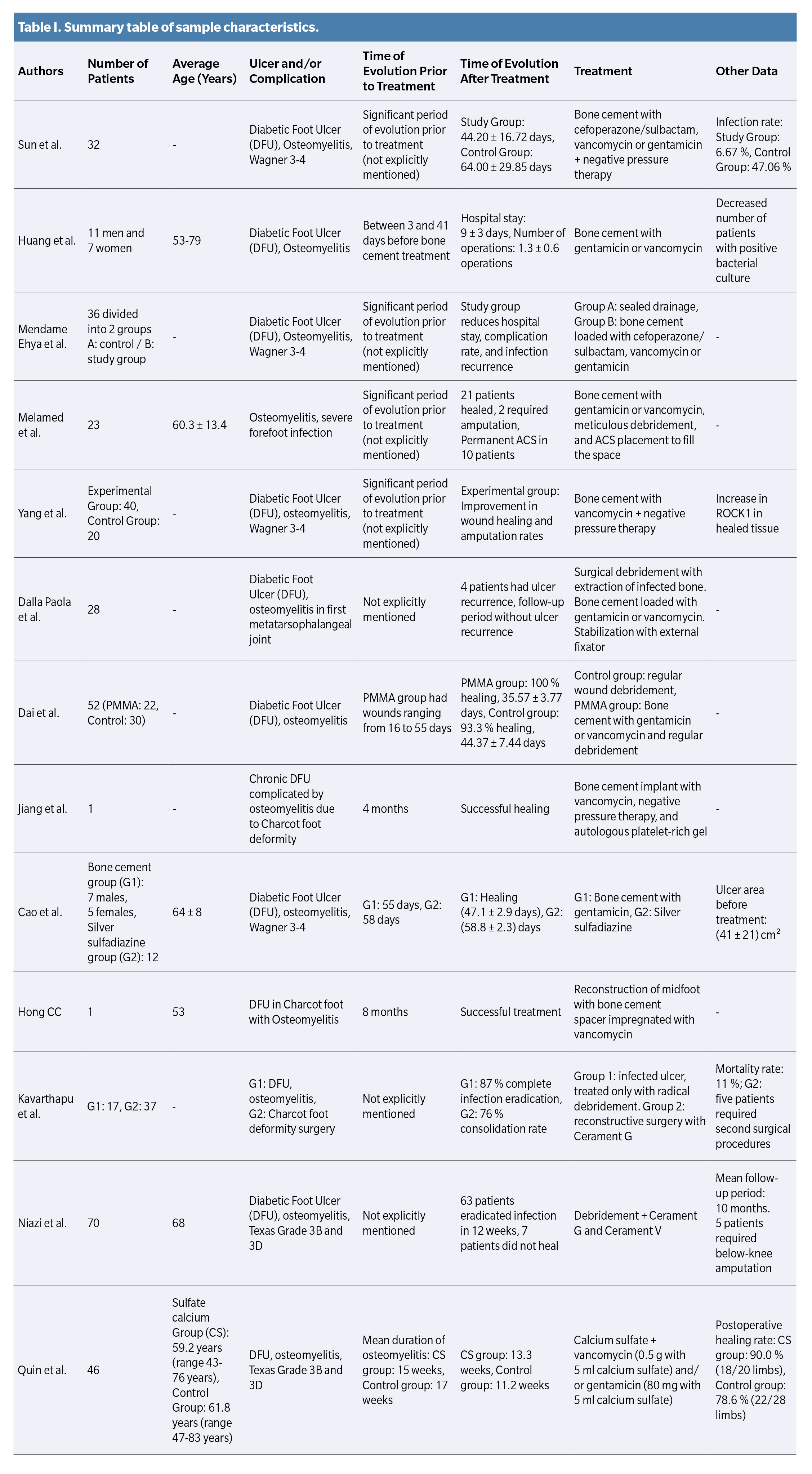
One of the authors of the article selected the relevant literature, based on the inclusion criteria, for the study. Based on our research questions, a data table was created to record the authors, year, journal, study design, objectives, and outcomes of each article. Additionally, an attached table was created summarizing the lesion characteristics, duration, and treatment of each study (Table 1).
