DOI: 10.20986/revesppod.2022.1647/2022
ORIGINAL
Effect of custom rigid insoles in compressive plantar heel pain:
a prospective case series
Efecto de las ortesis plantares rígidas a medida en la fasciopatía plantar compresiva:
serie de casos prospectiva
Javier Pascual Huerta, Lucia Trincado Villa y Leticia Palacio Fernández
Clínica del Pie Elcano. Barakaldo. Bizkaia, España
Abstract
Objetives: There is no strong evidence for the use of insoles in the treatment of plantar heel pain associated to fasciopathy. The present study used a specific orthosis type with custom elements for offloading the heel to assess its effect in pain and plantar fascia thickness in patients with plantar fasciopathy.
Patients and methods: A prospective study of case series type was performed in patients with unilateral plantar fasciitis with the only conservative treatment of rigid custom plantar insoles made in polypropylene with a partial weightbearing cast and specific offloading elements of the medial process of the posterior tuberosity of the calcaneus and increased heel cup. Pain and plantar fascia thickness was measured at four different localizations before and after one, three and six months of treatment.
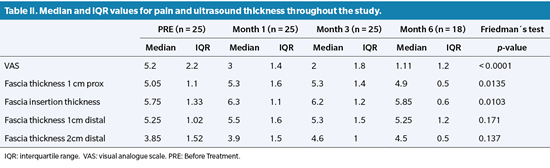
Results: Of the 42 patients initially recruited only a final number of 18 cases completed the study at six months. It was observed a decreased in pain intensity at one, three and six months that was statistically significant in all comparisons. There were significant differences in plantar fascia thickness between pretreatment measurements and measurements at the sixth month with a small decrease in thickness.
Conclusions: Although not a randomized clinical trial, the present study showed that orthoses reduced significantly pain at one, three and six months suggesting that this type of specific prescription could be effective for the symptomatic improvement of these patients.
Keywords: Plantar fasciitis, heel spur syndrome, treatment, foot orthoses, insoles, visual analog scale, ultrasonography.
Resumen
Objetivos: No existen todavía evidencias sólidas para el uso de ortesis plantares en el tratamiento de pacientes con dolor de talón asociado a fasciopatía plantar. El presente trabajo valora el efecto de un tipo de ortesis plantar a medida con elementos específicos de descarga en el dolor y el grosor de la fascia plantar.
Pacientes y métodos: Se realizó estudio prospectivo de serie de casos en pacientes con fasciopatía plantar unilateral con tratamiento conservador por medio de ortesis plantares a medida rígidas en polipropileno con molde en semicarga y con descarga específica del proceso medial de la tuberosidad posterior del calcáneo y aumento de la cazoleta posterior. Se midió el dolor mediante escala analógica visual y grosor de la fascia plantar en 4 localizaciones antes del tratamiento y durante el tratamiento al mes, tres y seis meses.
Resultados: De los 42 pacientes inicialmente reclutados hubo pérdidas hasta llegar a 18 pacientes a los 6 meses. Se observó una disminución del dolor al mes, a los 3 meses y a los 6 meses, que fue estadísticamente significativa en todas las comparaciones. Se observaron diferencias estadísticamente significativas en el grosor de la fascia plantar entre la valoración inicial y al sexto mes con disminución del grosor.
Conclusiones: A pesar de no tratarse de un ensayo clínico aleatorizado, los resultados mostraron una reducción estadísticamente significativa del dolor al primer, tercer y sexto mes, sugiriendo que las plantillas con este tipo de prescripción específica podrían ser efectivas en la mejoría sintomática de estos pacientes.
Palabras clave: Fascitis plantar, espolón calcáneo, tratamiento, ortesis, plantillas, escala analógica visual, ecografía.
Received: 24-08-2022
Accepted: 31-10-2022
Correspondence: Javier Pascual Huerta
javier.pascual@hotmail.com
INTRODUCTION
Heel pain associated with plantar fasciopathy is one of the most common disorders in the adult population with an estimated prevalence of around 10 % of the population1,2. This condition mainly affects the active population, especially common in runners where it can have a prevalence of 22 %, and the pain associated with this condition significantly affects the function and quality of life of these patients1-4. Treatment is almost always conservative with rest, NSAIDs, physical therapy, plantar orthoses, shockwave therapy and infiltrations among others5,6. Although research into this pathology has grown in recent years, there is still no clear rationale for the use of plantar foot orthoses as a line of treatment for pain associated with plantar fasciopathy. The quality of the published evidence is low-moderate in most cases and although in the medium term the use of insoles seems to be effective in reducing pain, in the short and long term their role is much more controversial7-9. Similarly, the use of custom-made insoles in these patients has not shown superior effects in pain reduction to the use of standard or prefabricated insoles10,11.
