DOI: http://dx.doi.org/10.20986/revesppod.2024.1707/2024
CLINICAL NOTE
Treatment of recalcitrant plantar wart using Falknor’s multipuncture technique in combination with oral zinc: a case report
Tratamiento de verruga plantar recalcitrante mediante la técnica de multipunción de Falknor en combinación con zinc oral: a propósito de un caso clínico
Lois García-Clavería1
Carla Lanuza-Cerzócimo2
Javier Alfaro-Santafé3
Antonio Gómez-Bernal3
1Departamento de Formación e Investigación. Clínica Podoactiva Vitoria. Vitoria, España
2Departamento de Formación e Investigación. Clínica Podoactiva Huesca, Huesca, España
3Departamento de Formación e Investigación. Central de Podoactiva Walqa. Huesca, España
Abstract
Plantar warts are skin lesions caused by the human papillomavirus (HPV), which infects epidermal cells and can remain latent before becoming active. Although generally asymptomatic, these lesions can cause pain, be unsightly, or become contagious. HPV evades detection by the immune system by not releasing viral proteins that would alert it. Treatments for plantar warts include chemical, physical, pharmacological, and surgical methods, with studies suggesting that early induction of immunity can be beneficial. In the case of a 24-year-old patient with warts on the metatarsal areas and the pads of the toes of both feet, a treatment with nitric acid was attempted without success. Subsequently, the multipuncture technique was chosen in the right foot. The intervention included an ultrasound-guided anesthetic block of the posterior tibial and deep peroneal nerves, followed by debridement of hyperkeratosis and the application of the multipuncture technique, with multiple punctures covering the entire surface of the warts. The patient was treated with Inmunoferon® (Cantabria Labs, Spain) and was advised relative rest, avoiding non-steroidal anti-inflammatory drugs (NSAIDs). Subsequent reviews showed progressive improvement: at 48 hours, the lesions had fine scabs and were painless; at 15 days, the lesions appeared drier also in the contralateral foot; at one month, continuous improvement was evident. The multipuncture technique associated with Inmunoferon® proved to be effective, less painful, and required minimal care.
Keywords: Plantar wart, papilloma, HPV, treatment, multipuncture, Falknor, therapy, foot
Resumen
La verruga plantar es una lesión cutánea causada por el virus del papiloma humano (VPH), que infecta las células epidérmicas y puede permanecer latente antes de activarse. Aunque generalmente asintomáticas, estas lesiones pueden causar dolor, ser antiestéticas o contagiarse. El VPH evade la detección del sistema inmunitario al no liberar proteínas virales que lo alerten. Los tratamientos para las verrugas plantares incluyen métodos químicos, físicos, farmacológicos y quirúrgicos, con estudios que sugieren que la inducción temprana de la inmunidad puede ser beneficiosa. En el caso de un paciente de 24 años con verrugas en las zonas metatarsal y el pulpejo de los dedos de ambos pies, se intentó un tratamiento con ácido nítrico, sin éxito. Posteriormente, se optó por la técnica de multipunción en el pie derecho. La intervención incluyó un bloqueo anestésico ecoguiado de los nervios tibial posterior y peroneo profundo, seguido de un deslaminado de la hiperqueratosis y la aplicación de la técnica de multipunción, con múltiples pinchazos para cubrir toda la superficie de las verrugas. El paciente fue tratado con Inmunoferón® (Cantabria Labs, España) y se le recomendó reposo relativo, evitando antinflamatorios no esteroideos (AINE). Las revisiones posteriores mostraron una mejora progresiva: a las 48 horas, las lesiones tenían costras finas y eran indoloras; a los 15 días, las lesiones se vieron más secas también en el pie contralateral; al mes, se evidenció una mejora continua. La técnica de multipunción asociada al Inmunoferón® demostró ser efectiva, menos dolorosa y con mínimos cuidados requeridos.