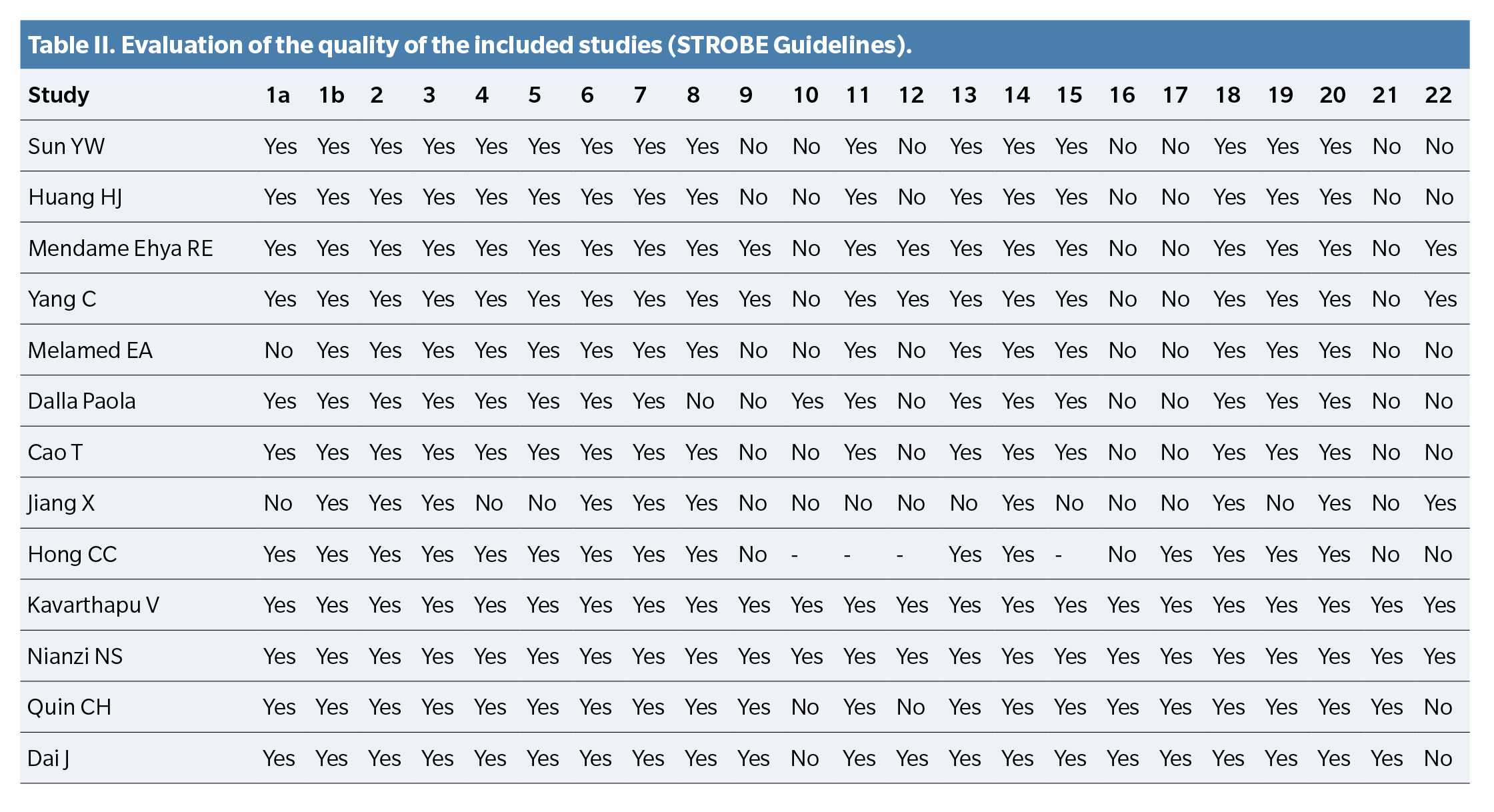
Quality assessment of the included studies (STROBE Guidelines)
The data collected from all articles were analyzed. Since most of the included articles were retrospective studies and randomized controlled trials, the quality assessment was based on the standard STROBE guidelines to ensure high-quality presentation of observational studies. The evaluators assessed the adequacy of the reported elements using the STROBE checklist, which provides a framework for integrity and transparency. The STROBE checklist has 22 items, including items 1 (title and abstract), 2 and 3 (introduction), 4-12 (methods), 13-17 (results), 18-21 (discussion), and 22 (funding and sponsorship). The results of the analysis are found in Table 2.