However, the concept of custom-made insoles is excessively heterogeneous and vague. There are many variables in this idea that refer to the materials used (rigid, soft, etc...), manufacturing methods (cast taking, fitting technique, work on the positive, etc...), use of specific elements in the prescription of the insole for cases of plantar fasciopathy (cupping, rebound, subcalcaneal fenestratiions, etc...) and observations of the clinician who carries out the examination, among others. The multiple combinations that exist between all these factors make the options for custom-made insoles excessively heterogeneous and make this process a difficult concept to standardize in order to carry out research. In fact, there are no single studies that had used the same type of insoles considered “custom-made” and this may be one of the reasons why the results of the studies using custom-made insoles in patients with heel pain show ambiguous results.
The aim of this paper is to present the results of a case series of patients treated with custom-made polypropylene plantar foot orthoses with specific offloading elements for the treatment of compressive plantar fasciopathy12,13 and to assess their clinical effectiveness in reducing pain as well as their effect on the thickness of the plantar fascia measured sonographically.
PATIENTS AND METHODS
Study Design
A prospective longitudinal case series study was conducted in patients with heel pain associated with plantar fasciopathy. This article was written according to the recommendations of the STROBE guidelines for writing observational studies14.
Study population
The study sample consists of patients with heel pain who met the following inclusion criteria: age over 18 years old, clinical and ultrasound diagnosis of unilateral plantar fasciopathy (plantar fascia thickness greater than 4 mm with hypoechoic image and loss of fibrillar pattern15) of compressive type (located in the medial process of the posterior calcaneal tuberosity and not in the distal course of the plantar fascia) and who were seeking to undergo treatment for heel pain by conservative means with custom-made plantar orthoses without infiltrations, shockwave therapy or other invasive therapies. Cases with bilateral heel pain, cases with connective tissue diseases under treatment with corticosteroids, cases with pain and/or ultrasound lesion in the course of the plantar fascia distal to its insertion (not located in the medial process of the posterior calcaneal tuberosity) and cases that had already started some kind of treatment for plantar fasciopathy such as infiltrations, shock waves or previous insoles in the previous 12 months.
All patients were private patients of the Elcano Foot Clinic (Bilbao, Spain) who came to the clinic on a voluntary basis for treatment of heel pain. Data collection was conducted from April 2017 to March 2020. The present study is classified as a prospective observational case series study, which did not alter or exceed the usual or standard clinical practice that had been carried out in this centre for these patients.
Protocol and interventions
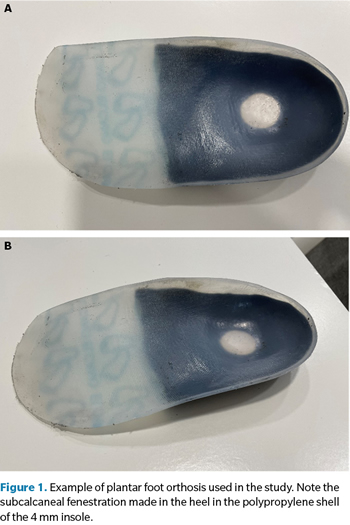
Once the patient met the inclusion criteria, a custom-made foot insole was made following the steps described below after a biomechanical examination of the patient. Initially, a semiweightbearing cast in seated position was taken for all patients in phenolic foam box, looking for the neutral position of the subtalar joint by means of the palpation technique of the head of the talus16. The cast was sent for fabrication with the following prescription in all cases: 1) the plantar orthosis was fabricated in 4 mm polypropylene; 2) a polypropylene rear foot neutral post was used with the idea of leaving the cast in a neutral position (0°) without inversion or eversion of the orthosis; 3) the cup size was increased by about 1 cm; and 4) a 4 mm subcalcaneal fenestration was performed for accommodation of the medial process of the posterior calcaneal tuberosity. This accommodation could be medially or centrally located on the shell depending on the clinical location of the heel pain reported by the patient (Figure 1). Finally, the prescriber also considered fascial accommodation of the shell to avoid irritation of the medial portion of the medial component of the plantar fascia with the insole along the internal longitudinal arch in cases where this was deemed necessary based on the patient’s previous biomechanical examination. A 3 mm Ethyl Vinyl Acetate (EVA) top cover was used in conjunction with 3 mm Poron in the hindfoot in all insoles. All examinations as well as casting and orthotic prescription was performed by the same podiatric clinician with more than 20 years of experience (J.P.H.).