Palabras clave: Verruga plantar, papiloma, VPH, tratamiento, multipunción, Falknor, terapia, pie
Corresponding author: Antonio Gómez-Bernal
antoniogomez@podoactiva.com
Received: 18-09-2024
Accepted: 20-11-2024
Introduction
Plantar warts are skin lesions that affect the basal layer of the epidermis, caused by the human papillomavirus (HPV), typically types 1, 2, 4, 19, 27, 41, and 57(1,2,3). HPV infects keratinocytes and can remain latent for 1 up to 8 months. As epidermal cells differentiate and migrate to the surface, the virus activates and replicates2. While often asymptomatic, plantar warts can cause pain due to their location on weight-bearing areas (such as the heel or metatarsal heads), as well as being unsightly, spreading to other parts of the body, or transmitting to other individuals(1)..
In most viral infections, viral proteins within the cell stimulate the production of cytotoxic T cells that seek out and destroy infected cells. However, HPV prevents cell lysis as the infection spreads, meaning the release of viral proteins and their presentation to the immune system are minimal or nonexistent(2)..
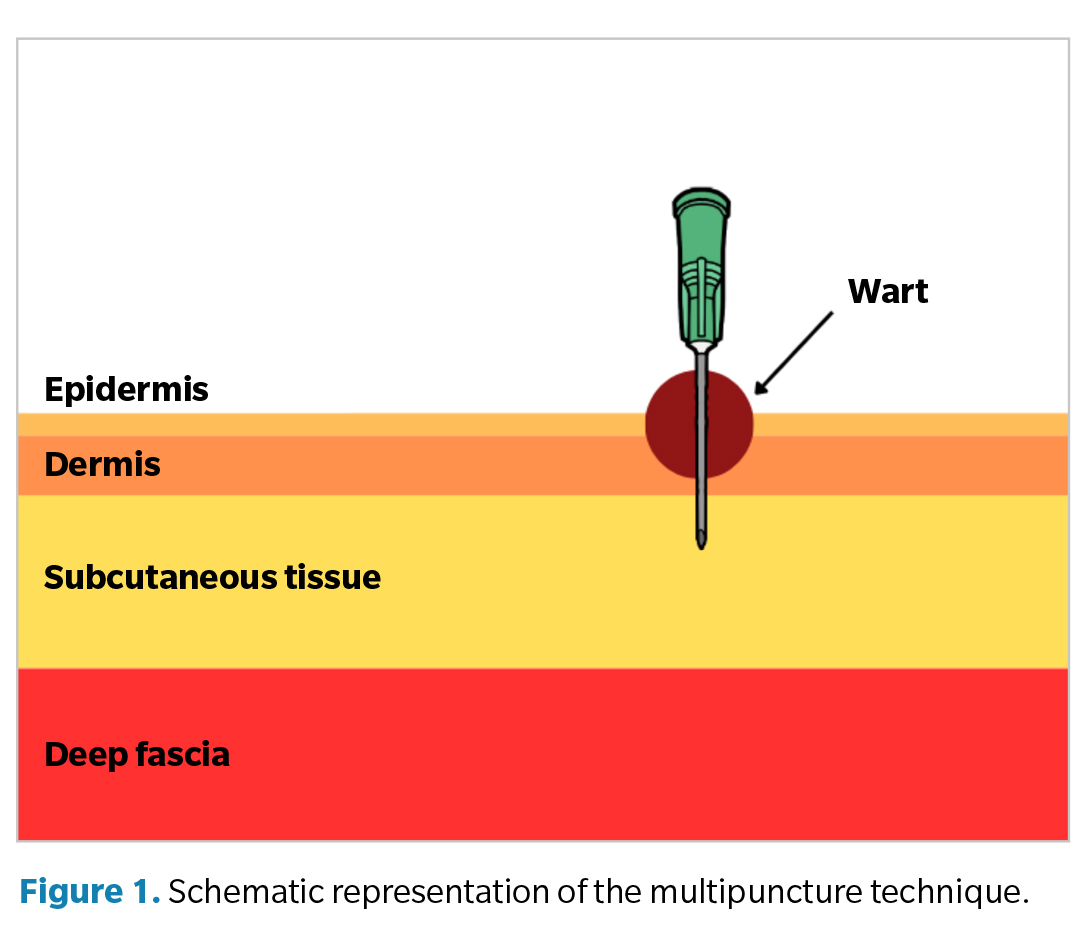
There are multiple therapeutic options: chemical treatments (nitric acid, salicylic acid, cantharidin...), physical treatments (liquid nitrogen, laser...), pharmacological approaches (bleomycin), and surgical options(4). Falknor’s multipuncture technique, or the “needling method,” is an alternative to conventional surgical treatment first described by Gordon W. Falknor in 1969. This technique involves puncturing the plantar wart (Figure 1), inducing a controlled inflammatory process that allows the immune system to identify viral proteins and generate antibodies to eliminate the virus-infected cells(2,5,6,7,8,9).
