DOI: http://dx.doi.org/10.20986/revesppod.2024.1693/2024
UPDATES
Anatomy and sonopathology of the metatarsophalangeal plantar plate
Anatomía y sonopatología de la placa plantar metatarsofalángica
Javier Alcalá Sanz1
Ana Isabel Marcos Casado1
Jordi Sánchez Mercè2
Bernat Cabestany Perich3
Pedro Nogales Gómez4
1Clínica del Pie Alcalá. Bormujos, Sevilla, España
2Clínica del Peu Maresme. Mataró, Barcelona, España
3Clínica Novamedicum. Sabadell, Barcelona, España
4Clínica Podoactiva Málaga, España
Abstract
The plantar plate of the lesser metatarsophalangeal joints plays a fundamental role in digital stability, maintaining the correct alignment of the finger with its metatarsal and also acting as an achor point of the rest of the articular stabilizing structures. Injury to this specialized ligament precipitates deformity of the lesser toes, especially the second, and is a common reason for consultation in the podiatry clinic. In this article we carry out a detailed review of its anatomical and histological characteristics, its mechanical functions and injury mechanisms as well as its clinical examination and through imaging tests, dedicating a special section to ultrasound, which has emerged in the last decade as a accesible resource and increasingly common in podiatry consultations. Thanks to the use of this technique we can make an economical, real-time, dynamic and more precise diagnosis of the type of injury that occurs in the plantar plate or in the adjacent tissues, from small strains to partial or complete tears accompanied by a greater or less bone damage and inflammation in peripheral soft tissues such as plantar fat pad or flexor tendons. The characterization of the lesions allows us to correlate the etiology with the lesion much better, as well as establish the greater or lesser need for treatment and a more accurate prognosis for each patient.
Keywords: Plantar plate, flexor plate, forefoot anatomy, forefoot pain, metatarsophalangeal predislocation syndrome, claw toe, forefoot sonography
Resumen
La placa plantar de las articulaciones metatarsofalángicas menores juega un papel fundamental en la estabilidad digital, manteniendo la correcta alineación del dedo con su metatarsiano y actuando asimismo de punto de anclaje para el resto de estructuras estabilizadoras de dicha articulación. La lesión de este ligamento especializado precipita la deformidad de los dedos menores, en especial el segundo, y es un motivo de consulta habitual en la clínica podológica. En el presente artículo realizamos una revisión pormenorizada de sus características anatómicas e histológicas, sus funciones mecánicas y mecanismos lesionales, así como su exploración clínica y mediante pruebas de imagen, dedicando un apartado especial a la ecografía que se ha erigido en la última década como un recurso accesible y cada vez más habitual en las consultas de podología. Gracias al uso de esta técnica podemos realizar un diagnóstico económico, en tiempo real, dinámico y más preciso del tipo de lesión que se presenta en la placa plantar o en los tejidos adyacentes, desde pequeñas distensiones hasta roturas parciales o completas acompañadas de un mayor o menor daño óseo e inflamación en los tejidos blandos periféricos, como la grasa plantar o los tendones flexores. La caracterización de las lesiones permite correlacionar mucho mejor la etiología con la lesión, así como establecer la mayor o menor necesidad de tratamiento y un pronóstico más certero para cada paciente.
Palabras clave: Placa plantar, plato flexor, anatomía del antepié, metatarsalgia, síndrome de predislocación metatarsofalángica, dedo en garra, ecografía del antepié
Correspondence: Javier Alcalá Sanz
javialcalasanz@gmail.com
Received: 06-04-2024
Accepted: 14-05-2024
Anatomy and histology of the plantar plate
The plantar plate (i.e. flexor plate, glenoid plate) of the lesser metatarsophalangeal joints plays a crucial role in toe stability, being the main anatomical structure, in synergy with the collateral ligaments, that counteracts the dorsiflexion forces of these joints.
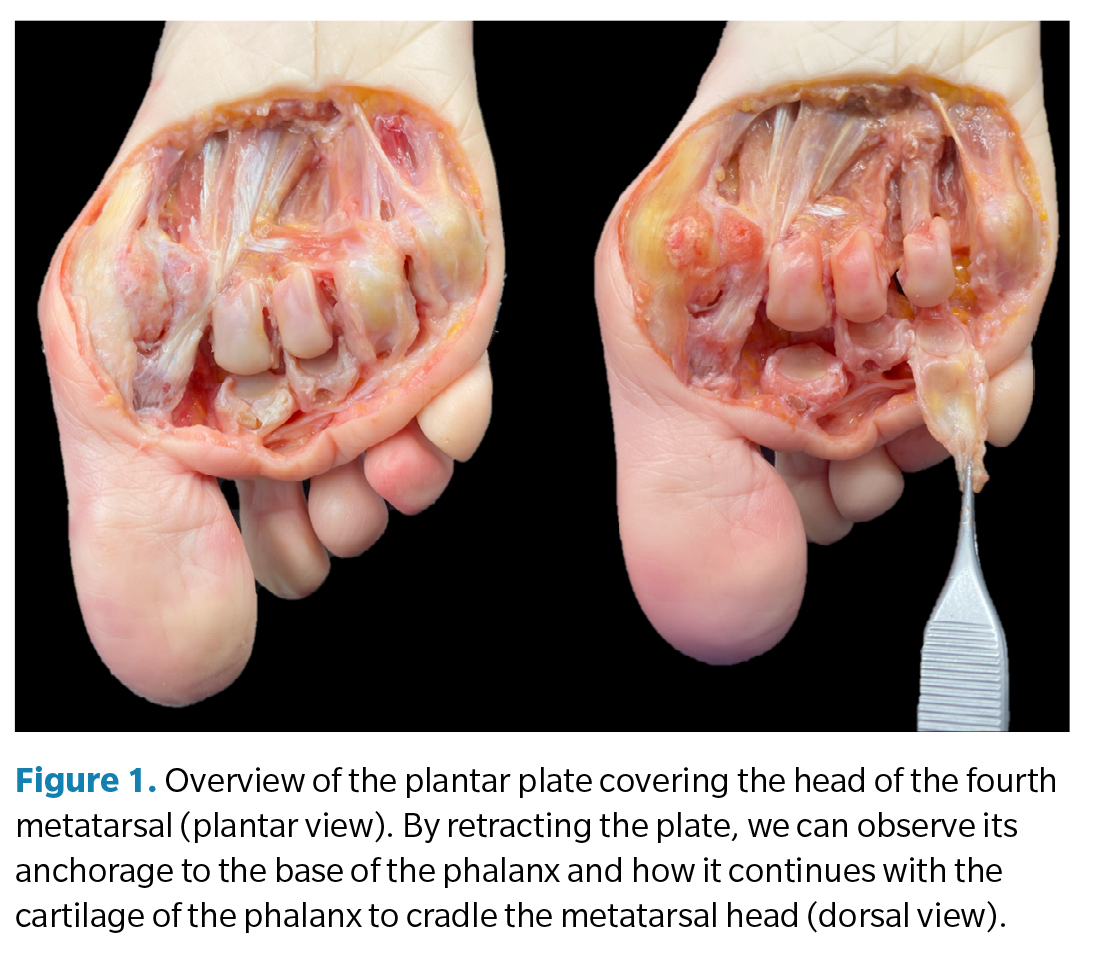
It is a small, highly specialized structure, mainly fibrocartilaginous, that continues the deep terminal zone of the plantar fascia and is firmly anchored to the base of the proximal phalanx of the toes (Figure 1), also providing an anchorage surface for other ligamentous and tendinous structures and, on its plantar side, serving as a passage area for the flexor tendons. Due to its location, characteristics, and function, it is compared to the sesamoids of the first metatarsophalangeal joint(1,2).
Despite its small size, it is a complex structure, firm yet flexible, serving as an anchorage point for the anatomical structures in its region, highlighting its importance in joint stability(3,4). To better understand its anatomy and mechanical function, it is useful to study its different regions in detail, as well as their histological variability(1,2,3,4):
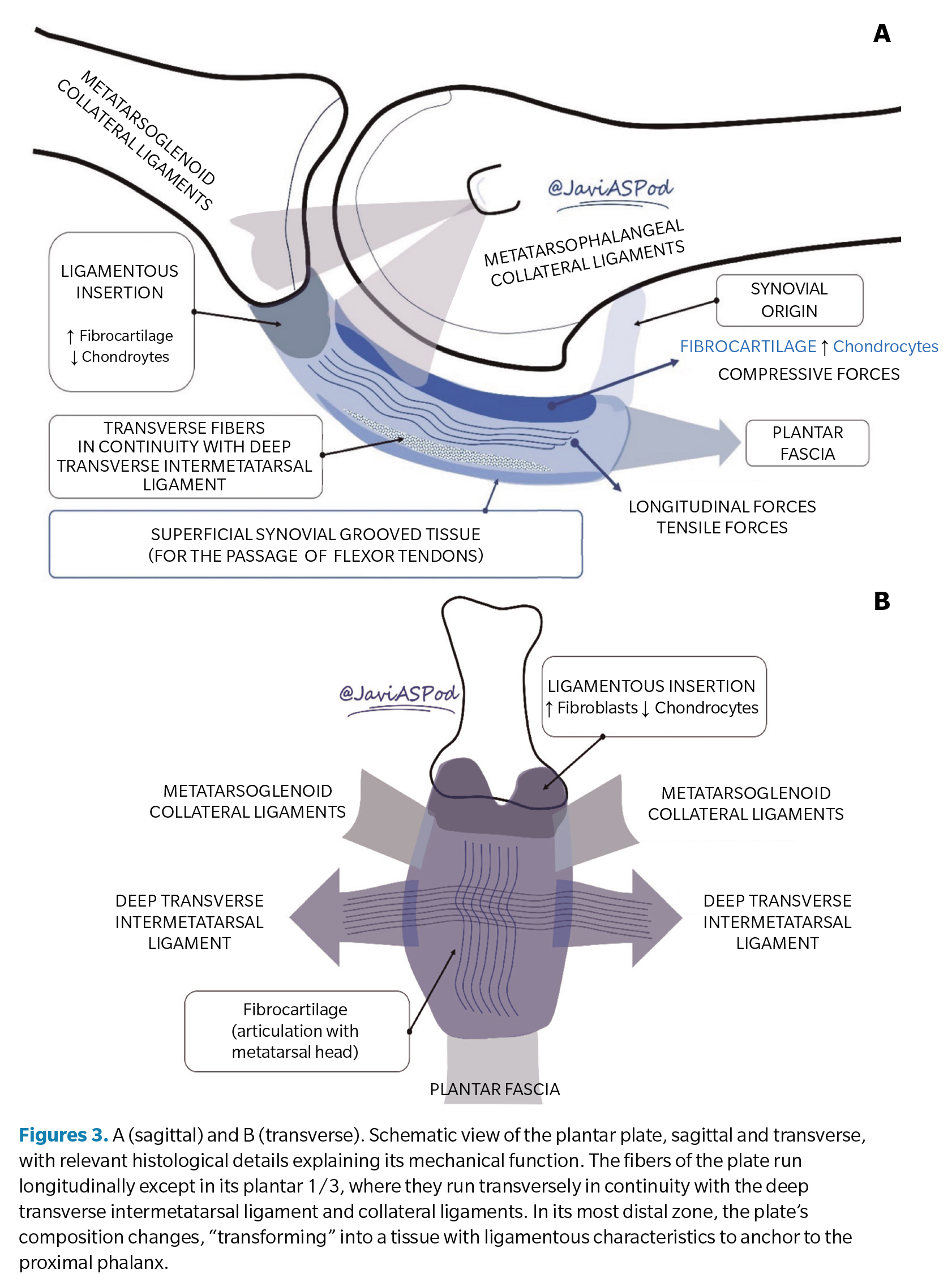
- General characteristics: for the most part, the plantar plate is a fibrocartilaginous tissue mainly composed of type 1 collagen (similar to knee cartilage) and to a lesser extent type 2 (75 vs. 21 %) without elastin fibers2. Its thickness ranges from 2 to 5 mm (greater in its central area), with an average width of 10 mm and an average length of 17-19 mm. In the dorsal 2/3, the fibers are oriented longitudinally, while in its plantar 1/3, they are oriented transversely in continuity with the deep transverse intermetatarsal ligament and collateral ligaments.