The plantar foot orthoses were delivered to the patients within 10-15 days after the casting with instructions to start using the insoles progressively during the first 3-5 days. During the waiting period for the insoles, patients were instructed to reduce the load on the foot with fasciopathy as much as possible (hours of standing, physical activity, etc.) and to introduce treatment with local ice cryotherapy on the area (10-15 minutes; 3 times/day) and specific stretching exercises of the plantar fascia17. At treatment delivery, patients were instructed to maintain cryotherapy and stretching for as long as they maintained pain. Patients were reviewed at 1 month, 3 months and 6 months. During these reviews, patients were asked to point out areas of discomfort or uncomfortable areas of the insole in order to make adjustments or accommodations to these areas to avoid points of hyper pressure or uncomfortable areas with the insole especially in the heel or inner arch area. Patients were also instructed to come to the clinic earlier if the symptoms worsened with the use of the insoles or if the insoles were not tolerated by the patient for any of the reasons mentioned above.
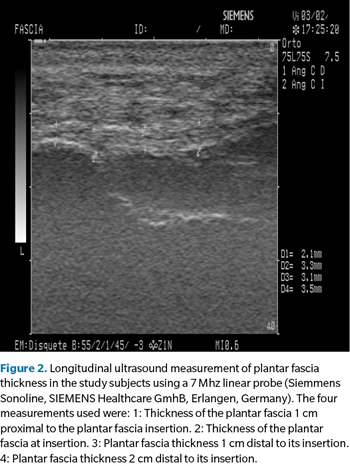
Outcomes
Clinical outcomes were measured using a 20 centimeter-long visual analogue scale (VAS) with 6 graduated images (faces) on one side indicating pain sensations ranging from no pain to extreme pain. On the other side, the scale presented a numerical graduation that corresponded to the different sides shown. This scale is validated and universally accepted as an instrument for measuring pain intensity18,19. Patients assessed the degree of pain in the first steps of the morning in the area of the scale where the images were displayed and the examiner wrote down the numerical value to which the area of the scale selected by the patient corresponded. The thickness of the plantar fascia was also measured sonographycally at 4 different locations in all patients. The ultrasound assessment was performed using an ultrasound with a 7 Mhz linear probe (Siemmens Sonoline, SIEMENS Healthcare GmhB, Erlangen, Germany) with the patient in the supine position where a sagittal section image was taken of the plantar fascia corresponding to the area of greatest thickening in each patient. On this image, measurements of plantar fascia thickness were taken at 4 different locations: plantar fascia thickness 1 cm proximal to insertion, plantar fascia thickness at insertion, plantar fascia thickness 1 cm distal to insertion and plantar fascia thickness 2 cm distal to insertion as described by Pascual et al.20 (Figure 2). Both measurements (VAS and ultrasound) were taken on the first day of the patient’s consultation, which was considered the PRE value, and were repeated at one month, three months and six months of treatment. Likewise, all measurements were taken by the same observer who performed the biomechanical examinations and the prescription of the insoles.