Of note, the lack of cellular response in most treatments could explain why many are not uniformly successful and challenging in certain cases. Most treatments focus on tissue destruction, but tissue damage alone may not suffice to generate the cytokines necessary to eradicate the virus(2).. Frazer concluded in his study that inducing early immunity could be useful in treating HPV infections, potentially achieved by presenting viral antigens to the immune system5. Chapman et al. hypothesized that it should be possible to achieve a “systemic body response” in patients with multiple warts by treating just one wart(6). They concluded that treatment success is more likely in patients under 14 years old(6).
A review of the existing literature reveals a wide range of treatments. In 2022, Peiyao Zhu et al. developed a guide for the diagnosis and treatment of cutaneous warts, including various options depending on the type of wart, location, number of lesions, etc. (4). For common warts, treatments such as bleomycin injections, cryotherapy, and thermotherapy are included(4).. Bagwell’s study evaluates the option of oral acyclovir treatment for resolving these lesions(10). Interestingly, the article by García-Oreja et al. notes that more invasive treatments, such as immunotherapy or intralesional bleomycin, have higher cure rates than conventional topical treatments(11). Additionally, it is worth noting that zinc deficiency is associated with persistent and recurrent plantar warts(12,13).due to the mineral’s role in cellular metabolism, playing a crucial role in human T-cell functions(13).
Cure is considered achieved when the lesions disappear within 4 weeks and do not recur for at least 6 months(7)..
Due to the good results obtained in treating our patient by combining the multipuncture technique with immunoferon, we found it interesting to present a case report describing the procedure used, as it may be of interest for podiatry community.
Case report
A 24-year-old man presented to the clinic with no relevant past medical history. He exhibited hyperkeratotic lesions on the metatarsal area and the fingertips, most prominently on the first and second metatarsal heads of the right foot and the fourth metatarsal head of the left foot (Figure 2).

The lesions were bothersome but not painful in daily activities, although they were painful to the pinch test during consultation. Upon debridement of the hyperkeratosis with a scalpel, papillae were visible, and mosaic plantar warts were diagnosed. The patient had 17 plantar lesions in total (11 on the right foot and 6 on the left), distributed across the forefoot (metatarsal area and fingertips).
Prior treatment with 60 % nitric acid was attempted over 11 weekly sessions without success. The patient was subsequently offered treatment using the multipuncture technique that he accepted. The materials used for the technique are detailed in Figure 3.