- Proximal attachment to the metatarsal: in its proximal area, the plantar plate attaches to the metatarsal neck and head (just proximal to the articular cartilage) through a thin (0.4 mm), fibrous tissue with synovial characteristics.
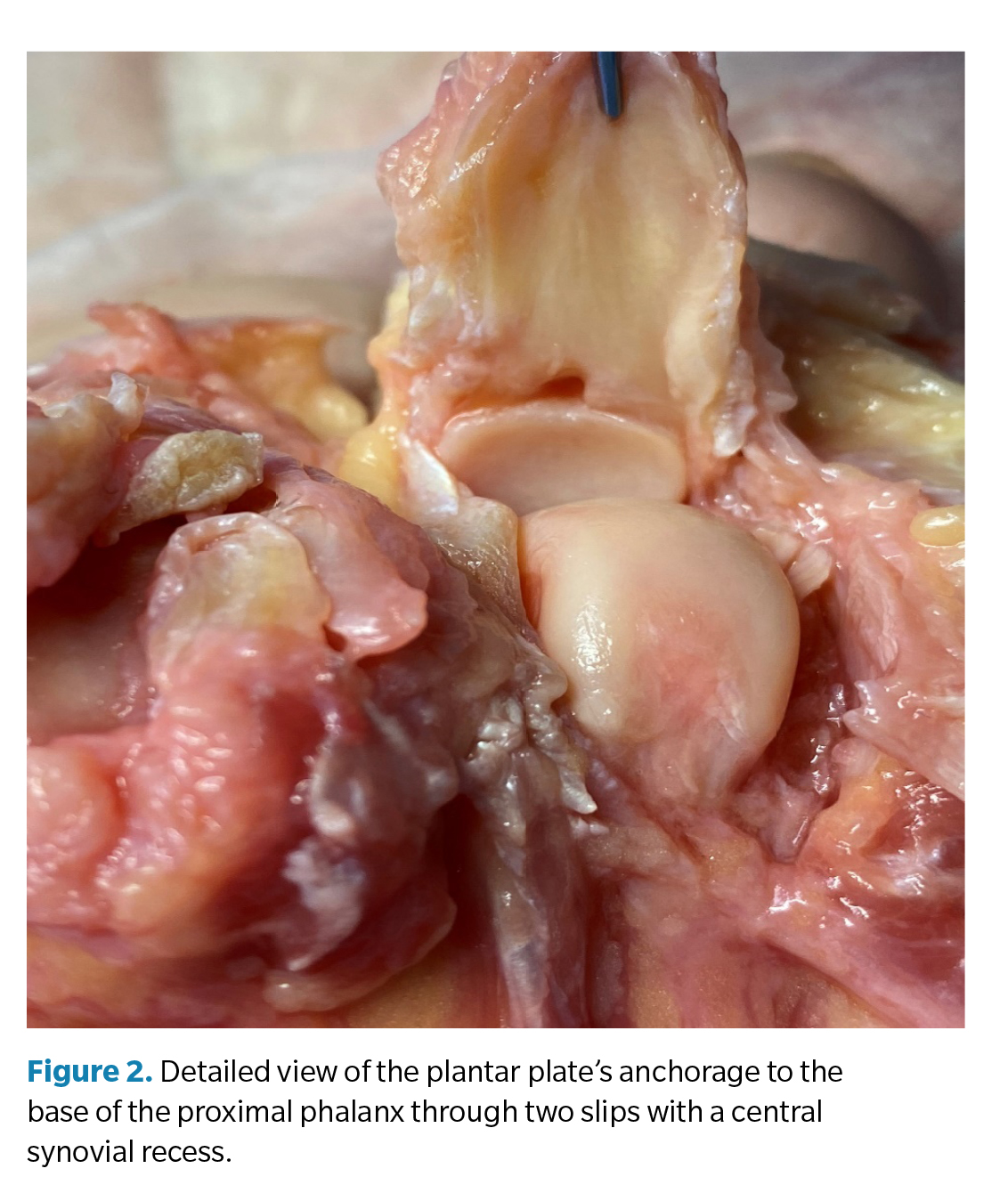
- Distal anchorage to the base of the proximal phalanx: its insertion at the plantar area of the base of the proximal phalanx is strong and composed of a higher proportion of fibroblasts, forming a tissue with ligamentous characteristics(4). The entire thickness of the structure inserts into the bone through two reinforced bands, medial and lateral, and in continuity with the cartilage, forming a concave cavity for the metatarsal head. In its central area, there may be a small central synovial recess that is sometimes confused with pathology in MRI images (pseudo-rupture of the plantar plate) (5) (Figure 2).
- Central portion (midsubstance): in its central portion, it is useful to distinguish between its dorsal 2/3, which are composed of fibrocartilaginous tissue with a higher proportion of chondrocytes, forming an articular surface for the metatarsal head with characteristics similar to the knee meniscus (4,5).
On its plantar side, it forms a channeled structure of fibrous and synovial tissue that serves as a link between the plate and the flexor tendon sheath, allowing their sliding.
- Muscle-ligamentous relationships: the plantar plate serves as a base for the anchorage of different ligamentous structures. In the original description by Kelikian and Sarrafian(6), two collateral ligamentous pathways (medial and lateral) are described, differentiated into metatarsophalangeal fibers (connecting the metatarsal epicondyle with the base of the phalanx) and metatarsoglenoid fibers that connect the epicondyle of the metatarsal head directly with the plate. Both groups of ligaments are intracapsular (Figure 3A). Recently, a different nomenclature for these ligaments has been proposed, distinguishing between proper and accessory collateral ligaments(7).
On the other hand, the plantar plates also act as a union nexus of the different pathways of the deep transverse intermetatarsal ligament, which anchors to both sides of the flexor plate in its most plantar portion, providing consistency to the entire structure (Figure 3B).
Finally, both the interosseous and lumbrical tendons can also project expansions that continue with the plantar plate(2,5).
- Vascularization: the vascularization of the plate has also been studied by different researchers. Gregg et al. 4) established that the blood supply to the plate is mainly through the peripheral plantar area. More recently, Finney et al.(8) have conducted several studies using nano-computed tomography, concluding that the central portion of the plate could be a hypovascularized region, which would explain a higher tendency to pathology in that region as well as the difficulties observed in the healing process. In a more recent article by the same research team, it is suggested that the previously described proximal synovial junction may not simply be a connecting tissue but a pedicle through which around 65 % of the proximal region of the plate is nourished via the metatarsal neck, with significant implications for surgical management(9).
Mechanical functions of the plantar plate
Analyzing the anatomy and tissue composition of the plantar plate, we can better understand the mechanical functions it performs, which we list below:
- Plantar reinforcement of the joint capsule: the metatarsophalangeal joint capsule, well differentiated in its dorsal aspect, fuses with the plantar plate in its plantar aspect, constituting the “floor” of this capsule(5,10).
- Static stabilization of the lesser metatarsophalangeal joints: as previously mentioned, the plantar plates constitute the distal and insertional region of the plantar fascia, which has important biomechanical implications through the so-called reverse windlass mechanism. This mechanism implies that the ground reaction forces acting on the plantar side of the foot tend to flatten the arch and increase the tension of the plantar fascia, resulting in a plantarflexion moment of the proximal phalanx, where it inserts through the plate, acting as a passive stabilizer of the toes on the ground during weight-bearing activities. This effect is not mediated by any muscular activity (nor, therefore, the CNS) but is directly produced by the disposition and characteristics of the plantar fascia and its insertion at the bases of the proximal phalanges. For this reason, the plantar plates, through the reverse windlass mechanism, are the main passive stabilizers of the toes to allow digital grip(11). Following Pauwels’ theory(12) of “causal histogenesis”, collagen fibers always orient themselves in the direction of greatest tension. According to the histological analysis of the plantar plate, most of its fibers are oriented longitudinally in continuity with the fascia fibers, which indicates the design of this structure to primarily resist tensile forces.