Statistical analysis
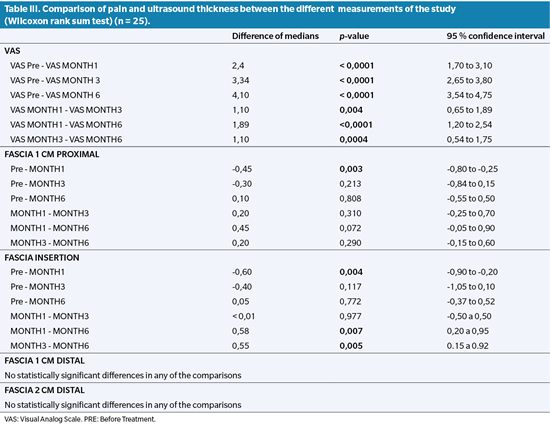
The mean ± standard deviation was calculated for continuous variables and the simple percentage for categorical variables (laterality and sex). The median together with the interquartile range (IQR) of the values obtained on the VAS scale and the thickness of the plantar fascia in the 4 proposed locations before treatment, at 1 month, 3 months and 6 months of treatment were calculated. A significance test was performed on the null hypothesis, which was the absence of statistically significant differences in pain and plantar fascia thickness (in the 4 measurements taken) during the 6 months of follow-up. To perform this test, the Friedman test (non-parametric equivalent to the ANOVA test) was used and in cases where the Friedman test showed statistically significant differences (p < 0.05), a post hoc analysis was performed using the Wilcoxon rank test of all possible combinations where differences could be found (PRE - 1st month, PRE - 3rd month, PRE - 6th month, 1st month - 3rd month, 1st month - 6th month, 3rd month - 6th month, 3rd month - 6th month). The median difference together with the 95 % confidence interval (95 % CI) was calculated for all tests performed for the Wilcoxon test. All calculations were performed using the free software programme R [R Core Team (2021). R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. URL https://www.R-project.org/].
RESULTS
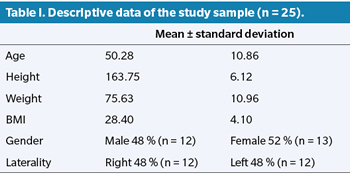
Figure 3 shows the flowchart of the patients who participated in the study. A total of 42 patients were initially included in the study of which 10 were excluded in the first month (8 did not attend the first visit and 2 cases were infiltrated by another professional during that period). Of the 32 cases evaluated at one month, 7 were excluded after 3 months (3 of them were infiltrated during the follow-up period by another professional, 1 case started oral corticosteroid treatment and 3 patients did not attend the successive consultations). Of the 25 cases evaluated at 3 months, 7 patients did not attend the 6-month follow-up, so that only 18 patients were evaluated at 6 months. Data analysis was performed on the cases available at 3 months (n = 25) for Friedman and Wilcoxon test comparisons. In the case of the 6-month comparison for the Friedman and Wilcoxon test, missing data (7 cases) were filled in with the median and RIQ of the 18 cases that completed the 6-month review. Table I shows the descriptive data of the study sample.
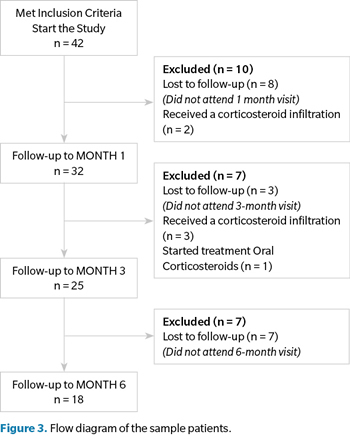
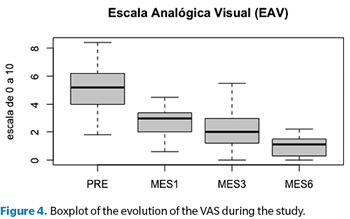
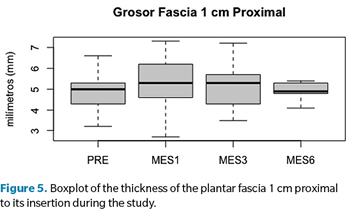
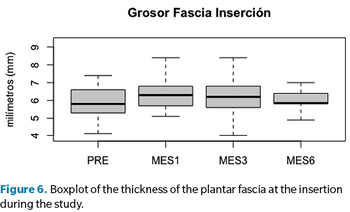
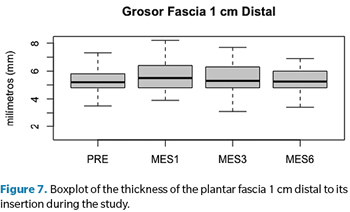
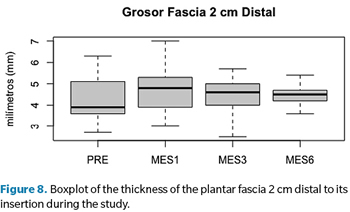
A decrease in VAS pain at 1 month, 3 months and 6 months was statistically significant in all comparisons (Tables II and III). Similarly, statistically significant differences were observed in plantar fascia thickness 1 cm proximal and at the insertion between the PRE assessment and the assessment at 1 month (with increased plantar fascia thickness) and at the insertion between the PRE assessment and at 6 months (with decreased plantar fascia thickness) (Tables II and III). No differences in plantar fascia thickness were found 1 cm distal and 2 cm distal to the insertion in any of the measurements taken. Tables II and III together with pictures 3 to 8 show the results obtained from all measurements taken in the study together with the result of the statistical tests.