Analysis
Given the high heterogeneity in the study designs, survey times, and outcome indicators of the included studies, conducting a quantitative analysis was difficult. Therefore, only qualitative analyses were performed.
Results
Literature retrieval
Once the inclusion and exclusion criteria were applied, a total of 13 articles were selected. Appendix 1 shows the figure representing the article selection process through a flowchart.
Characteristics of the included studies
A total of 13 documents published between 2012-2024 are included. These consist of: 3 randomized controlled trials, 3 retrospective trials, 1 multicenter trial, 2 case studies, 2 comparative studies, 1 cohort study, and 1 clinical trial.
The 13 articles include a total of 444 patients with diabetic foot ulcers complicated by osteomyelitis. The etiology of the lesions was neuroisquemic in nature in most cases, although some articles also included neuropathic and ischemic diabetic foot ulcers (DFU).
Sun YW et al. (19), in their retrospective study, demonstrated the superiority of combining antibiotic-impregnated bone cement and vacuum-assisted closure (VAC) therapy in treating Wagner 3-4 ulcers. The findings indicated that the mean healing time in the study group (44.20 ± 16.72 days) was shorter than in the control group (64.00 ± 29.85 days) (p < 0.05). The infection rate in the study group 10 days after surgery was lower vs the control group (6.67 %, 47.06 %, p < 0.05). No statistically significant differences were observed between the two groups regarding complications such as bleeding and necrosis. This therapeutic combination resulted in a significant reduction in healing time and a notably lower infection rate compared to conventional treatments. The results of this study highlight the potential of this strategy to improve clinical outcomes in patients with severe DFUs.
Huang HJ et al. (20) noted that antibiotic bone cement treatment was effective in reducing the number of patients with bacteria in postoperative lesions, as well as decreasing the need for additional surgical interventions. Additionally, a reduction in hospital stay duration was observed in patients treated with this procedure.
In a randomized controlled trial, Mendame Ehya Re et al. (21) compared the effectiveness of antibiotic-impregnated bone cement with traditional treatment in patients with osteomyelitis linked to diabetic foot infection concerning their primary outcome. The findings showed that, in patients with diabetic foot ulcers complicated by osteomyelitis, the application of antibiotic-impregnated bone cement notably accelerated lesion healing, reducing the average time to complete healing and, consequently, hospital stay. Furthermore, a significant reduction in pain and greater expulsion of infectious agents were observed vs the control group, which was treated with vacuum drainage.
Yang C et al. (22) provided a new perspective by investigating the molecular mechanisms underlying the action of bone cement. The study compared 2 therapies for DFUs: one including bone cement, antibiotics, and negative pressure therapy, and the other using only negative pressure therapy. The findings indicated that the first group, which underwent treatment with bone cement and antibiotics, showed a considerably faster healing rate, a reduced amputation rate, and lower levels of inflammation. Additionally, a reduction in bacterial presence in the lesions of this group was recorded. This suggests that the combination of bone cement with antibiotics and negative pressure therapy may be a more effective strategy for treating diabetic foot ulcers and promoting healing, thus reducing the need for amputation.
Melamed Ea et al. (23) evaluated the efficacy of antibiotic-impregnated bone cement in the treatment of osteomyelitis and severe forefoot infection. The study compared two methods for relieving diabetic foot ulcers with bone infection (osteomyelitis): the application of antibiotic-impregnated bone cement and vacuum drainage. The findings indicated that bone cement with antibiotics was significantly more effective in promoting lesion healing, reducing pain, shortening hospital stays, and decreasing the need for dressing changes. Additionally, this treatment led to a more effective elimination of the bacteria responsible for the infection. In conclusion, the research suggests that antibiotic-impregnated bone cement is a promising therapeutic alternative for treating diabetic foot ulcers with osteomyelitis, providing superior clinical outcomes compared to vacuum drainage.
The study by Dalla Paola et al. (24) focuses on the use of bone cement in patients with first ray ulcers and positive Probe to Bone test (PTB). The study showed a high success rate in wound healing, reaching 96.4 % of treated patients. However, certain problems were detected, such as wound dehiscence (opening of the incision), ulceration at the surgical site, and recurrence of absence of blood flow in the tissue (critical ischemia), which affected a relatively small percentage of patients. Furthermore, a small group of patients required partial foot amputation, and certain deformities in the toes were reported. Overall, the findings suggest that the conservative method presented could be a feasible alternative for treating diabetic foot ulcers with bone infection in the big toe. However, further research is needed to corroborate these findings and evaluate the benefits and risks of this procedure.