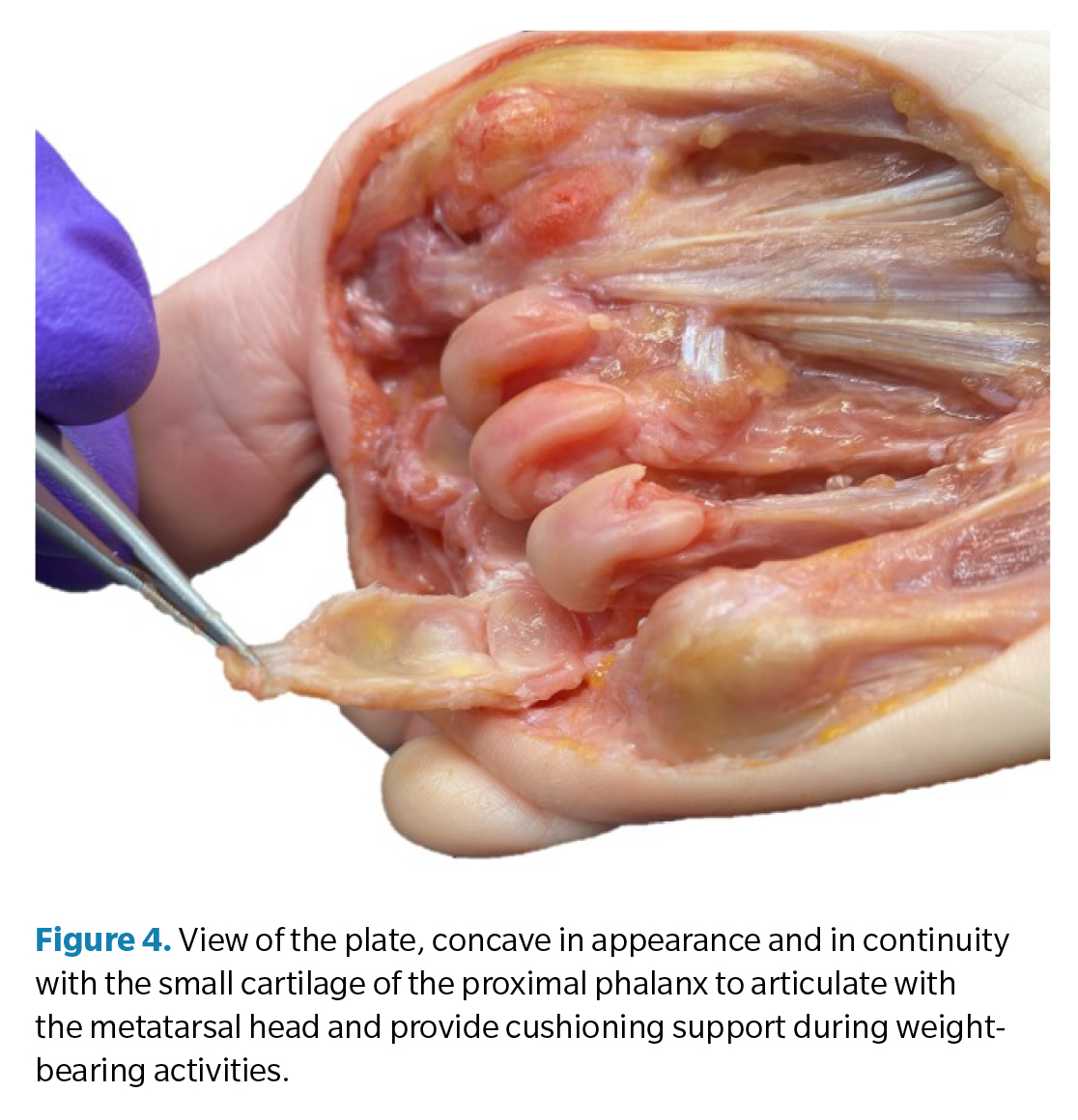
- Prolongation of the phalangeal cartilage and “shock absorber” of the metatarsal head (Figure 4): observing the anatomical relationship of the cartilage at the base of the proximal phalanx and that of the metatarsal head, it is easy to discern the size discrepancy between them. To compensate for this lack, the plantar plate continues the cartilage of the phalanx so that it articulates with the metatarsal head(10). However, its fibrocartilaginous composition, a tissue specialized in compressive force support, also suggests that the plantar plate is not simply a prolongation of the cartilage but rather a shock absorber for the compressive forces generated by the metatarsal head during weight-bearing activities(13).
- Medio-lateral stability: the collateral ligaments (proper and accessory) provide stability to the joint, preventing deviation of the toe in the transverse plane (clinodactyly) and, together with the plate, in the sagittal plane (dorsal dislocation). Various authors have studied the importance of the plantar plate-collateral ligament complex in joint stability by performing cadaver studies in which structures are progressively sectioned and the force required to produce displacement or joint dislocation is measured. In the study by Bhatia and Myerson(14), the sectioning of the plantar plate reduced by 30 % the force needed to vertically displace the proximal phalanx, while the sectioning of the collateral ligaments reduced it by 46 %. A similar study with a larger sample was conducted by Suero et al(15), determining that the sectioning of the plate reduces stability by 19 %, while the sectioning of the collateral ligaments does so by 37 %. The joint sectioning of both structures resulted in a 63 % reduction in stabilizing force in the sagittal plane. From these studies, we can conclude that the collateral ligaments are the most resistant structures in joint stability, although the anchorage of the accessory collateral ligaments to the plate implies that both structures contribute in unison to this stabilization. Barg et al. reached this same conclusion in their 2012 study(16). In 2016, Maas et al. published a systematic review on this issue, gathering information from the referenced studies16. Among their conclusions, they emphasized that, since these studies were conducted on anatomical specimens with acute lesions, the knowledge derived from these experiments may not be a true reflection of clinical situations for chronic injuries (most of the cases we attend in consultation), where the biological healing processes play a relevant role not considered in the conclusions of these studies.
Etiological factors associated with plantar plate pathology
The plantar plate of the second metatarsophalangeal joint is, by far, the most frequently injured. Between 67 % and 90 % of plantar plate tears occur in the second metatarsophalangeal joint, according to some studies(17,18)In most cases, they tend to be chronic degenerative tears in middle-aged and elderly women. Acute or traumatic tears, although possible, are less common and generally confined to young patients with moderate to intense sports activity and repetitive or acute trauma(19).
Various authors have evaluated the etiological factors most related to plantar plate pathology. In 2012, Klein conducted a study to correlate radiological findings with patients undergoing surgery for suspected flexor plate rupture. A sample of 106 feet was obtained, in which 97 of them confirmed the rupture of the flexor plate intraoperatively(20). Of all the variables studied in the preoperative X-rays of these patients, the separation between the second and third toes (splaying toe) and metatarsal protrusion greater than 2 mm were the variables most correlated with feet with plantar plate injury.
In 2016, Fleischer(21) et al. conducted a retrospective case-control study on 100 patients with pathology vs. 200 healthy patients, establishing that a long second metatarsal (metatarsal protrusion index > 4 mm according to Nilsonne’s methodology) is the main risk factor for the development of plantar plate injuries. Other variables studied that were not statistically significant included body mass index, smoking, presence or absence of hallux valgus, intermetatarsal angle, and Seiberg index. However, variables of interest such as the type of usual footwear or level of physical activity were not considered in this study. It is generally accepted that narrow and high-heeled shoes are a predisposing factor as they cause chronic hyperextension forces in the metatarsophalangeal joints, predisposing to the elongation and tearing of the plantar plate(19,21)
The results of the previous study were also corroborated by Mann in 2021(22). In this case, 211 feet were retrospectively analyzed using magnetic resonance imaging to determine the degree of plantar plate injury and conventional X-ray to measure the metatarsal protrusion index following Coughlin’s methodology. The conclusion of this study was similarly that there is a correlation between second metatarsal protrusion (> 5 mm) and plantar plate injury.
Local corticosteroid infiltrations have also been reported as a factor that can trigger the complete rupture of the plantar plate. Although there are no studies to support this statement, there are several case reports where the use of infiltrations was associated with subsequent joint dislocation (23).
Exploration and clinical presentation
For many years, various authors from different disciplines (podiatry, traumatology, physiotherapy, etc.) have referred to frequent cases of inflammatory and incapacitating processes that appear non-traumatic and without systemic involvement of the metatarsophalangeal joints(24). This has led to varied nomenclature until, in 2002, Gerard Yu published his article(25), a classic in our discipline, establishing a relationship of events between the progressive damage of the flexor plate and adjacent structures and the dislocation of the second toe (crossover toe), unifying this timeline of events into a pathology he called the predislocation syndrome of the metatarsophalangeal joints; a term more accepted and used today.
The most common clinical presentation in the initial stages occurs in middle-aged women with focal, acute, or subacute pain on the plantar side of the affected joint. This pain has mechanical characteristics, subsides with rest, and patients may perceive it as a mass they are stepping on. Occasionally, edema can be seen dorsally with a loss of the contour of the extensor tendons, although the peak of pain upon palpation is usually plantar and antecapital (base of the proximal phalanx). It is uncommon for hyperkeratosis or heloma to appear at the dorsal interphalangeal level (although it may present erythema) or at the plantar level of the metatarsal head, which distinguishes this entity from the classic claw toe. Some patients may relate the onset of symptoms to a recent increase in activity or the use of specific footwear for a certain period.
Mobility, both passive and active, is usually not compromised in the early stages, and some patients may experience some relief by plantarflexing the toe. The lack of treatment in these early stages can inexorably lead to the progressive dorsal subluxation of the toe, which, in turn, may be accompanied by transverse deviation, generally towards the medial side, suggesting involvement of the lateral collateral ligaments. As one of the functions of the second toe is to slow the development of HAV, when the toe becomes unstable, HAV can progress significantly, resulting in the establishment of an irreversible dislocation with a characteristic crossover toe(26).
As mentioned before, the combination of the plantar plate and collateral ligaments is the main passive stabilizer of the metatarsophalangeal joint. The intrinsic musculature (lumbricals and interossei) and the extrinsic musculature (extensors and flexors) act as active stabilizers through a balance of forces that largely depends on the position of the proximal phalanx. When the proximal phalanx progressively adopts a dorsiflexed position, the balance of forces between the extrinsic and intrinsic musculature is altered because the insertion of the interossei and lumbricals migrates above the axis of the joint, losing their plantarflexion mechanical advantage(27).