DISCUSSION
The effect of plantar orthoses in the treatment of plantar fasciopathy remains controversial at present. Studies show different results in which it is difficult to draw definitive conclusions7,8,11. The present work shows that custom-made insoles made of polypropylene with specific unloading elements could be effective in reducing pain in cases of plantar fasciopathy with a compressive component located in the medial process of the posterior calcaneal tuberosity.
Although plantar foot orthoses are a widely used treatment, especially in the podiatric community, for a large number of foot complaints21-25, we still do not know the exact reasons why insoles are effective in reducing pain26,27, including plantar fasciopathy. It is unclear whether the reduction in pain is due to kinematic changes in foot position or foot motion during dynamic activities, kinetic changes with reduced plantar heel pressure during loading, proprioceptive mechanisms modifying the pattern of muscle activity, other causes, or a combination of all of these. Griffiths and Spooner proposed that the effects of plantar orthoses are mainly attributable to the kinetic changes they produce in the different tissues of the foot and lower limb28. In this regard, the present study has used a type of custom-made orthotic insole centered on this idea with load reduction on the medial process of the posterior calcaneal tuberosity showing a significant improvement in pain within 1-3 months when the insoles are well fitted. Related to these ideas is the idea of plantar orthoses and “custom-made” foot insoles. The concept of a custom-made insole is a noneasy idea to implement and also extremely difficult to standardize among different professionals, especially in the podiatric community, and even more difficult to implement in clinical trials with a control or placebo group29. Different professionals carry out their professional practice with the development and prescription of insoles following different paradigms with different treatment goals to achieve the effect of orthoses. In addition, there is a great variety of materials (soft, semi-rigid, rigid...), construction methodology (mould making, live fitting technique...), specific prescription elements and personal preferences of the prescribing clinicians for the plantar orthosis, which makes it very difficult to standardize the real effect of a plantar orthosis in clinical research, especially when several clinicians are involved. As an example, Whittaker et al. conducted a systematic review with metanalysis in 2017 on the effects of plantar orthoses treatment for heel pain. They analyzed a total of 19 clinical trials and the authors themselves acknowledge a extremely high variability of the plantar orthoses intervention as long as in the 19 trials included in the metanalysis, none or them used the same type of insoles. These issues could be one of the factors to explain the non-significant findings found in certain studies with so-called “custom-made” insoles for plantar fasciopathy30. In the present study, an attempt was made to standardize the effect of the insoles at all times by using the same clinician to make the prescription of the insoles after a personal biomechanical assessment of each patient. The aim was to achieve the same kinetic effect of pressure reduction in the medial process of the posterior calcaneal tuberosity in all patients. This aspect can be considered a strength of the present study compared to other studies in which the types of insoles can be very different from patient to patient.
In the present study, a statistically significant improvement in VAS pain from the start of insole treatment to 6 months follow-up was found in the patients who completed the study (n = 18). This improvement translated clinically into a mean reduction in VAS pain of 2.4 points at month 1 (n = 25), 3.34 at month 3 (n = 25) and 4.10 at month 6 (n = 18). We believe that these changes are clinically relevant and show that the custom-made insoles used in the present study could be effective in the treatment of this entity. It is the authors opinion that pressure reduction at the medial process of the posterior calcaneal tuberosity is key for treatment efficacy. Kirby noted the anatomical importance of the medial process of the posterior calcaneal tuberosity which, because of its more prominent anatomical configuration plantarly, is more prone to have a greater amount of local stress in the area with increased plantar pressures concentrated at that level at the heel12. This increased pressure on the medial process of the posterior calcaneal tuberosity is critical to understand its possible involvement in the pathogenesis of plantar fasciopathy due to increased compressive stress at this level. The plantar orthoses used in this study were made of 4 mm polypropylene with specific elements to reduce pressure in the medial process of the posterior calcaneal tuberosity. These modifications refer to an increase in the positive cast that generates a fenestration or hollow at the level of the medial process of the calcaneus together with an increase in the height of the cup (of approximately 1 cm) that “hugs” the lateral contour of the calcaneus and produces a decrease in pressure on the plantar heel31.