Cao T et al. (25) compared the effectiveness of gentamicin-based bone cement and silver sulfadiazine in the treatment of diabetic foot ulcers. The findings indicated that the antibiotic-impregnated bone cement was significantly more effective in promoting the healing of lesions, reducing pain, hospital stay, and the need for bandage modifications. Additionally, this treatment led to a more effective elimination of the bacteria responsible for the infection.
Dai J et al. (26) examined the use of bone cement combined with debridement versus debridement alone. The study’s findings revealed that the group treated with PMMA (polymethyl methacrylate) exhibited a significantly higher wound healing rate (100 %) compared to the control group (93.3 %). Furthermore, the mean healing time was shorter in the PMMA group (35.32 days) vs the control group (44.37 days). Regarding debridement methods, a lower average number was required in the PMMA group (1.50) vs. the control group (2.13). Finally, a lower amputation rate was recorded in the PMMA group, with 5 minor amputations, in contrast to the control group, which had 8 minor amputations and 2 major amputations.
Through a clinical case, Jiang X et al. (27) illustrated the importance of biomechanical evaluation and the use of therapeutic footwear in the treatment of diabetic foot ulcers. The treatment included surgical removal of necrotic tissue, the application of antibiotic-impregnated bone cement to combat the infection, and negative pressure wound therapy (NPWT) to promote healing. Additionally, platelet-rich organic gel (APG) was used to stimulate tissue regeneration. After 5 months of therapy, the ulcer completely healed, and no recurrence was recorded during follow-ups at 1 month and 1 year.
Hong CC et al. (28) presented a clinical case where a combination of surgical techniques, including the use of antibiotic-impregnated bone cement, was used to treat a complicated Charcot deformity. The research findings indicate that foot reconstruction through subtalar fusion with an antibiotic-impregnated bone cement spacer, along with an adipofascial flap to fill the tissue defect, was successful. At 8-12 weeks post-surgery, bone union was observed in the tibio-calcaneal fusion, and the complete healing of the flap allowed the patient to gradually begin weight-bearing. At 6 months, the patient could walk with a cane, and after more than two years of follow-up, she continued walking without requiring additional aids, with no pain, and maintained good foot function. The spacer not only contributed to structural stability but also allowed for a certain range of residual motion in the forefoot, resulting in a rewarding and satisfactory functional outcome, avoiding complications such as recurrent infections.
In the studies conducted by Kavarthapu V et al. (29) and Niazi NS et al. (30), the use of bone cement as an adjunctive treatment for diabetic foot ulcers with osteomyelitis was evaluated. In both scenarios, a high success rate in wound healing was recorded, indicating that this method could be established as a standard of care for this type of wound. Furthermore, there was a notable decrease in postoperative pain and a reduction in hospitalization time, leading to a significant improvement in the patients’ quality of life. However, the studies also showed the existence of certain complications, such as wound dehiscence, ulceration at the surgical site, and recurrence of critical ischemia. Although these complications were not common, they highlight the importance of careful patient selection and strict postoperative monitoring. Another common finding in both studies was the appearance of deformities in some patients, such as hallux valgus and hammer toes.
Qin CH et al. (31) compared the use of antibiotic-impregnated calcium sulfate and bone resection alone. The findings indicated that, while both tactics achieved similar healing rates (90 % in the calcium sulfate group and 78.6 % in the control group), the group treated with calcium sulfate did not experience a recurrence of the infection, whereas 36.4 % of the control group did. The healing time and amputation rate did not show significant differences between the groups.
Discussion
The provided literature review extensively evaluates the effectiveness of bone cement in the treatment of DFUs and associated infections. The studies consistently demonstrate positive results in terms of healing rates, reduced hospitalization, and decreased amputation rates.
Sun YW et al. (19) observed a significant reduction in wound healing time when combining bone cement with negative pressure therapy (NPT) vs NPT alone. This synergistic effect suggests that bone cement may improve the wound healing environment.
Huang HJ et al. (20) and Mendame Ehya RE et al. (21) corroborated these findings, noting not only accelerated healing but also a reduction in pain, fewer dressing changes, and a smaller wound surface. Additionally, these studies highlighted a lower complication rate associated with the use of bone cement.