The proximal phalanx can adopt a chronic dorsiflexed position for various reasons and can be a consequence of plantar plate injury or predispose to such an injury. All this leads us to conclude the important role the plantar plate plays as the main stabilizer of the lesser metatarsophalangeal joint.
Clinical tests of interest
Among the clinical tests suggested to evaluate the possible injury of the plantar plate, the “Drawer test” initially proposed by Thompson and Hamilton and the “Paper pull-out test” (digital pressure test) stand out(28). While these tests have clinical, academic, and demonstration interest for the patient, the current use of imaging tests such as ultrasound, which allows direct visualization of the structures, greatly simplifies the diagnostic process in correlation with the previously described clinical findings.
In Yu et al. article(25), a proposal for the classification of predislocation syndrome into three stages related to clinical findings was also made. These classifications have subsequently been enriched and modified based on anatomical and surgical findings, especially by the team of Caio Nery and Michael Coughlin et al. in successive studies(29,30).
While these classifications have evident academic interest, they may not always be precise or easy to establish without imaging tests or intraoperative inspection. Therefore, for the present article, we will focus on ultrasound findings, which we will discuss in the next section.
Sonoanatomy and sonopathology of the plantar plate
Currently, following the recommendations of the European Society of Musculoskeletal Radiology (ESSR), magnetic resonance imaging (MRI) and ultrasound are the two most relevant imaging modalities for the correct imaging diagnosis of plantar plate injuries. Both have a high degree of sensitivity and specificity, leading to a consensus to consider them equivalent in the diagnosis of flexor plate injuries(31).
Conventional X-rays are also routinely used. Although they do not allow visualization of the plate, they do allow observation of the effects of its injury and the collateral ligaments on bone alignment and are essential in surgical planning when performing procedures such as shortening and/or elevation osteotomies.
The main advantage of ultrasound lies in its immediacy and low cost, and the possibility of visualizing the structure in real time and with dynamic stress maneuvers, which allow a better understanding of the injury mechanism. However, MRI allows greater precision in determining the degree of injury, as well as the additional visualization of other structures of interest, such as collateral ligaments, which cannot be assessed by ultrasound(32).
In the last decade, we have seen a very significant increase in publications in this regard(7,33,34,35,36). In 2021, Catherine McCarthy published a review article on ultrasound of the plantar plate, which we will use for this review as a reference article(37). Thus, regarding ultrasound findings related to plantar plate pathology, we will differentiate between direct and indirect findings.
Examination technique
As in any ultrasound examination, we acquire longitudinal and transverse views (long and short axes). In general, dynamic longitudinal images provide the most information about the integrity of the plate. For this, it is useful to dorsiflex the toe with the passive hand, tensioning the plate, which changes from a curved appearance to a more linear and better-defined aspect.
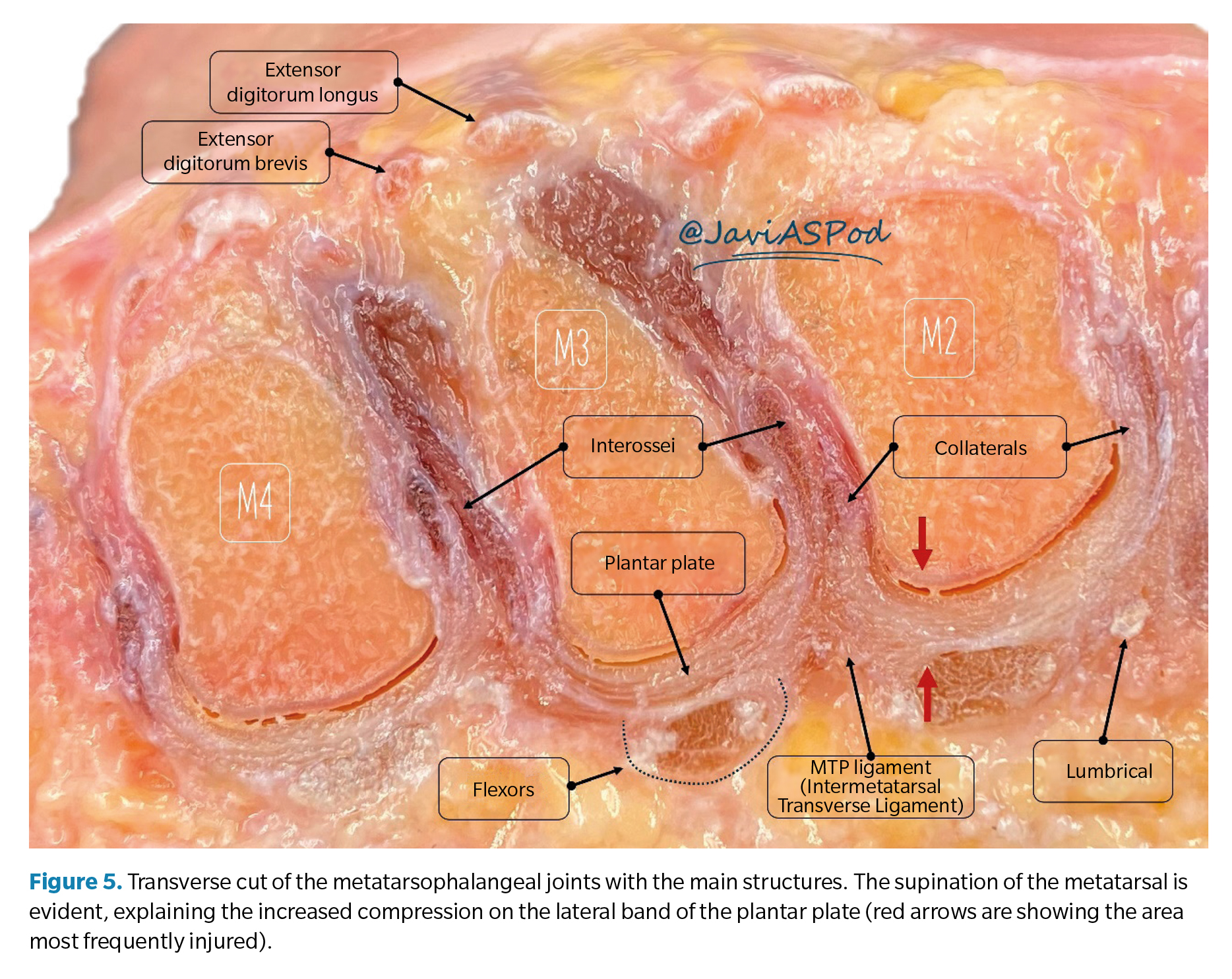
On the other hand, it is important to perform sweeps in the lateral-medial direction. Tears are most frequently described initially along the lateral insertional band of the plantar plate, with purely central or medial tears being less common and usually appearing when the injury progresses from the lateral band. This is explained because the lesser metatarsals are relatively supinated, and the lateral condyle is positioned more plantarly than the medial condyle, concentrating compressive forces on the lateral band of the plate(7) (Figure 5). Similarly, this finding corresponds with the tendency of the second toe to deviate medially since the progressive failure in the plate, collateral ligament, and lateral capsule favors medial side contracture, predisposing to the formation of the crossover toe(38).
Finally, it is always useful to perform comparative ultrasounds with the plantar plate of the contralateral foot when it is asymptomatic, especially if there are doubts about a less conclusive injury during the examination.
Normal criteria for ultrasound images
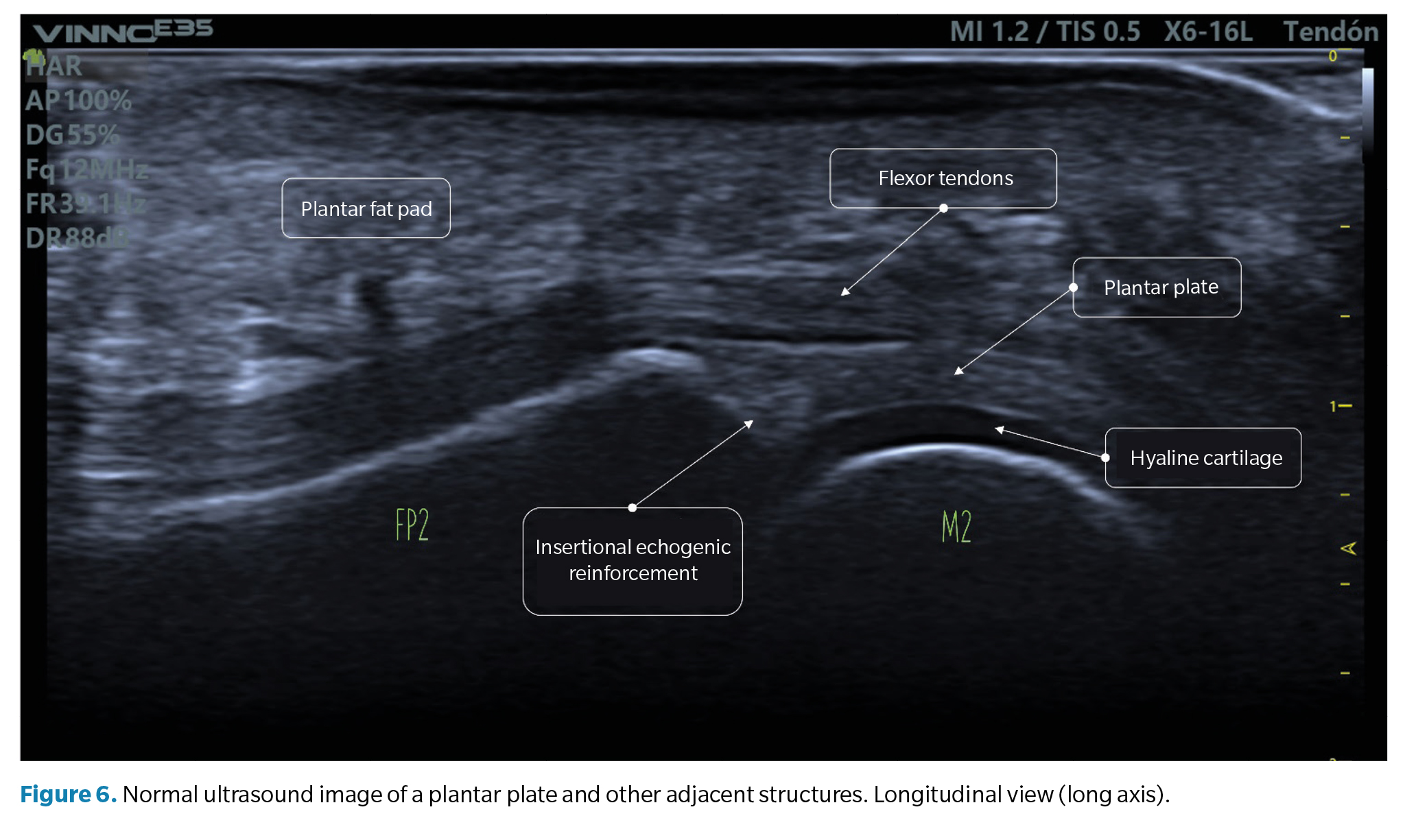
- Longitudinal view (long axis): the normal plantar plate appears on ultrasound as a slightly echogenic curvilinear structure with a homogeneous granular echotexture. This texture allows differentiation, not always well-defined, from the underlying flexor tendons with a fibrillar texture. The articular surface of the plate is precisely defined, bordering the hypoechoic hyaline cartilage of the metatarsal head (Figure 6).