On the other hand, the thickening of the plantar fascia in these patients did not change or showed little change during the 6 months of patient follow-up. In fact, an increase in the thickness of the plantar fascia was observed in 2 of the locations studied (1 cm proximal and at the insertion) in the first month after treatment. These data suggest that the improvement in pain experienced by these patients is not related to the changes in thickness shown by these patients on ultrasound. Other studies have reported the same finding32,33. Although a decrease in the thickness of the plantar fascia at the insertion was observed 6 months after treatment, the change was small and does not seem to be related to clinical improvement in pain, so we understand that fascial thickness may not be the best marker of the evolution of this disorder until it is resolved. The thickness of the plantar fascia at the locations 1 cm and 2 cm distal to its insertion did not undergo any significant change in any of the measurements taken. It is possible that these locations could not be representative of the behaviour of the plantar fascia in individuals with plantar fasciopathy. It is possible that these locations could not be the most appropriate in future studies using plantar fascia thickness as a variable to be studied.
The present study has several important limitations and the results obtained must be interpreted in the context of these limitations. Firstly, the study design was of a prospective case series study and not a clinical trial. The absence of a control group with placebo-type insoles prevents definitive conclusions about the real effect that the insoles used with the specific prescription might have on these patients. Secondly, the number of dropouts from the study is extremely high and after 6 months it exceeds 50 % of the initial sample of subjects who started the study. The authors are aware of this and have no clear explanation as to why this might have happened. All patients were seen at 1 month, 3 months and 6 months after treatment delivery and were instructed to come to the clinic prior to appointments if they were in pain or not adjusting well to treatment. All were also telephoned the day before to check that they were coming to the appointment. The vast majority of the losses did not answer the phone when called the day before and did not attend the check-up appointment either. Some of them reported6 that they were good and did not want to attend the appointment because “they were cured” although it was decided not to include them in the study as there was no assessment of VAS and no assessment of plantar fascia thickness measured by ultrasound. However, the authors also understand that it is possible that some of the losses were due to the fact that they did not feel well with the treatment and gave up using it. The data used have been calculated based on the number of patients available in the third month (n = 25) and we are not sure whether these losses could have positively or negatively influenced the final assessment of pain, but we believe that they could possibly have had an influence. Finally, we understand that assessments of plantar fascia thickness are subject to some degree of variability in ultrasound measurement. This aspect could have some impact on the assessment of plantar fascia thickness reported in the patients despite the fact that we tried to mitigate this variability by always using the same protocol by the same examiner in all patients.
In conclusion, the present study provides data from a small sample of patients with heel pain compatible with unilateral plantar fasciopathy who were treated with rigid custom-made plantar orthoses with a specific prescription for unloading the medial process of the posterior calcaneal tuberosity and increasing the posterior cup in order to reduce the compressive stress at that level. The results showed a statistically significant reduction in pain at 1, 3 and 6 months suggesting that insoles with this type of specific prescription could be effective in symptomatic improvement in these patients. There was a small reduction in plantar fascia thickness at 6 months ultrasonographically which did not specifically correspond to the clinical improvement reported by patients. Further studies in the form of clinical trials showing the actual efficacy of specific types of custom-made plantar orthoses are needed to measure how effective they are in the treatment of plantar fasciopathy.
ETHICAL DECLARATION
This study was approved by the direction comitte of the centre and the study was carried out following all the recommendations of the Declaration of Helsinki, obtaining informed consent from all the participants after a verbal explanation of the project. The conduct of this study did not alter, exceed or modify at any time the usual or standard clinical practice that had been carried out for this type of patient at the healthcare centre where it was performed, and therefore approval by a central ethics committee for clinical research was not requested.
CONFLICT OF INTEREST
The authors declare that they have no conflict of interest relevant to the conduct of this study.
FUNDING
The authors declare that they received no public or private funding for this study.
AUTHORS CONTRIBUTION
JPH and LTV did the conception and design of the paper; JPH, LTV and LPF did the data collection, analysis and interpretation of the results and Final review and acceptance of the manuscript; JPH did the creation drafting and preparation of the manuscript.