Melamed EA et al. (23) reported healing rates of up to 91.3 % in patients with osteomyelitis and severe forefoot infection treated with bone cement, further supporting its effectiveness in treating complex infections.
The underlying mechanisms contributing to the beneficial effects of bone cement in the treatment of diabetic foot include its ability to locally deliver antibiotics, fighting infection and preventing recurrence; its role as a scaffold for new tissue growth, accelerating wound healing; and its ability to fill bone defects caused by osteomyelitis, promoting bone regeneration.
Mendame Ehya RE et al. (21) found significantly lower amputation rates in the bone cement group compared to controls, emphasizing the potential of this treatment to preserve limbs. Hong CC et al. (29) and Kavarthapu V et al. (29) similarly demonstrated the ability of bone cement to save limbs in cases of osteomyelitis and Charcot foot deformity.
Qin CH et al. (31) reported a lower recurrence of infection and subsequent amputation risk with the use of bone cement, highlighting its long-term benefits.
Bone cement offers several advantages over systemic antibiotics, including its ability to administer higher concentrations of antibiotics directly at the infection site, ensuring effective bacterial elimination; its reduced systemic side effects due to localized drug delivery; and its ease of application, requiring minimal postoperative care.
Bone cement with antibiotics is used as a temporary treatment and is removed before proceeding with skin grafting or definitive ulcer closure. This approach is carried out after infection control has been achieved and granulation tissue formation has been promoted. The duration of bone cement use depends on the ulcer’s condition but is typically maintained for 7 to 10 days, depending on the ulcer’s status before removal.
After removal, granulation tissue quality is assessed, and if conditions are optimal, skin grafting or the final surgical intervention to close the ulcer is performed. Therefore, bone cement does not remain in the body long-term, as its purpose is to act as a local antibacterial support and wound healing promoter while in place. However, in some cases, as seen in the study by Mendame Ehya RE et al. (21), after approximately 3 weeks, the cement began to degrade or reduce in size, leaving a thin coating on the ulcer surface and promoting healthy tissue formation. This suggests that removal may not be necessary in some cases, as the cement gradually degrades, but in others, it is manually removed during a secondary procedure. In cases where Çerament is used, as in the study by Niazi NS et al. (30), the cement releases high concentrations of antibiotic (gentamicin in this case) for approximately 28 days, effectively combating infection. Calcium sulfate dissolves first, releasing the antibiotic and leaving a porous hydroxyapatite structure. Hydroxyapatite acts as an osteoconductive scaffold, promoting the formation of new bone.
In cases where bone cement with polymethyl methacrylate (PMMA) is used, as in the study by Hong CC et al. (28), a non-biodegradable cement widely used in orthopedic applications is employed for its ability to provide durable structural support and be molded to fit bone defects. The cement is shaped into a block to fill the cavity created after the resection of avascular and devitalized bone. Its main function is twofold: local release of high concentrations of antibiotics to treat osteomyelitis and providing structural stability to allow soft tissue healing and foot functionality. This approach enabled effective treatment of the infection and stabilization of the foot, without the need to remove the cement in the long-term follow-up—in this case, 2 years and 8 months, with the spacer remaining in situ, showing evidence of infection resolution and good bone fusion between the calcaneus and tibia. No significant bone loss or cement-related complications were observed. Although PMMA is still used in selected cases, it is being progressively replaced by biodegradable materials that offer fewer complications and greater efficacy in managing diabetic foot.
Conclusions
Bone cement with antibiotics could be an effective treatment for managing diabetic foot in cases of osteomyelitis. Some studies suggest that bone cement would be effective in redistributing pressure, providing stability, especially in cases of Charcot foot. Based on the reviewed literature, bone cement would promote ulcer healing and prevent serious complications like amputation. Furthermore, the use of bone cement reduces the bacterial load as the antibiotic is deposited locally in the affected area, leading to a reduction in infection symptoms and avoiding possible systemic toxicity. Finally, it is expected that the effects of bone cement will be enhanced when combined with other therapies indicated for the management of diabetic foot, such as negative pressure therapy, increasing the success rate.
Authors’ contributions
Study conception and design: AFO, MLM, YGA, JLLM.
Data collection: AFO, MLM.
Data analysis and interpretation: AFO, MLM, MGM, RJMB, JLLM.
Creation, drafting, and drafting of the initial manuscript: AFO, MLM, MGM, RJMB, YGA, JLLM.