At the junction with the proximal phalanx, which is well-defined, the bone contour is usually smooth, and a more echogenic triangular area may appear in the plate, described as a normal ultrasound finding and possibly representing a higher proportion of collagen fibers. The proximal junction with the metatarsal neck, however, has poor definition on the ultrasound image (Figure 6).
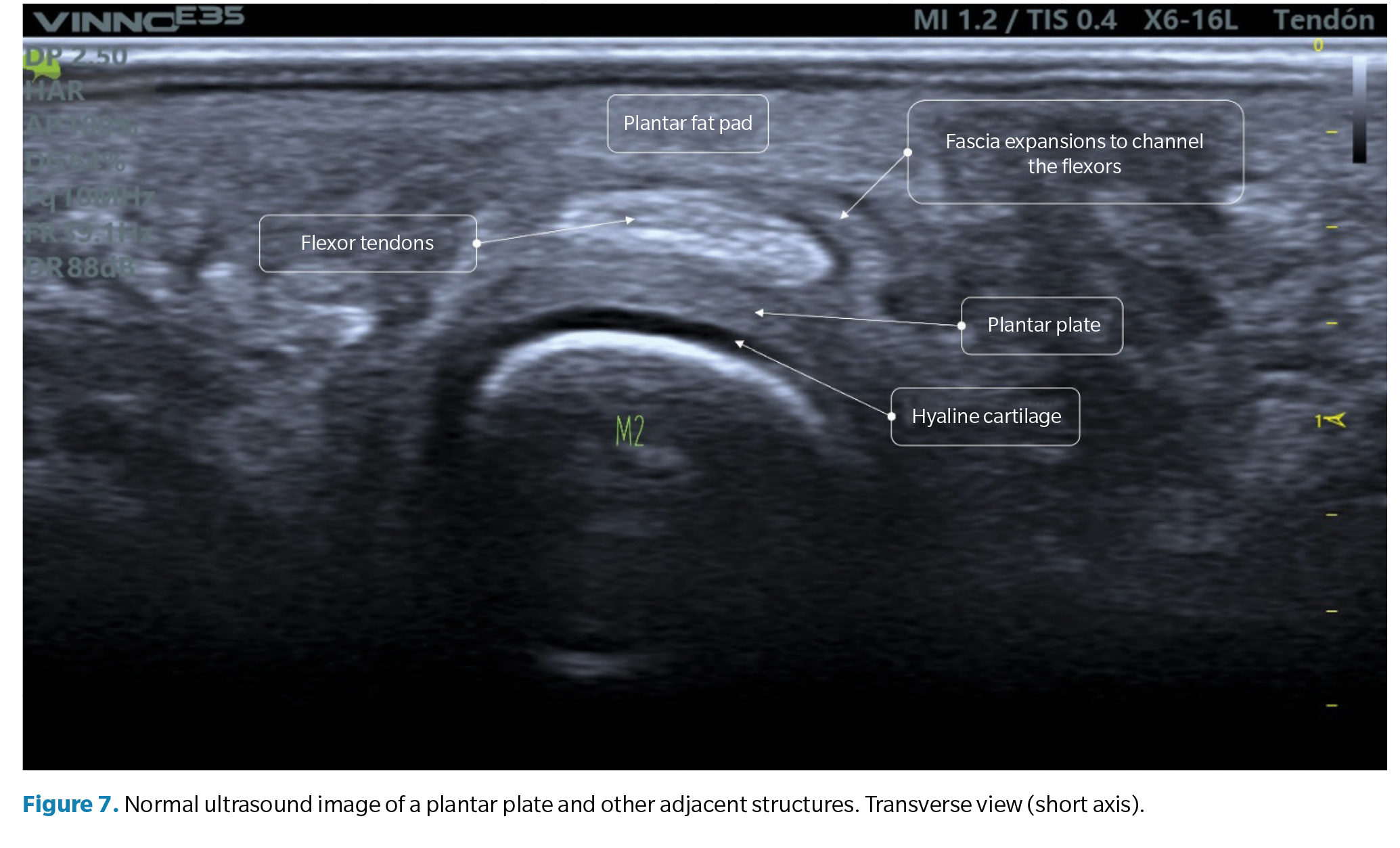
- Transverse view (short axis): the plantar plate will have a curved shape that cradles the metatarsal head. The echotexture is equally granular, although in this exam, the mottled appearance may be more heterogeneous, reflecting the longitudinal arrangement of collagen bundles. The flexor tendons can be seen over the plate and can be easily identified using anisotropy maneuvers (Figure 7).
Direct ultrasound findings
Plantar plate tears can show in different ways on ultrasound, affecting the structure partially or completely.