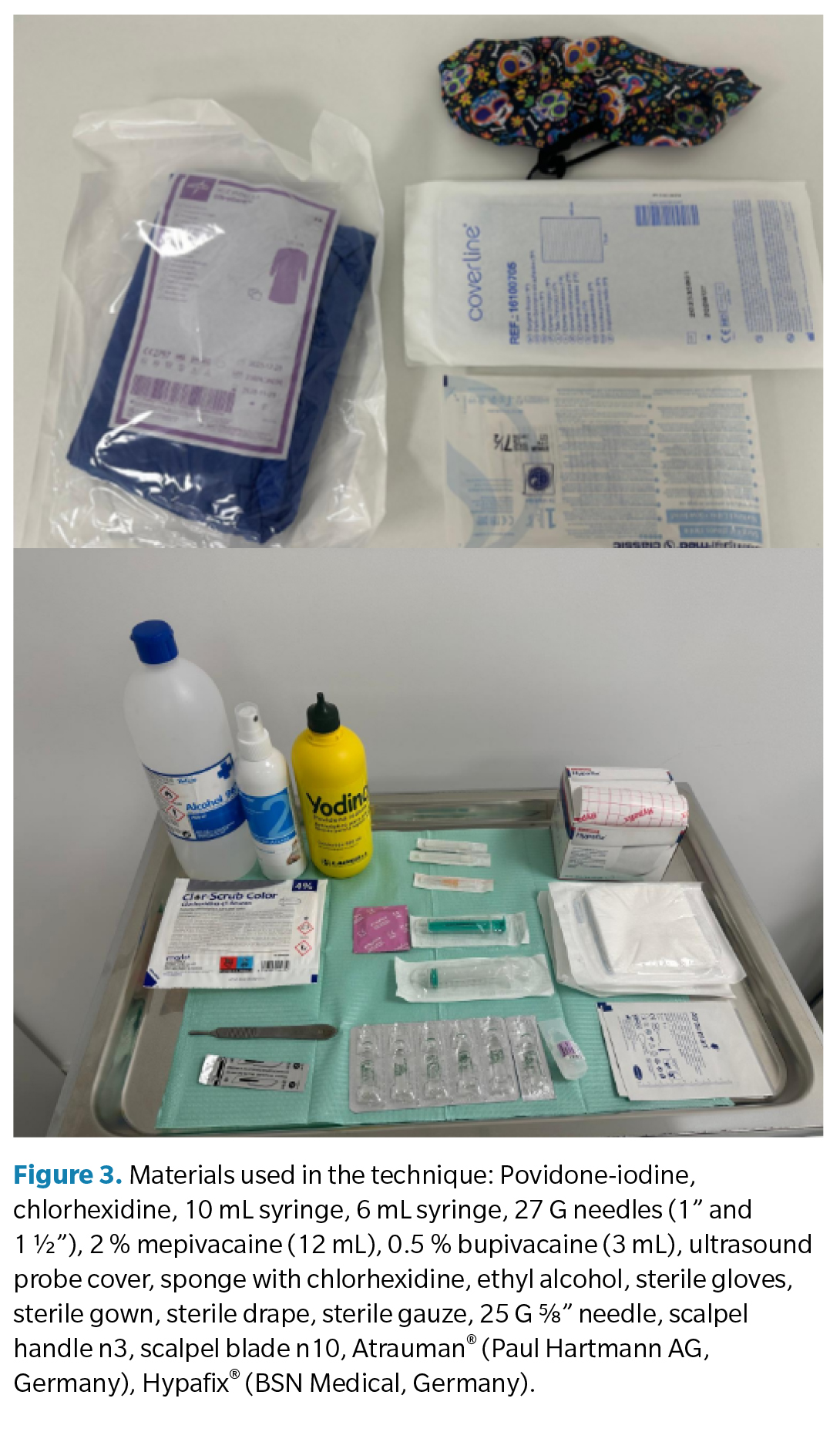
First, anesthetic blockage was performed. Considering the lesion sites, an ultrasound-guided posterior tibial nerve and deep peroneal nerve block were performed using 8 mL of mepivacaine + 2 mL of bupivacaine and 4 mL of mepivacaine + 1 mL of bupivacaine, respectively. This combination was used to pair the fast-acting effect of mepivacaine for the procedure with the longer-lasting analgesic effect of bupivacaine for patient comfort.
Asepsis was administered using povidone-iodine and sterile gauze, followed by cleansing the puncture sites with chlorhexidine. To accurately identify the structures and puncture sites, an ultrasound-guided technique was employed, using a protective cover to maintain asepsis throughout the procedure.
While waiting for the anesthetic to take effect, the foot was thoroughly washed with a chlorhexidine sponge and ethanol. The clinician dressed in sterile attire —gown and gloves— and a sterile field was prepared.
