
doi.org/10.20986/revesppod.2025.1731/2025
REVIEW
Consequences of juvenile dermatomyositis at the podiatric level: a literature review
Consecuencias de la dermatomiositis juvenil a nivel podológico. Revisión bibliográfica
Elena Contreras Barragán1
Rocío de Paz Picornell2
Rafael Rayo Martín3
Ana María Rayo Pérez3
1Clínica Cuidados. Huelva, España.
2Dispositivo de Cuidados Críticos. Distrito Huelva-Costa. Huelva, España.
3Universidad de Sevilla, Spain.
Abstract
Background: Juvenile dermatomyositis (JDM) is a rare inflammatory disease that affects the muscles and skin, leading to significant complications in the musculoskeletal system and gait. At the podiatric level, JDM can cause functional impairments such as muscle weakness, calcinosis, and structural deformities, all of which impact the quality of life in pediatric patients. Understanding these consequences is essential for comprehensive and multidisciplinary management. The main objetive of the present paper is to explore and describe podiatric and gait-related alterations in pediatric patients with JDM, emphasizing the functional and biomechanical complications associated with the disease.
Methodology: A narrative literature review was conducted using electronic databases including PubMed, Scopus, Web of Science, Cochrane Library, and Google Scholar. The review included original articles, systematic reviews, clinical case reports, clinical guidelines, and specialized literature published in the last 20 years, in both English and Spanish.
Results: JDM is associated with intrinsic foot muscle weakness, subcutaneous calcinosis, and joint contractures, contributing to biomechanical alterations and inefficient gait patterns. Podiatric complications include pain, digital deformities, and equinus foot. These conditions affect mobility and may lead to chronic disabilities if not properly addressed. Early and multidisciplinary management can prevent permanent deformities and improve functionality.
Conclusion: JDM has significant podiatric implications that affect gait and the quality of life in pediatric patients. A comprehensive approach, including early diagnosis, targeted podiatric interventions, and multidisciplinary care, is essential to minimize complications and optimize functional outcomes.
Keywords: Juvenile dermatomyositis, podiatry, gait, biomechanical alterations, dermal alterations
Resumen
Antecedentes: La dermatomiositis juvenil (DMJ) es una enfermedad inflamatoria rara que afecta músculos y piel, con complicaciones significativas en el sistema musculoesquelético y la marcha. A nivel podológico, la DMJ puede generar alteraciones funcionales como debilidad muscular, calcinosis, y deformidades estructurales, que impactan la calidad de vida de los pacientes pediátricos. Comprender estas consecuencias es esencial para un manejo integral y multidisciplinario. El objetivo del presente trabajo consiste en explorar y describir las alteraciones podológicas y de la marcha en pacientes pediátricos con DMJ, destacando las complicaciones funcionales y biomecánicas asociadas a la enfermedad.
Metodología: Se realizó una revisión narrativa de la literatura utilizando bases de datos electrónicas como PubMed, Scopus, Web of Science, Cochrane Library y Google Scholar. Se incluyeron artículos originales, revisiones sistemáticas, casos clínicos, guías clínicas y literatura especializada publicada en los últimos 20 años, en inglés y español.
Resultados: La DMJ se asocia con debilidad muscular intrínseca del pie, calcinosis subcutánea y contracturas articulares, lo que contribuye a alteraciones biomecánicas y un patrón de marcha ineficiente. Las complicaciones podológicas incluyen dolor, deformidades digitales y pie equino. Estas alteraciones impactan la movilidad y pueden derivar en discapacidades crónicas si no se intervienen adecuadamente. El manejo temprano y multidisciplinario puede prevenir deformidades permanentes y mejorar la funcionalidad.
Conclusión: La DMJ tiene implicaciones podológicas significativas que afectan la marcha y la calidad de vida de los pacientes pediátricos. Un enfoque integral, que incluya diagnóstico temprano, intervenciones podológicas específicas y atención multidisciplinaria, es fundamental para minimizar las complicaciones y optimizar los resultados funcionales.