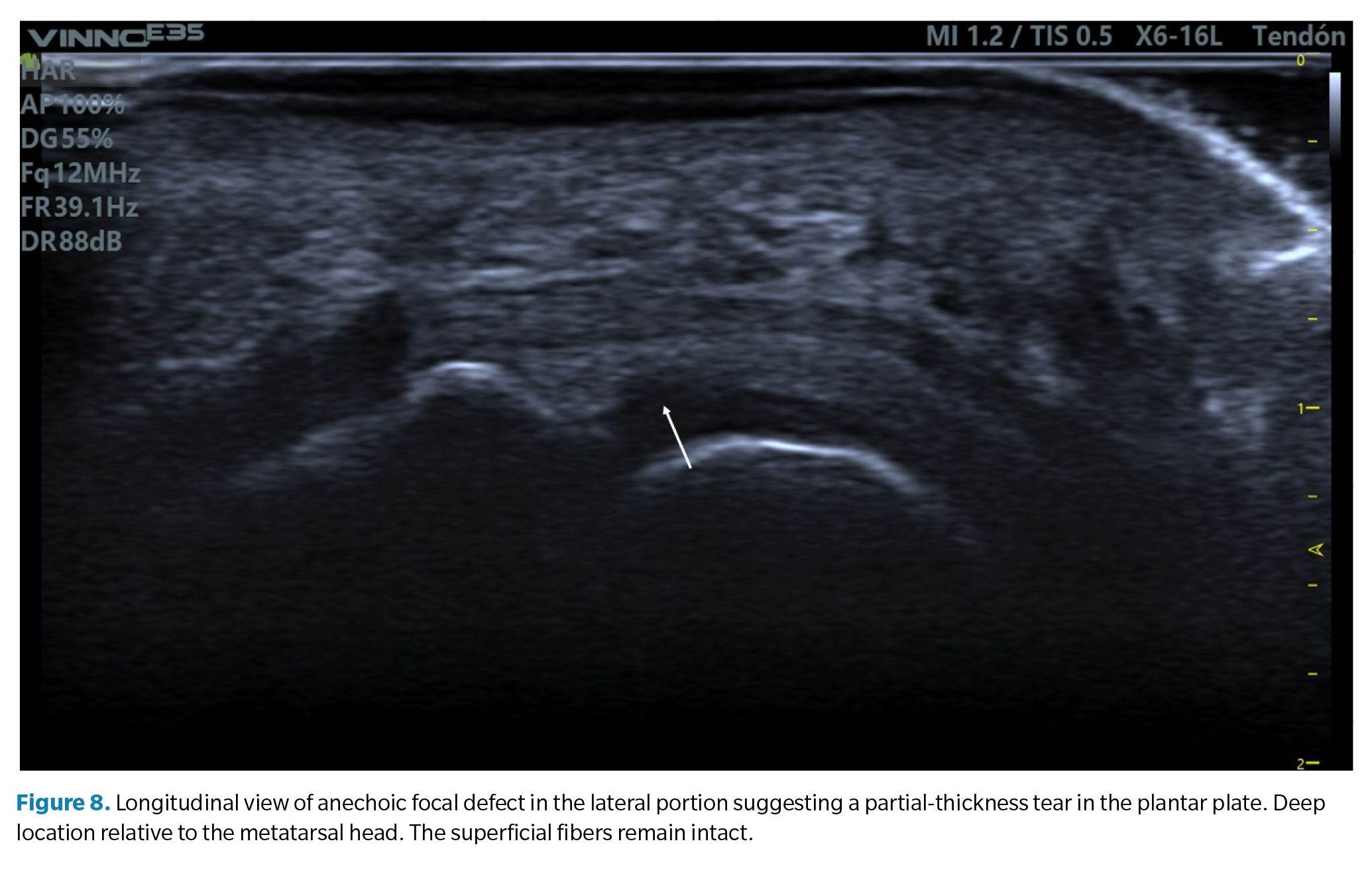
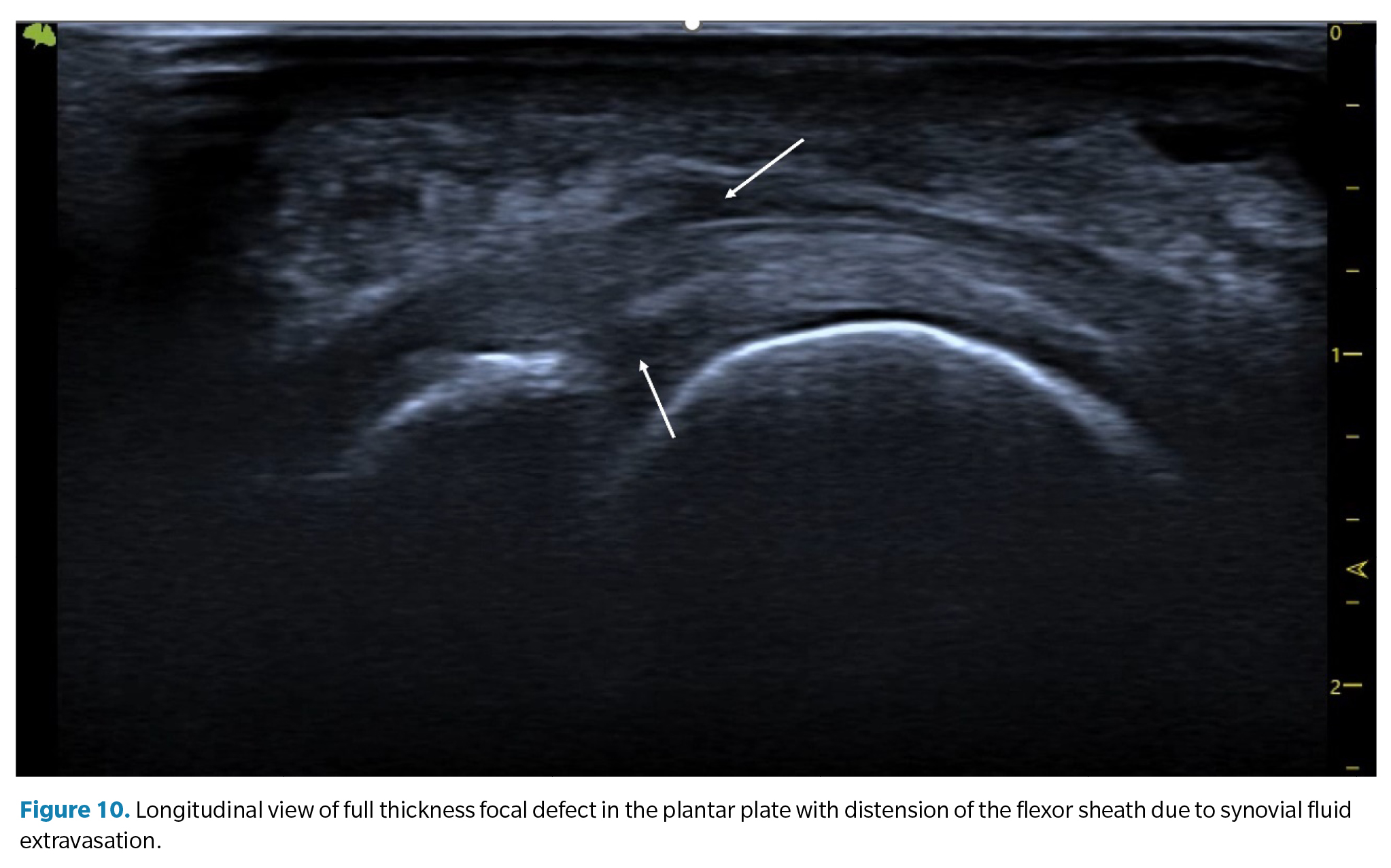
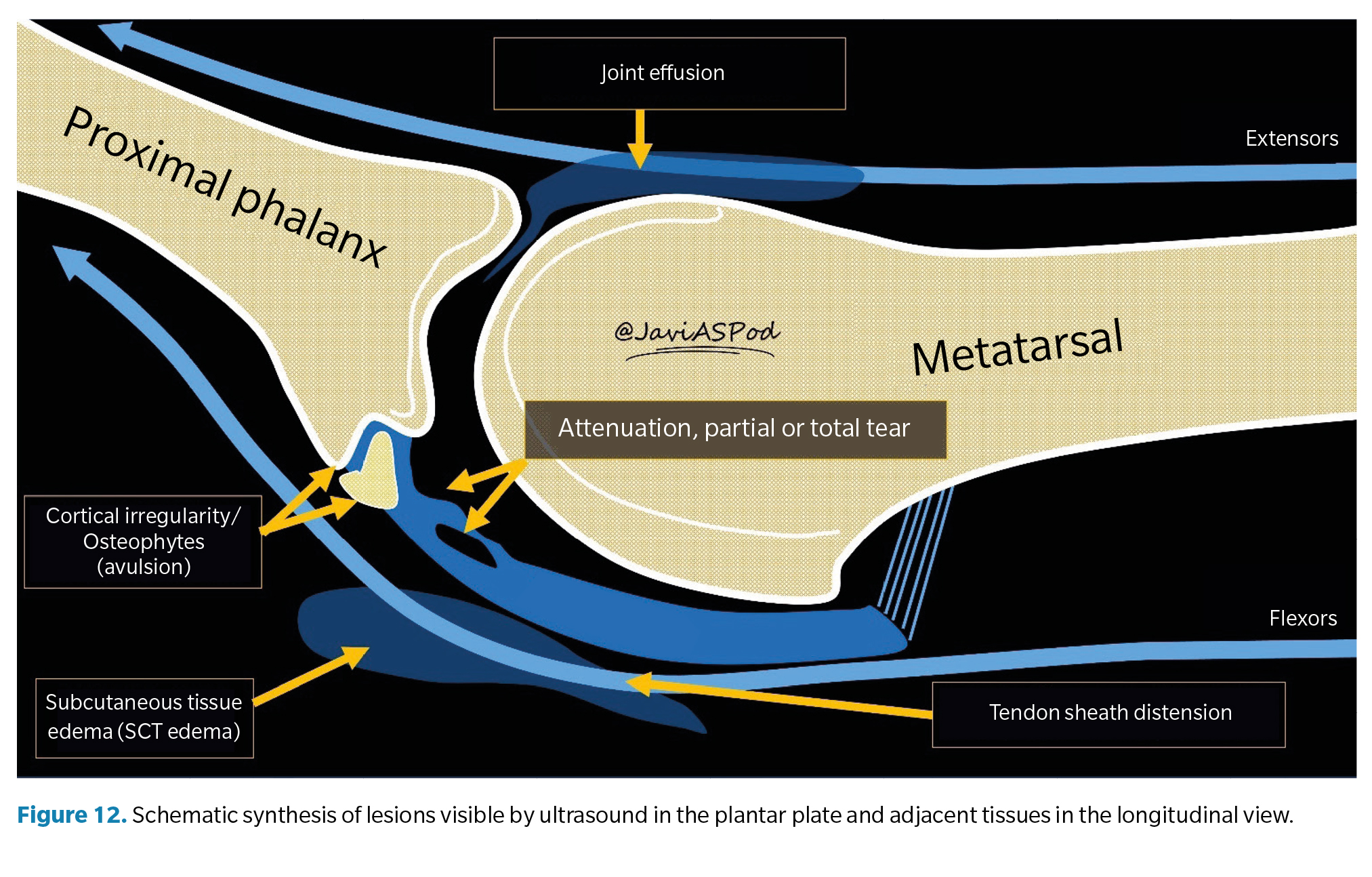
- Anechoic or hypoechoic focal defect. They appear as a discrete cleft in the deep tissue area (the area that articulates with the metatarsal head) on its lateral margin. When the superficial fibers are intact, it is called a partial-thickness tear, while a tear that traverses the entire tissue to its superficial region is called a full-thickness tear(39) (Figure 8).
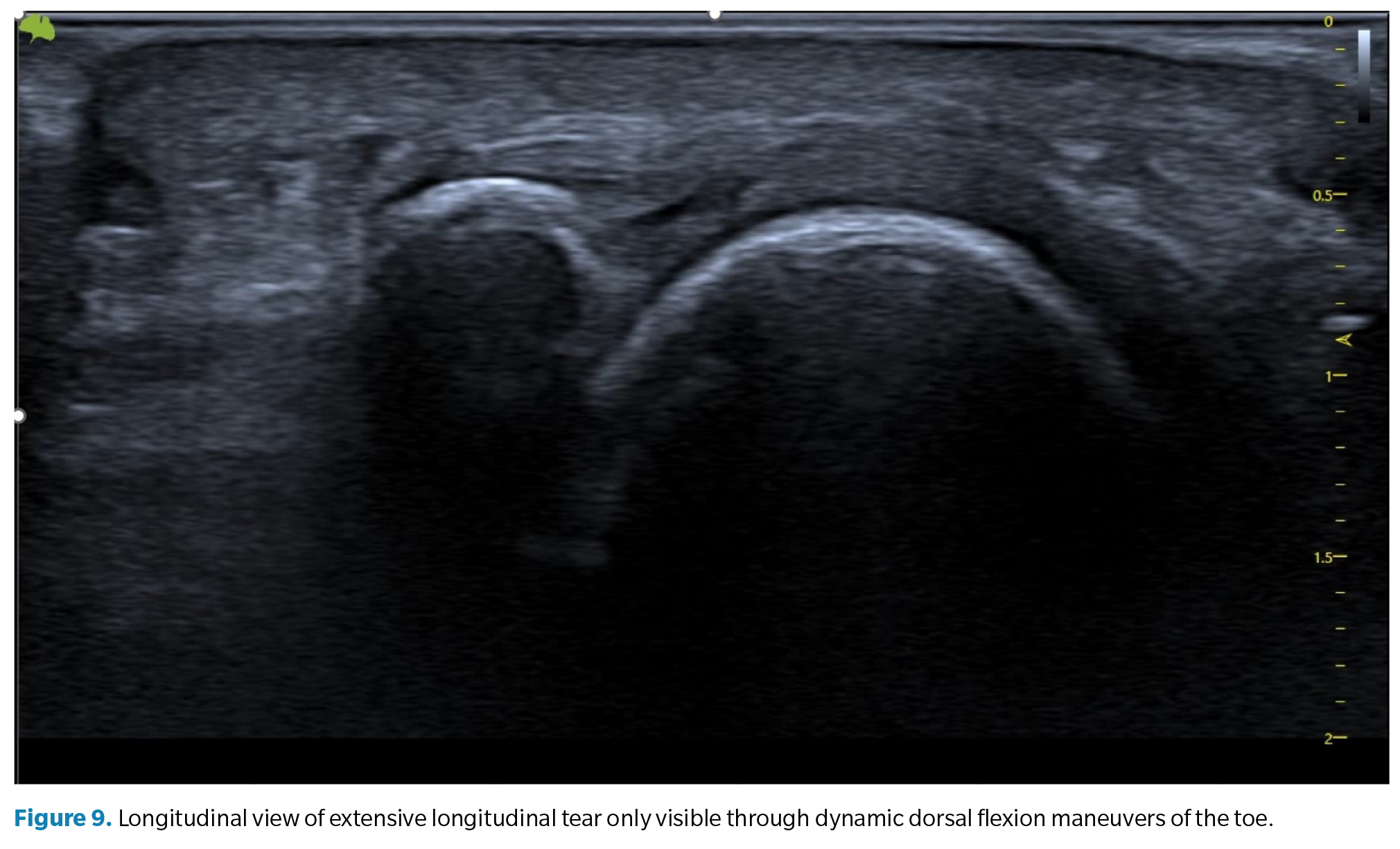
- Flattening and attenuation of the plantar plate. In these cases, a clear defect is not observed, but attention should be paid when the insertion area, usually thicker, appears thinner than the middle or proximal area of the plate. This generally suggests the presence of a transverse tear extending from the lateral portion to the central portion of the plate(40) (Figure 9).