Debridement of the hyperkeratosis was performed with a scalpel before the multipuncture technique. Then, using a 25 G ? needle, punctures were made across the surface of the wart (Figure 4). By targeting the papilloma through the immune system, treatment was applied only to the right foot, as a positive response to the therapy could lead to spontaneous resolution of the contralateral foot. This foot was chosen because it was the most affected one, with a higher likelihood of addressing the primary lesion.

There is no consensus in the literature regarding the number of punctures required. Some articles recommend puncturing until the entire lesion is covered2 or until no epidermal resistance is felt and the lesion has a soft, fleshy consistency(1). Both criteria were applied: punctures were performed until the entire lesion area was covered, forming a red wound with a fleshy, soft consistency (Figure 5). After addressing all lesions, the wound was covered with Atrauman®, sterile gauze, and Hypafix®.

Relative rest was recommended, and paracetamol was suggested for pain management. Importantly, NSAIDs were avoided, as only analgesics were used to promote a controlled inflammatory response that helps the immune system recognize the papilloma(2).
The treatment was supplemented with Immunoferon® (60 capsules, 2/day until completion) as an adjuvant therapy. This dietary supplement contains AM3® (phosphorylated alpha-glucomannan and soy protein), zinc, echinacea, and other ingredients aimed at immune stimulation.
Follow-up visits were scheduled at 48 hours, 15 days, 1 month, and 6 months to monitor progress and outcomes.
First follow-up (48 hours post-intervention)
Wounds are observed with a thin crust and the marks from the punctures (Figure 6). In this case, an attempt was made to superficially debride them, but it is not recommended (due to the skin being very thin and some areas causing slight bleeding). The patient reported no pain in the previous days and did not require any analgesics.

Second follow-up (15 days post-intervention)
A change in the appearance of the lesions is noted, with the wounds appearing much drier vs 48 hours post-treatment. At this stage, the lesions can be debrided without any issues. Hyperkeratosis was removed with a scalpel (including from the untreated contralateral foot, which showed apparent improvement, as seen in Figures 7 and 8).