Palabras clave: Dermatomiositis juvenil, podología, marcha, alteraciones biomecánicas, alteraciones dérmicas
Corresponding autor
Elena Contreras Barragán
elena.con.bar@gmail.com
Received: 03-13-2025
Accepted: 07-02-2025
Introduction
Juvenile dermatomyositis (JDM) is a rare autoimmune inflammatory disease that primarily affects children and is characterized by a combination of proximal muscle weakness and distinctive cutaneous eruptions. It lies within the spectrum of idiopathic inflammatory myopathies, with a multifactorial pathogenesis involving interactions among genetic predisposition, environmental factors, and immunologic dysregulation(1). Although JDM shares some clinical features with adult dermatomyositis, it has peculiarities in presentation, course, and complications, with particularly important musculoskeletal—and thus podiatric and biomechanical—impact(1,2)
JDM is defined as an autoimmune inflammatory myopathy with chronic inflammation of striated muscle and a vasculopathy affecting small vessels in the skin, muscle, and internal organs². Its precise etiology remains undetermined, although a combination of genetic predisposition—notably HLA-associated alleles—and environmental influences such as viral infections and ultraviolet exposure has been proposed as triggers of autoimmune activation(3,5).
Predisposing factors include a family history of autoimmune disease, recurrent infections, and prolonged sun exposure. Increased susceptibility has been observed in girls, with a 2:1 female-to-male ratio(4). In specific populations with particular genetic variants, a higher risk of more severe manifestations and multisystem complications has been documented(4).
JDM has an incidence rate of cases per million children per year and is most common between ages 5 and 15, although cases have been reported in infants and preschoolers. It is the most frequent inflammatory myopathy in pediatrics(1,4). Clinical course is variable: a minority achieve complete resolution, whereas others develop chronic complications such as calcinosis or permanent joint contractures(6).
The clinical picture includes symmetric weakness that may present as difficulty climbing stairs or rising from a seated position. Cutaneous findings are characteristic, including heliotrope erythema of the eyelids and Gottron papules over extensor surfaces. Systemic complications such as subcutaneous calcinosis and vasculopathy are common in severe or prolonged disease(5,6,7).
Diagnosis is based on a combination of clinical findings and imaging. Laboratory tests frequently show elevated muscle enzymes (eg, creatine kinase and aldolase) and disease-specific autoantibodies (eg, anti-MDA5 and anti-NXP2). MRI is useful to identify muscle inflammation, and muscle biopsy confirms the diagnosis in uncertain cases(4,5,6).
JDM can cause significant musculoskeletal complications. Weakness of intrinsic foot muscles, together with biomechanical alterations, contributes to an inefficient, high–energy-cost gait pattern?. One of the most frequent complications—subcutaneous calcinosis—causes severe pain and joint stiffness, further limiting mobility and function. Chronic inflammation may lead to joint contractures, digital deformities, and equinus foot, worsening functional impact(7,8).
Recent studies have described distinctive dermatologic findings on the feet of patients with JDM, termed “hiker’s feet” (Figure 1), with diffuse erythema and inflammation in areas of greatest pressure, often with scaling?.

Figure 1. Juvenile dermatomyositis in an adult patient showing “hiker’s feet” lesions on the plantar forefoot.
The podiatric prognosis in JDM is closely related to disease severity, treatment efficacy, and complications such as calcinosis or contractures. In mild cases, early, multidisciplinary management can prevent permanent deformity and substantially improve quality of life. In more severe cases, biomechanical alterations and progressive calcinosis may result in chronic disability(7,8,9).
The general objective was to explore and describe in detail podiatric and gait alterations in pediatric patients with JDM, analyzing functional, biomechanical, and clinical impact to improve comprehensive podiatric care. Specific endpoints were to identify and characterize foot musculoskeletal alterations (eg, flexible flatfoot, equinus, joint contractures, digital deformities); describe pathologic gait patterns related to proximal weakness, pain, calcinosis, and other biomechanical changes; analyze foot-specific cutaneous manifestations (eg, “hiker’s feet”) and nail conditions (eg, trachyonychia) as clinically relevant signs for podiatric diagnosis and follow-up; explore functional and energy impact on autonomy, mobility, and quality of life; review and systematize podiatric interventions in the literature (eg, custom orthoses, physical therapy, orthoses, footwear adaptations) within a multidisciplinary approach; and propose evidence-based clinical recommendations for comprehensive podiatric management.
Materials and methods
Study design
This narrative review identified, analyzed, and synthesized relevant literature on podiatric consequences and gait alterations in pediatric JDM. Sources were retrieved from PubMed, Scopus, Web of Science, Cochrane Library, and Google Scholar.
The research question—“What are the podiatric and gait consequences in pediatric patients with JDM?”—guided selection and synthesis to provide an integrated, updated view of podiatric impact.
Inclusion and exclusion criteria
We included studies describing podiatric, biomechanical, or gait manifestations in JDM, as well as articles analyzing musculoskeletal involvement in pediatric autoimmune disease. Only Spanish or English publications were considered.
On the other hand, excluded studies focused exclusively on adults; studies without full-text access or with insufficiently detailed abstracts; and JDM studies lacking specific podiatric/biomechanical information.