Final review: AFO, MLM, MGM, RJMB, YGA, JLLM.
Conflicts of interest
None declared.
Funding
None declared.
References
- Conget I. Diagnóstico, clasificación y patogenia de la diabetes mellitus. Rev Esp Cardiol. 2002;55(5):528-38. DOI: 10.1016/S0300-8932(02)76646-3.
- Kaul K, Tarr JM, Ahmad SI, Kohner EM, Chibber R. Introduction to diabetes mellitus. In: Ahmad SI, editor. Diabetes: An old disease, a new insight. Vol. 771. Springer; 2012. p. 1-11. DOI: 10.1007/978-1-4614-5441-0_1.
- International Diabetes Federation. IDF Diabetes Atlas. 10th ed. Brussels, Belgium: Author; 2021.
- Singh N, Armstrong DG, Lipsky BA. Preventing foot ulcers in patients with diabetes. JAMA. 2005;293(2):217-28. DOI: 10.1001/jama.293.2.217.
- Van Netten JJ, Price PE, Lavery LA, Monteiro-Soares M, Rasmussen A, Jubiz Y, et al. Prevention of foot ulcers in the at-risk patient with diabetes: A systematic review. Diabetes Metab Res Rev. 2016;32(S1):84-98. DOI: 10.1002/dmrr.2701.
- Lipsky BA, Berendt AR, Cornia PB, Pile JC, Peters EJ, Armstrong DG, et al. Infectious Diseases Society of America Clinical Practice Guideline for the Diagnosis and Treatment of Diabetic Foot Infections. Clin Infect Dis. 2012;54(12): e132-e173. DOI: 10.1093/cid/cis346.
- Senneville É, Albalawi Z, van Asten SA, Abbas ZG, Allison G, Aragón-Sánchez J, et al. IWGDF/IDSA Guidelines on the Diagnosis and Treatment of Diabetes-related Foot Infections (IWGDF/IDSA 2023). Clin Infect Dis. 2023. DOI: 10.1093/cid/ciad527.
- Lázaro-Martínez JL, Aragón-Sánchez J, García-Morales E. Antibiotics versus conservative surgery for treating diabetic foot osteomyelitis: A RCT. Diabetes Care. 2014; 37:789-95. DOI: 10.2337/dc13-1526.
- Game FL. Osteomyelitis in the diabetic foot: Diagnosis and management. Med Clin North Am. 2013; 97:947-56. DOI: 10.1016/j.mcna.2013.03.010.
- Alvaro-Afonso FJ, Lázaro-Martínez JL, García-Morales E, García-Álvarez Y, Sanz-Corbalán I, Molines-Barroso RJ. Cortical disruption is the most reliable and accurate plain radiographic sign in the diagnosis of diabetic foot osteomyelitis. Diabet Med. 2019;36:258-9. DOI: 10.1111/dme.13824.
- Butalia S, Palda VA, Sargeant RJ, Detsky AS, Mourad O. Does this patient with diabetes have osteomyelitis of the lower extremity? JAMA. 2008; 299:806.
- Lipsky BA, Peters EJ, Senneville E, Berendt AR, Embil JM, Lavery LA, et al. Expert opinion on the management of infections in the diabetic foot. Diabetes Metab Res Rev. 2012;28(Suppl 1):163-78. DOI: 10.1002/dmrr.2248.
- Peters EJ, Lipsky BA, Aragón-Sánchez J, Boyko EJ, Diggle M, Embil JM, et al. Interventions in the management of infection in the foot in diabetes: A systematic review. Diabetes Metab Res Rev. 2016;32(Suppl 1):145-53. DOI: 10.1002/dmrr.2706.
- Lipsky BA. Treating diabetic foot osteomyelitis primarily with surgery or antibiotics: Have we answered the question? Diabetes Care. 2014;37(3):593-5. DOI: 10.2337/dc13-2510.
- Arora M, Chan EK, Gupta S, Diwan AD. Polymethylmethacrylate bone cements and additives: A review of the literature. World J Orthop. 2013;4(2):67-74. DOI: 10.5312/wjo.v4.i2.67.
- Martel JRC, Núñez García JA. Capítulo 23: El cemento en las prótesis articulares, características y propiedades. En: Manual del residente de COT de la SECOT. 2014. p. 104-6.