Third follow-up (1 month post-intervention)
The improvement in appearance is increasingly evident, particularly in the contralateral foot. Hyperkeratosis was debrided from the untreated foot (Figure 9).

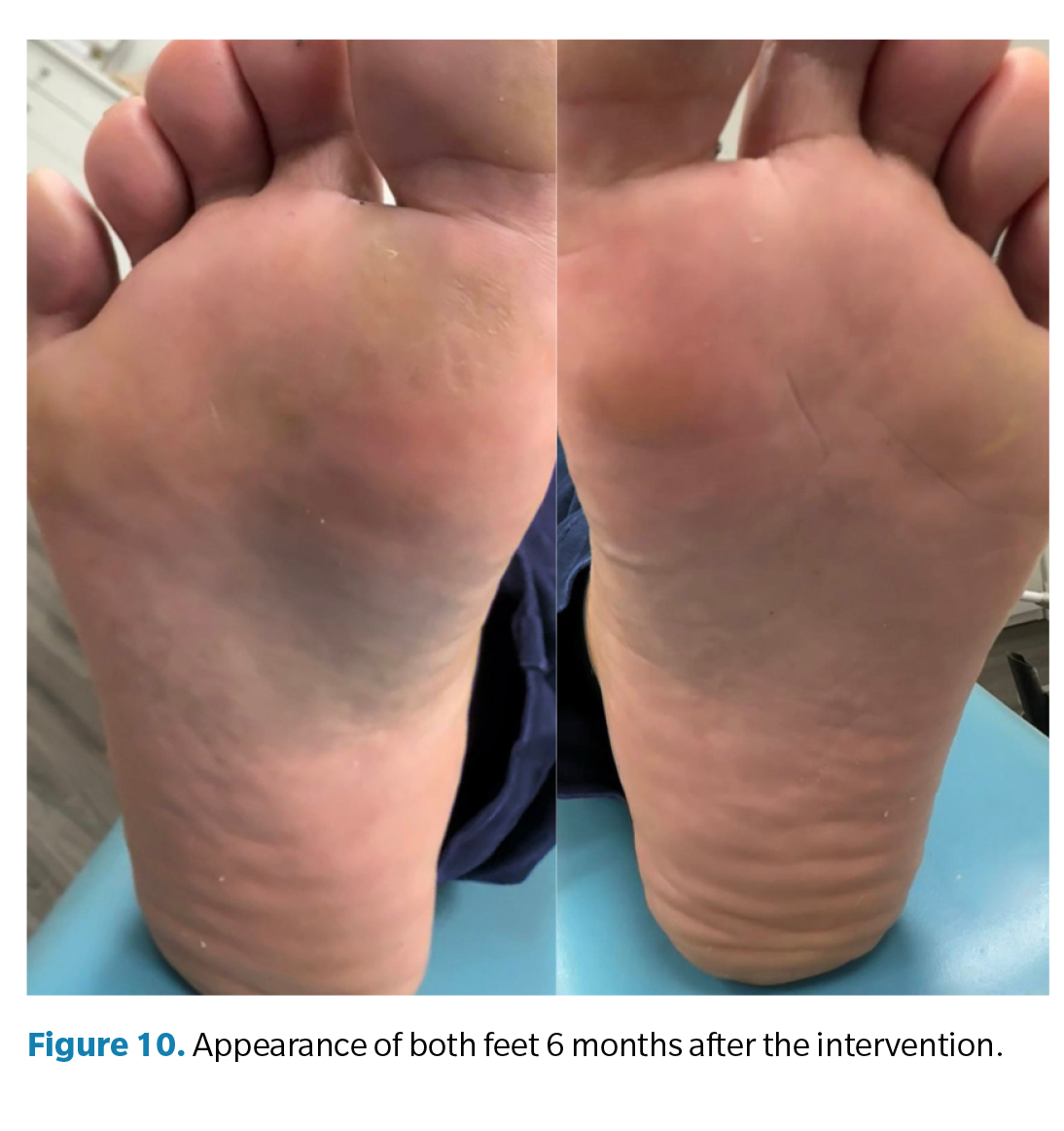
Fourth follow-up (6 months post-intervention)
Complete healing of the infection in both feet is considered to have occurred, as shown in Figure 10. No recurrence is observed, with only minor areas of hyperkeratosis present due to metatarsal overload.
Discussion
The multipuncture technique is a safe, effective, and quick alternative for the management of plantar warts(1,2,5,6,7,8).. Its use is particularly interesting in young patients(5).. Similarly, there is an important relationship between zinc deficiency and persistent, recurrent, and progressive warts(12;13,14). However, no studies have ever been found that combine this technique with oral zinc supplementation.
Using multipuncture in combination with oral zinc appears to be an effective and safe option for managing recalcitrant plantar warts. Among its advantages, the technique is convenient for patients, as it involves a minimally painful intervention requiring only a single session. Additionally, immune system stimulation can lead to a total cure, eliminating lesions in other anatomical regions, as observed in this case and as reflected in the literature.
However, the need to administer anesthesia beforehand, through sublesional or ankle nerve block, can make this procedure challenging in pediatric patients and requires a certain level of skill from the specialist. This treatment could be applied to any type of patient, although it might not be effective in immunocompromised individuals, for whom other therapeutic options should be considered.
Frequent follow-ups are not deemed necessary. In this case, multiple reviews were conducted to monitor progressive evolution and document it for the case study. Based on this case and the literature, an appropriate protocol would involve an initial follow-up at 48 hours to assess wound status and important parameters: presence of inflammation, absence of infection, and wound condition. A second follow-up is recommended at 1 month, as this is when good progress can be observed, as shown in this case. Subsequently, a review at 3 months is advisable, as this is the estimated time for complete wound remission2,5,6, and another at 6 months to ensure no recurrence(8).