Search and selection protocol
Database-specific strategies were applied using terms such as: “Juvenile dermatomyositis” AND “gait abnormalities,” “Juvenile dermatomyositis” AND “foot complications,” and “Pediatric autoimmune diseases” AND “gait” AND “pediatric motor skills.”
The search strategy was: (Juvenile dermatomyositis) AND ((gait abnormalities OR gait) OR (foot complications) OR (pediatric motor skills)).
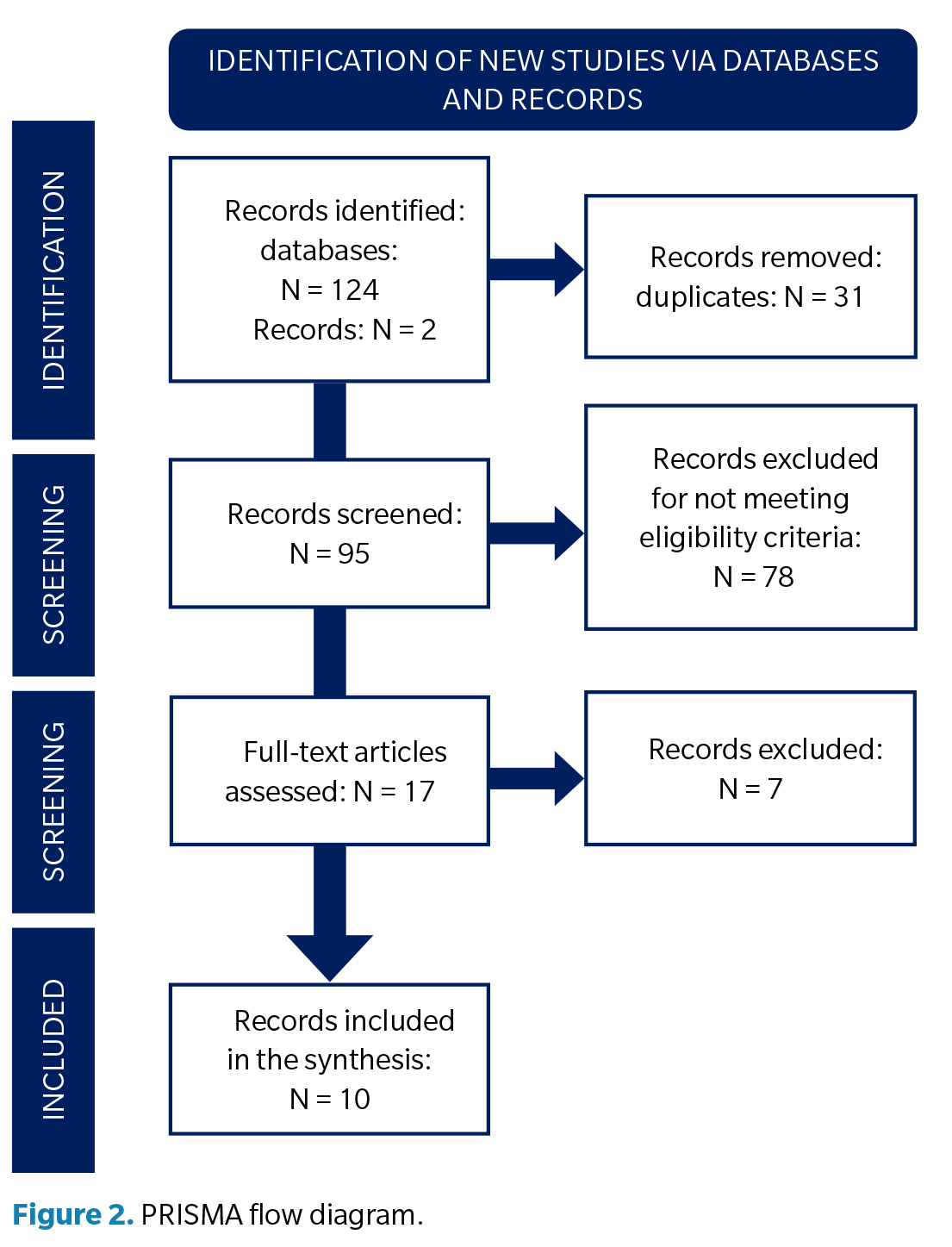
Titles/abstracts were screened for relevance and duplicates removed. Full texts of selected articles were reviewed against predefined criteria.
Relevant data were organized in a matrix capturing podiatric manifestations, gait impact, and relation to the analyzed case. Patterns and divergences were synthesized coherently.