REFERENCES
- Hill CL, Gill TK, Menz HB, Taylor AW. Prevalence and correlates of foot pain in a population-based study: the North West Adelaide health study. J Foot Ankle Res. 2008;1(1):2. DOI: 10.1186/1757-1146-1-2.
- Landorf KB. Plantar heel pain and plantar fasciitis. BMJ Clin Evid. 2015;2015:1111.
- Rome K, Howe T, Haslock I. Risk factors associated with the development of plantar heel pain in athletes. Foot. 2001;11(3):119-25. DOI: 10.1054/foot.2001.0698.
- Taunton JE, Ryan MB, Clement DB, McKenzie DC, Lloyd-Smith DR, Zumbo BD. A retrospective case-control analysis of 2002 running injuries. Br J Sports Med. 2002;36(2):95-101. DOI: 10.1136/bjsm.36.2.95.
- Motley T. Plantar Fasciitis/Fasciosis. Clin Podiatr Med Surg. 2021;38(2):193-200. DOI: 10.1016/j.cpm.2020.12.005.
- Schuitema D, Gree C, Postema K, Dekker R, Heijmans JM. Effectiveness of Mechanical Treatment for Plantar Fasciitis: A Systematic Review. J Sport Rehab. 2020;29(5):657-74. DOI: 10.1123/jsr.2019-0036.
- Whittaker GA, Munteanu SE, Menz HB, Tan JM, Rabusin CL, Landorf KB. Foot orthoses for plantar heel pain: A systematic review and meta-analysis. Br J Sports Med. 2018;52(5):322-8. DOI: 10.1136/bjsports-2016-097355.
- Whittaker GA, Munteanu SE, Menz HB, Landorf KB. Should foot orthoses be used for plantar heel pain? Br J Sports Med. 2018;52(5):322-8. DOI: 10.1136/bjsports-2016-097355.
- Morrissey D, Cotchett M, Said J‘Bari A, Prior T, Griffiths IB, Rathleff MS, et al. Management of plantar heel pain: a best practice guide informed by a systematic review, expert clinical reasoning and patient values. Br J Sports Med. 2021;55(19):1106-18. DOI: 10.1136/bjsports-2019-101970.
- Whittaker GA, Munteanu SE, Menz HB, Tan JM, Rabusin CL, Landorf KB. Foot orthoses for plantar heel pain: a systematic review and meta-analysis. Br J Sports Med. 2018;52(5):322-8. DOI: 10.1136/bjsports-2016-097355.
- Rasenberg N, Riel H, Rathleff MS, Bierma-Zeinstra SMA, van Middelkoop M. Efficacy of foot orthoses for the treatment of plantar heel pain: a systematic review and meta-analysis. Br J Sports Med. 2018;52(16):1040-6. DOI: 10.1136/bjsports-2017-097892.
- Kirby KA. Foot and Lower Extremity Biomechanics III: Precision Intricast Newsletters, 2002-2008. Precision Intricast Inc.: Payson, AZ; 2009.
- Kirby KA. Foot and Lower Extremity Biomechanics IV: Precision Intricast Newsletters, 2009-2013. Precision Intricast Inc.: Payson, AZ, 2014.
- von Elm E, Altman DG, Egger M, Pocock SJ, Gotzsche PC, Vandenbroucke JP. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: guidelines for reporting observational studies. Ann Intern Med. 2007;147(8):573-7. DOI: 10.7326/0003-4819-147-8-200710160-00010.
- McMillan AM, Landorf KB, Barrett JT, Menz HB, Bird AR. Diagnostic imaging for chronic plantar heel pain: A systematic review and meta-analysis. J Foot Ankle Res. 2009;2:32. DOI: 10.1186/1757-1146-2-32.
- Michaud TC. Foot orthoses and others forms of conservative foot care. Boston: Williams and Wilkins; 1996.
- Siriphorn A, Sukanya E. Calf Stretching and plantar fascia-specific stretching for plantar fasciitis: A systematic review and meta-analysis. J Body W Mov Ther. 2020;24(4):222-32. DOI: 10.1016/j.jbmt.2020.06.013.
- Dworkin RH, Turk DC, Farrar JT, Haythornthwaite JA, Jensen MP, Katz NP, et al. Core outcomes measures for chronic pain clinical trials: IMMPACT recommendations. Pain. 2005;113(1-2):9-19.