In conclusion, the multipuncture technique plus oral zinc supplementation could be a very promising therapeutic option for cases involving multiple recalcitrant plantar warts. For a large number of warts, an ankle-level anesthetic block is recommended, but a full block is not necessary. In cases with lesions on both feet, it is recommended to perform the intervention on only one foot, as the contralateral foot may heal without requiring the multipuncture technique, due to immune system stimulation. It is considered worthwhile to conduct a randomized clinical trial to evaluate the efficacy of this technique in a larger sample.
Informed consent
The patient has given consent for the use of images and clinical data in the preparation of this article.
Conflicts of interest
None declared.
Funding
None declared.
Authors’ contributions
Study conception and design: LGC, AGB
Data collection: LGC, CLC
Analysis and interpretation: LGC
Drafting and preparation of the initial manuscript: LGC
Final review: LGC, CLC, JAS, AGB
References
- Kumari P, Yadav D, Vijay A, Jain SK, Kumar M, Kumar R, et al. Falknor’s needling method as a potential immunotherapy in palmo-plantar warts. Indian J Dermatol Venereol Leprol. 2019;85(1):129. DOI: 10.4103/ijdvl.IJDVL_809_17.
- Longhurst B, Bristow I. The treatment of verrucae pedis using Falknor’s needling method: a review of 46 cases. J Clin Med. 2013;2(2):13-21. DOI: 10.3390/jcm2020013.
- García-Oreja S, Álvaro-Afonso FJ, Sevillano-Fernández D, García-Morales EA, López-Moral M, Lázaro-Martínez JL. Does HPV biotype influence the characteristics and evolution of plantar warts? J Evid Based Med. 2024;17(1):10-2. DOI: 10.1111/jebm.12584.
- Zhu P, Qi RQ, Yang Y, Huo W, et al. Clinical guideline for the diagnosis and treatment of cutaneous warts (2022). J Evid Based Med. 2022;15(3):284-301.
- Frazer IH. Interaction of human papillomaviruses with the host immune system: a well evolved relationship. Virology. 2009;384(2):410-4. DOI: 10.1016/j.virol.2008.10.004.
- Chapman C, Visaya G. Treatment of multiple verrucae by triggering cell-mediated immunity: a clinical trial. Br J Podiatry. 1998;1:89-90.
- Falknor GW. Needling-a new technique in verruca therapy. J Am Podiatry Assoc. 1969;59(2):51-2. DOI: 10.7547/87507315-59-2-51.
- Baveja S, Grover C, Reddy BS. Falknor’s needling technique for the treatment of warts: minimum investment, maximum benefit. Med J Armed Forces India. 2022;78(4):403-7.
- Hashmi F, Torgerson D, Fairhurst C, Cockayne S, Bell K, Cullen M, et al. EVerT2-needling versus non-surgical debridement for the treatment of verrucae: study protocol for a single-centre randomised controlled trial. BMJ Open. 2015;5(11):e009406. DOI: 10.1136/bmjopen-2015-009406.
- Bagwell A, Loy A, McFarland MS, Tessmer-Neubauer A. Oral acyclovir in the treatment of verruca. J Drugs Dermatol. 2016;15(2):237-8.
- García-Oreja S, Álvaro-Afonso FJ, García-Álvarez Y, García-Morales E, Sanz-Corbalán I, Lázaro Martínez JL. Topical treatment for plantar warts: A systematic review. Dermatol Ther. 2021;34(1):e14621. DOI: 10.1111/dth.14621.
- Raza N, Khan DA. Zinc deficiency in patients with persistent viral warts. J Coll Physicians Surg Pak. 2010;20(2):83-6.
- Ghanem AH, Esawy AM, Khalifa NA, Kamal HM. Evaluation of serum interleukin 17 and zinc levels in recalcitrant viral warts. J Cosmet Dermatol. 2020;19(4):954-9. DOI: 10.1111/jocd.13106.
- Cassano N, Ferrari A, Fai D, Pettinato M, Pellè S, Del Brocco L, et al. Oral supplementation with a nutraceutical containing Echinacea, methionine, and antioxidant/immunostimulating compounds in patients with cutaneous viral warts. G Ital Dermatol Venereol. 2011;146(3):191-5.