- Non-visualization of the plantar plate. The non-visualization of the plantar plate may indicate a complete transverse tear with tissue retraction, often associated with dorsal dislocation of the proximal phalanx.
As mentioned, in all cases, dynamic maneuvers to tense the toe (and the plate) are essential to establish the presence and extent of a tear(41,42). The inability to tense the plate (transition from a curved to a linear state) and the loss of congruent movement between the proximal phalanx and the plate are very suggestive signs of a tear that can only be appreciated with these maneuvers.
Indirect ultrasound findings
- Plantar or dorsal joint fluid (synovitis). Synovial effusion. Since the plantar plate forms the plantar closure of the joint capsule, tears in the plate can lead to a significant increase in synovial fluid, which manifests as a detectable synovial effusion both dorsally and plantarly. In some cases, this fluid can leak into the flexor tendons, creating a hypoechoic halo around them resembling the characteristic image of tenosynovitis with distension of the tendon sheath (Figure 10).
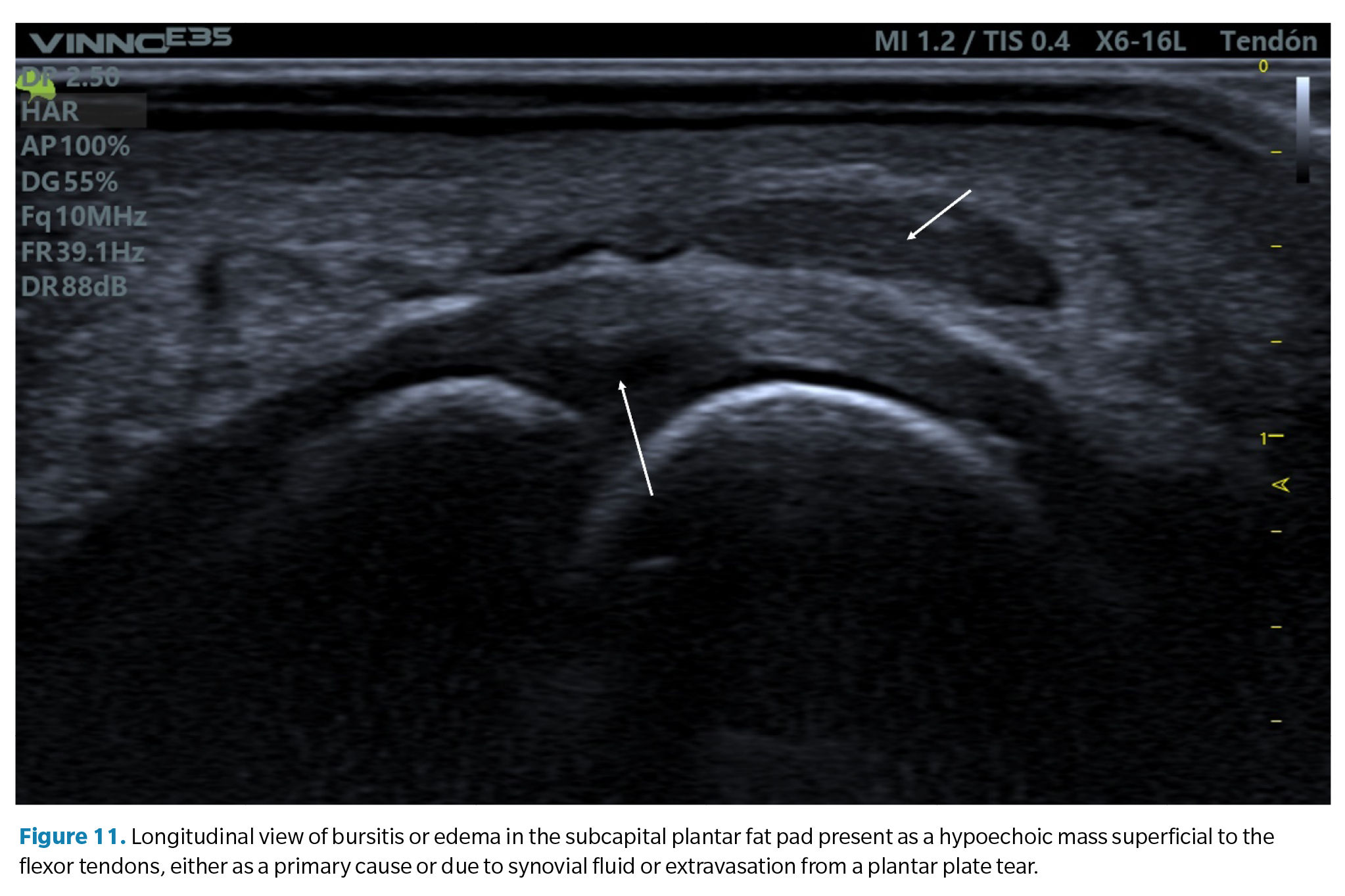
- Bursitis of the plantar fat pad. In relation to the previous finding, some cases of plantar plate tears may also be accompanied by a hypoechoic infiltrate in the adjacent plantar fat pad. This may be a primary defect due to excessive compression of the fat (compression which is also part of the compressive injury etiology of the plate) or the result of a synovial fluid infiltrate due to capsular rupture extravasation as previously mentioned. It is common in these cases to detect a positive <
- Echogenic enthesophytes in the proximal phalanx. In advanced stages, it is common to see marked irregularity of the plantar cortex of the proximal phalanx base and the presence of enthesophytes associated with plantar plate tears, similar to other ligaments where traction can cause avulsion of the bone tissue(43) (Figure 12).
Conclusions
As a conclusion to this review, we will address a classic debate in our discipline about which forces predominate in plantar plate injuries. As we have seen, the plate is an ultra-specialized tissue, and from its anatomical arrangement and histological composition, we can deduce that it is prepared to withstand both compressive and tensile forces. How or to what extent one predominates over the other will likely depend on the characteristics of each patient.
Arguments in favor of the predominance of compressive forces are based on the fact that the most clearly established etiological factor in the scientific literature is the presence of a long second metatarsal or a short first metatarsal. In both cases, the excess metatarsal protrusion or insufficiency of the first ray increases compressive forces on the head of the second metatarsal. This, in turn, corresponds to a common injury pattern observed in ultrasound: focal lesions in the deep central portion (midsubstance) of the plate on its lateral margin, where the metatarsal condyle compresses more forcefully.
However, in another distinct group of patients, we observe that the injuries tend to be more distal, in the purely ligamentous area of the plate, and associated with irregularities of the phalanx cortex and even bone avulsion injuries and enthesophytes, suggesting a traction injury mechanism and therefore tensile force predominance. Additionally, in many patients, the implementation of plantar flexion splinting of the toe using buddy taping or devices designed for this purpose, neutralizing dorsiflexion forces, results in very significant symptomatic relief.
Another factor that has been little studied in this and other pathologies is the loss of competence of the plantar fat pad to absorb and dissipate compressive forces during weight-bearing activities. This could explain why certain injuries on the plantar foot have similar demographic characteristics in terms of their age of onset, which coincides with the time when the plantar fat pad undergoes significant deterioration both quantitatively and qualitatively, thus increasing compressive forces on internal tissues and predisposing them to injury.
Certainly, both tensile and compressive forces contribute in varying proportions depending on each patient’s anatomical characteristics and activity level, from which we can deduce whether the injury mechanism is more pronounced in the second or third rocker. It is the clinician’s duty to establish the predominance of one or the other to determine the diagnosis based on clinical examination and history. However, at present, with the accessibility of imaging tests such as ultrasound, it is highly advisable to establish the degree of injury and its prognosis to decide the most appropriate treatment in each case.
References
- Deland JT, Lee KT, Sobel M, Dicarlo EF. Anatomy of the Plantar Plate and Its Attachments in the Lesser Metatarsal Phalangeal Joint. Foot Ankle Int. 1995;16(8):480-6. DOI: 10.1177/107110079501600804.
- Johnston RB, Daniels T, Smith J. The Plantar Plate of the Lesser Toes: An Anatomical Study in Human Cadavers. Foot Ankle Int. 1994;15(5):276-82. DOI: 10.1177/107110079401500508.
- Hatch DJ. Anatomy: Plantar Plate. Clin Podiatr Med Surg. 2022;39(3):411-9. DOI: 10.1016/j.cpm.2022.02.004.
- Gregg J, Marks P, Silberstein M, Schneider T, Kerr J. Histologic anatomy of the lesser metatarsophalangeal joint plantar plate. Surg Radiol Anat. 2007;29(2):141-7. DOI: 10.1007/s00276-007-0188-2.
- Mohana-Borges AVR, Theumann NH, Pfirrmann CWA, Chung CB, Resnick DL, Trudell DJ. Lesser Metatarsophalangeal Joints: Standard MR Imaging, MR Arthrography, and MR Bursography—Initial Results in 48 Cadaveric Joints. Radiology. 2003;227(1):175-82. DOI: 10.1148/radiol.2271020283.