- Younger J, McCue R, Mackey S. Pain Outcomes: A Brief Review of Instruments and Techniques. Curt Pain Headache Rep. 2009;13(1):39-43. DOI: 10.1007/s11916-009-0009-x.
- Pascual-Huerta J, Alarcón-García JM. Effect of gender, age and anthropometric variables on plantar fascia thickness at different locations in asymptomatic subjects. Eur J Radiol. 2007;62(3):449-53. DOI: 10.1016/j.ejrad.2007.01.002.
- Conrad KJ, Budiman-Mak E, Roach KE, Hedeker D, Caraballada R, Burks D, Moore H. Impacts of foot orthoses on pain and disability in rheumatoid arthritics. J Clin Epidemiol. 1996;49(1):1-7. DOI: 10.1016/0895-4356(96)00534-3.
- Munteanu SE, Scott LA, Bonanno DR, Landorf KB, Pizzari T, Cook JL, Menz HB. Effectiveness of customised foot orthoses for Achilles tendinopathy: a randomised controlled trial. Br J Sports Med. 2015;49(15):989-94. DOI: 10.1136/bjsports-2014-093845.
- Kirby KA, Spooner SK, Scherer PR, Schuberth JM. Foot orthoses. Foot Ankle Spec. 2012;5(5):334-43. DOI: 10.1177/1938640012458900.
- Halstead J, Chapman GJ, Gray JC, Grainger AJ, Brown S, Wilkins RA, et al. Foot orhoses in the treatment of symptomatic mid foot osteoarthritis using clinical and biomechanics outcomes: a randomized feasibility study. Clin Rheumatol. 2016;35(4):987-96. DOI: 10.1007/s10067-015-2946-6.
- Tanner C, d´Hooghe P. Foot Orthotic Advances for the Athlete. En: Canata GL, d´Hooghe P, Hunt KJ, et al. (eds.). Sports Injuries of the Foot and Ankle. Berlin: ISAKOS; 2019. p. 407-16.
- Mills K, Blanch P, Chapman AR, McPoil TG, Vicenzino B. Foot orthoses and gait: a systematic review and meta-analysis of literature pertaining to potential mechanisms. Br J Sports Med. 2010;44(14):1035-46. DOI: 10.1136/bjsm.2009.066977.
- Williams DS 3rd, McClay Davis I, Baitch SP. Effect of inverted orthoses on lower-extremity mechanics in runners. Med Sci Sports Exerc. 2003;35(12):2060-8. DOI: 10.1249/01.MSS.0000098988.17182.8A.
- Griffiths IB, Spooner SK. Foot orthoses research: identifying limitations to improve translation to clinical knowledge and practice. Br J Sports Med. 2018;52(6):350. DOI: 10.1136/bjsports-2016-096269.
- Bonanno DR, Landorf KB, Murley GS, Menz HB. Selecting control interventions for use in orthotic trials: The methodological benefits of sham orthoses. Contemp Clin Trials. 2015;42:257. DOI: 10.1016/j.cct.2015.05.008.
- Rasenberg N, Bierma-Zeinstra SMA, Fuit L, Rathleff MS, Dieker A, van Veldhoven P, et al. Custom insoles versus sham and GP-led usual care in patients with plantar heel pain: results of the STAP-study - a randomised controlled trial. Br J Sports Med. 2021;55(5):272-8. DOI: 10.1136/bjsports-2019-101409.
- Chia KK, Suresh S, Kuah A, Ong JL, Phua JM, Seah AL. Comparative trial of the foot pressure patterns between corrective orthotics,formthotics, bone spur pads and flat insoles in patients with chronic plantar fasciitis. Ann Acad Med Singap. 2009;38(10):869-75.
- Bishop C, Thewlis D, HJillier S. Custom foot orthoses improve first-step pain in individuals with unilateral plantar fasciopathy: a pragmática randomised controles trial. BCM Musculoskelet Disord. 2018;19(1):222. DOI: 10.1186/s12891-018-2131-6.
- Las TW, Ma HL, Lee MS, Chen PM, Ku MC. Ultrasonography and clinical outcome comparison of extracorporeal shock wave therapy and corticosteroid injections for chronic plantar fasciitis: A randomized controlled trial. J Musculoskelet Neuronal Interact. 2018;18(1):47-54.