- Ramanujam CL, Zgonis T. Antibiotic-loaded cement beads for Charcot ankle osteomyelitis. Foot Ankle Spec. 2010;3(5):274-7. DOI: 10.1177/1938640010376563.
- Rao N, Ziran BH, Lipsky BA. Treating osteomyelitis: Antibiotics and surgery. Plast Reconstr Surg. 2011;127(Suppl 1):177S-87S. DOI: 10.1097/PRS.0b013e3182001f0f.
- Sun YW, Li L, Zhang ZH. Antibiotic-loaded bone cement combined with vacuum-assisted closure facilitating wound healing in Wagner 3-4 diabetic foot ulcers. Int J Lower Extremity Wounds. 2022. DOI: 10.1177/15347346221109045.
- Huang HJ, Niu XH, Yang GL, Wang LY, Shi FC, Xu SJ, et al. Clinical effects of application of antibiotic bone cement in wounds of diabetic foot ulcers. Zhonghua Shao Shang Za Zhi. 2019;35(6):464-6.
- Mendame Ehya RE, Zhang H, Qi B, Yu A. Application and clinical effectiveness of antibiotic-loaded bone cement to promote soft tissue granulation in the treatment of neuropathic diabetic foot ulcers complicated by osteomyelitis: A randomized controlled trial. J Diabetes Res. 2021; 2021:9911072. DOI: 10.1155/2021/9911072.
- Yang C, Wang D. Antibiotic bone cement accelerates diabetic foot wound healing: Elucidating the role of ROCK1 protein expression. Int Wound J. 2024;21(4): e14590. DOI: 10.1111/iwj.14590.
- Melamed EA, Peled E. Antibiotic impregnated cement spacer for salvage of diabetic osteomyelitis. Foot Ankle Int. 2012;33(3):213-9. DOI: 10.3113/FAI.2012.0213.
- Dalla Paola L, Carone A, Morisi C, Cardillo S, Pattavina M. Conservative surgical treatment of infected ulceration of the first metatarsophalangeal joint with osteomyelitis in diabetic patients. J Foot Ankle Surg. 2015;54(4):536-40. DOI: 10.1053/j.jfas.2014.08.004.
- Cao T, Ji P, Zhang Z, Xiao D, Wang KJ, Li N, et al. A prospective randomized controlled study of antibiotic bone cement in the treatment of diabetic foot ulcer. Zhonghua Shao Shang Yu Chuang Mian Xiu Fu Za Zhi. 2023;39(4):311-8.
- Dai J, Zhou Y, Mei S, Chen H. Application of antibiotic bone cement in the treatment of infected diabetic foot ulcers in type 2 diabetes. BMC Musculoskelet Disord. 2023;24(1):135. DOI: 10.1186/s12891-023-06244-w.
- Jiang X, Li N, Yuan Y, Yang C, Chen Y, Ma Y, et al. Limb salvage and prevention of ulcer recurrence in chronic refractory diabetic foot osteomyelitis. Diabetes Metab Syndr Obes. 2020; 13:2289-96. DOI: 10.2147/DMSO.S254586.
- Hong CC, Jin Tan K, Lahiri A, Nather A. Use of a definitive cement spacer for simultaneous bony and soft tissue reconstruction of mid- and hindfoot diabetic neuroarthropathy: A case report. J Foot Ankle Surg. 2015;54(1):120-5. DOI: 10.1053/j.jfas.2014.10.009.
- Kavarthapu V, Giddie J, Kommalapati V, Casey J, Bates M, Vas P. Evaluation of adjuvant antibiotic-loaded injectable bio-composite material in diabetic foot osteomyelitis and Charcot foot reconstruction. J Clin Med. 2023;12(9):3239. DOI: 10.3390/jcm12093239.
- Niazi NS, Drampalos E, Morrissey N, Jahangir N, Wee A, Pillai A. Adjuvant antibiotic-loaded bio-composite in the management of diabetic foot osteomyelitis: A multicentre study. Foot (Edinb). 2019; 39:22-7. DOI: 10.1016/j.foot.2019.01.005.
- Qin CH, Zhou CH, Song HJ, Cheng GY, Zhang HA, Fang J, Tao R. Infected bone resection plus adjuvant antibiotic-impregnated calcium sulfate versus infected bone resection alone in the treatment of diabetic forefoot osteomyelitis. BMC Musculoskelet Disord. 2019;20(1):246. DOI: 10.1186/s12891-019-2635-8.