- Kelikian AS, Sarrafian SK. Sarrafian’s anatomy of the foot and ankle?: descriptive, topographical, functional. 3ª ed. Wolters Kluwer Health/Lippincott Williams & Wilkins (ed); 2011. p. 759.
- Nery C, Baumfeld D, Umans H, Yamada AF. MR Imaging of the Plantar Plate. Magn Reson Imaging Clin N Am. 2017;25(1):127-44. DOI: 10.1016/j.mric.2016.08.007.
- Finney FT, McPheters A, Singer NV, Scott JC, Jepsen KJ, Holmes JR, et al. Microvasculature of the Plantar Plate Using Nano–Computed Tomography. Foot Ankle Int. 2019;40(4):457-64. DOI: 10.1177/1071100718816292.
- Park JV, Finney FT, Singer NV, Saunders NE, Walley KC, Holmes JR, et al. Proximal Plantar Plate of Lesser Toe Metatarsophalangeal Joint Vascular Supply. Foot Ankle Int. 2023;44(1):75-80. DOI: 10.1177/10711007221140043.
- Viladot Voegeli A, Gasch Blasi J. La placa plantar. Rev Pie Tobillo. 2015;29(1):2-10. DOI: 10.1016/S1697-2198(16)30002-7.
- Kirby KA. Biomecánica del pie y la extremidad inferior V: Artículos de Precisión Intricast. 2014-2018. Smith JJ (ed.). Payson (Arizona): Precision Intricast Inc; 2019. p. 1-157.
- Pauwels F. Biomechanics of the Locomotor Apparatus. Berlin, Heidelberg: Springer Berlin Heidelberg; 1980.
- Barg A, Courville XF, Nickisch F, Bachus KN, Saltzman CL. Role of collateral ligaments in metatarsophalangeal stability: A cadaver study. Foot Ankle Int. 2012;33(10):877-82. DOI: 10.3113/FAI.2012.0877.
- Bhatia D, Myerson MS, Curtis MJ, Cunningham BW, Jinnah RH. Anatomical restraints to dislocation of the second metatarsophalangeal joint and assessment of a repair technique. J Bone Joint Surg. 1994;76(9):1371-5. DOI: 10.2106/00004623-199409000-00012.
- Suero EM, Meyers KN, Bohne WHO. Stability of the metatarsophalangeal joint of the lesser toes: A cadaveric study. J Orthop Res. 2012;30(12):1995-8. DOI: 10.1002/jor.22173.
- Maas NMG, van der Grinten M, Bramer WM, Kleinrensink GJ. Metatarsophalangeal joint stability: A systematic review on the plantar plate of the lesser toes. J Foot Ankle Res. 2016;9:32. DOI: 10.1186/s13047-016-0165-2.
- Umans H, Srinivasan R, Elsinger E, Wilde GE. MRI of lesser metatarsophalangeal joint plantar plate tears and associated adjacent interspace lesions. Skeletal Radiol. 2014;43(10):1361-8. DOI: 10.1007/s00256-014-1920-8.
- Nery C, Coughlin MJ, Baumfeld D, Mann TS. Lesser metatarsophalangeal joint instability: Prospective evaluation and repair of plantar plate and capsular insufficiency. Foot Ankle Int. 2012;33(4):301-11. DOI: 10.3113/FAI.2012.0301.
- Linklater JM, Bird SJ. Imaging of Lesser Metatarsophalangeal Joint Plantar Plate Degeneration, Tear, and Repair. Semin Musculoskelet Radiol. 2016;20(2):192-204. DOI: 10.1055/s-0036-1581115.
- Klein EE, Weil L, Weil LS, Knight J. The Underlying Osseous Deformity in Plantar Plate Tears: A Radiographic Analysis. Foot Ankle Spec. 2013;6(2):108-18. DOI: 10.1177/1938640012463060.
- Weil L, Fleischer AE, Klein EE, Ahmad M, Shah S, Catena F, et al. Association of Abnormal Metatarsal Parabola with Second Metatarsophalangeal Joint Plantar Plate Pathology. Foot Ankle Int. 2017;38(3):289-97. DOI: 10.1177/1071100716674671.
- Mann TS, Nery C, Baumfeld D, Fernandes EA. Is second metatarsal protrusion related to metatarsophalangeal plantar plate rupture? Am J Roentg. 2021;216(1):132-40. DOI: 10.2214/AJR.19.22563.
- Ito E, Shima H, Togei K, Hirai Y, Tsujinaka S, Yasuda T, et al. Dislocations of the second and third metatarsophalangeal joints after local steroid injection in patients with refractory metatarsalgia: A case report. SAGE Open Med Case Rep. 2021;9:2050313X211046744. DOI: 10.1177/2050313X211046744.
- Mann RA, Mizel MS. Monarticular Nontraumatic Synovitis of the Metatarsophalangeal Joint: A New Diagnosis? Foot Ankle. 1985;6(1):18-21. DOI: 10.1177/107110078500600104.
- Yu GV, Judge MS, Hudson JR, Seidelmann FE. Predislocation Syndrome Progressive Subluxation/Dislocation of the Lesser Metatarsophalangeal Joint. JAPMA. 2002;92(4):182-99.
- Butterworth ML, Block AJ. Update on Fibrocartilaginous Disease Clinical Examination. Clin Podiatr Med Surg. 2022;39(3):371-92. DOI: 10.1016/j.cpm.2022.03.002.
- Dalmau-Pastor M, Fargues B, Alcolea E, Martínez-Franco N, Ruiz-Escobar P, Vega J, et al. Extensor apparatus of the lesser toes: Anatomy with clinical implications - Topical review. Foot Ankle Int. 2014;35(10):957-69. DOI: 10.1177/1071100714546189.
- Doty JF, Coughlin MJ, Weil L, Nery C. Etiology and management of lesser toe metatarsophalangeal joint instability. Foot Ankle Clin. 2014;19(3):385-405. DOI: 10.1016/j.fcl.2014.06.013.
- Nery C, Coughlin M, Baumfeld D, Raduan F, Mann TS, Catena F. How to classify plantar plate injuries: parameters from history and physical examination. Rev Bras Ortop (English Edition). 2015;50(6):720-8. DOI: 10.1016/j.rboe.2015.10.009.
- Nery C, Umans H, Baumfeld D. Etiology, Clinical Assessment, and Surgical Repair of Plantar Plate Tears. Semin Musculoskelet Radiol. 2016;20(2):205-13. DOI: 10.1055/s-0036-1581114.
- Sconfienza LM, Albano D, Allen G, Bazzocchi A, Bignotti B, Chianca V, et al. Clinical indications for musculoskeletal ultrasound updated in 2017 by European Society of Musculoskeletal Radiology (ESSR) consensus. Eur Radiol. 2018;28(12):5338-51. DOI: 10.1007/s00330-018-5474-3.
- Albright RH, Brooks BM, Chingre M, Klein EE, Weil LS, Fleischer AE. Diagnostic accuracy of magnetic resonance imaging (MRI) versus dynamic ultrasound for plantar plate injuries: A systematic review and meta-analysis. Eur J Radiol. 2022;152:110315. DOI: 10.1016/j.ejrad.2022.110315.
- Dinoá V, von Ranke F, Costa F, Marchiori E. Evaluation of lesser metatarsophalangeal joint plantar plate tears with contrast-enhanced and fat-suppressed MRI. Skeletal Radiol. 2016;45(5):635-44. DOI: 10.1007/s00256-016-2349-z.
- Hulstaert T, Shahabpour M, Provyn S, Lenchik L, Simons P, Vanheste R, et al. Forefoot Pain in the Lesser Toes: Anatomical Considerations and Magnetic Resonance Imaging Findings. Can Assoc Radiol J. 2019;70(4):408-15. DOI: 10.1016/j.carj.2019.06.010.
- Mann TS, Nery CA de S, Baumfeld D, Fernandes E de Á. Degenerative injuries of the metatarsophalangeal plantar plate on magnetic resonance imaging: a new perspective. Einstein (Sao Paulo). 2022;20:eAO6543. DOI: 10.31744/einstein_journal/2022AO6543.
- Reijnierse M, Griffith JF. High-resolution ultrasound and MRI in the evaluation of the forefoot and midfoot. J Ultrason. 2023;23(95):249-69. DOI: 10.15557/JoU.2023.0033.
- McCarthy CL, Thompson G V. Ultrasound findings of plantar plate tears of the lesser metatarsophalangeal joints. Skelet Radiol. 2021;50(8):1513-25. DOI: 10.1007/s00256-020-03708-1.
- Carlson RM, Dux K, Stuck RM. Ultrasound Imaging for Diagnosis of Plantar Plate Ruptures of the Lesser Metatarsophalangeal Joints: A Retrospective Case Series. J Foot Ankle Surg. 2013;52(6):786-8. DOI: 10.1053/j.jfas.2013.05.009.
- Stone M, Eyler W, Rhodenizer J, Van Holsbeeck M. Accuracy of sonography in plantar plate tears in cadavers. J Ultrasound Med. 2017;36(7):1355-61. DOI: 10.7863/ultra.16.06067.
- Yamada AF, Crema MD, Nery C, Baumfeld D, Mann TS, Skaf AY, et al. Second and third metatarsophalangeal plantar plate tears: Diagnostic performance of direct and indirect MRI features using surgical findings as the reference standard. Am J Roentgen. 2017;209(2):W100-8. DOI: 10.2214/AJR.16.17276.
- Feuerstein CA, Weil L, Weil LS, Klein EE, Fleischer A, Argerakis NG. Static Versus Dynamic Musculoskeletal Ultrasound for Detection of Plantar Plate Pathology. Foot Ankle Spec. 2014;7(4):259-65. DOI: 10.1177/1938640014537300.
- Donegan RJ, Stauffer A, Heaslet M, Poliskie M. Comparing Magnetic Resonance Imaging and High-Resolution Dynamic Ultrasonography for Diagnosis of Plantar Plate Pathology: A Case Series. J Foot Ankle Surg. 2017;56(2):371-4. DOI: 10.1053/j.jfas.2016.11.009.
- Hodes A, Umans H. Metatarsalgia. Radiol Clinics. 2018;56(6):877-92. DOI: 10.1016/j.rcl.2018.06.004.