Analysis and synthesis
Podiatric and gait consequences were categorized by etiology, severity, and relation to JDM, and clinical implications were discussed in a podiatric context. Risk of bias and methodologic quality were assessed qualitatively.
Results
Among 17 selected articles, diverse findings related to podiatric and gait consequences in JDM were identified, though the literature is limited. Most studies (n = 10) (Table 1) reported general musculoskeletal complications; of these, only a few (n = 5) specifically addressed podiatric or biomechanical gait manifestations.
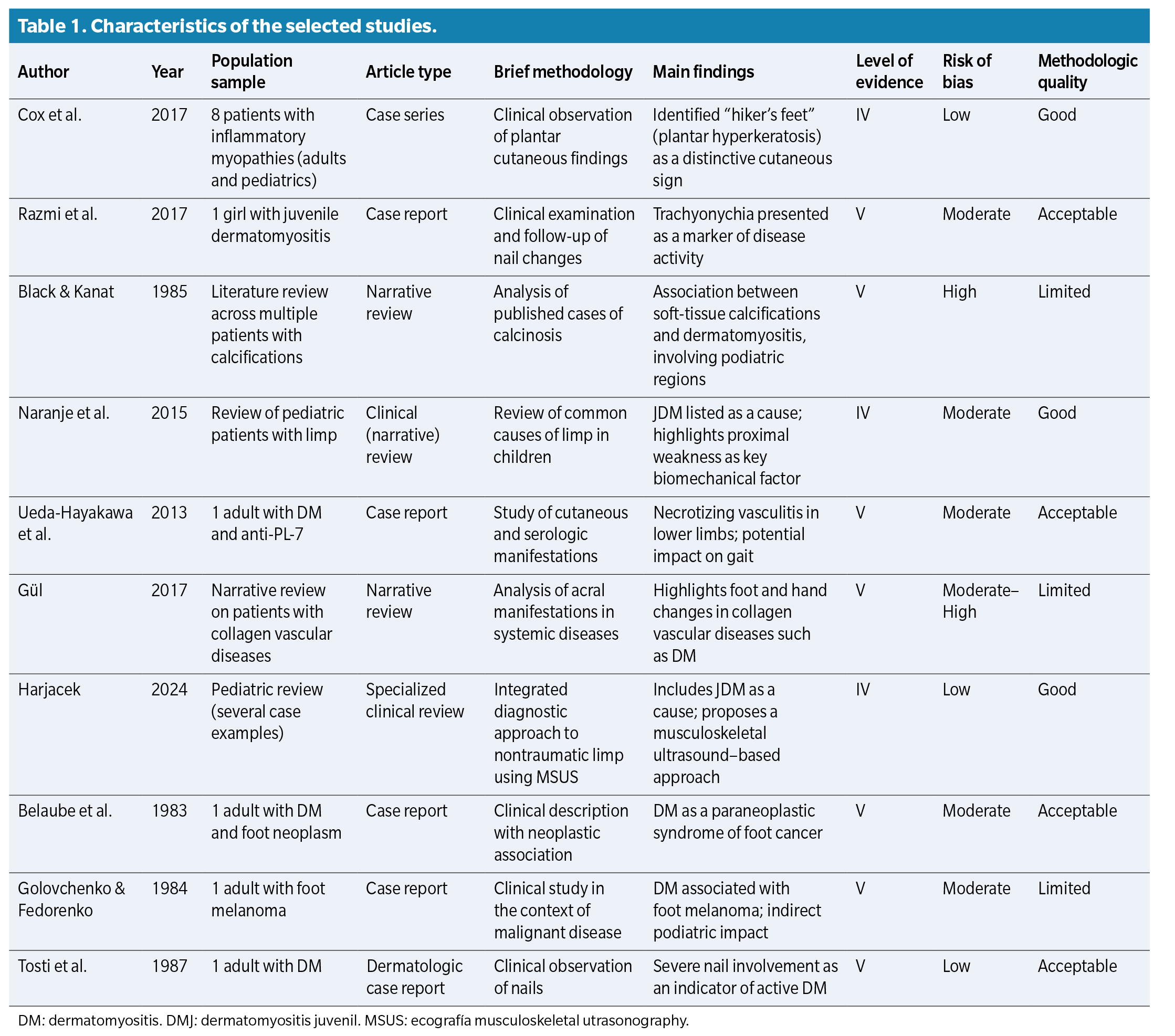
Applying inclusion/exclusion criteria (Figure 2) yielded 10 relevant studies addressing podiatric, musculoskeletal, and biomechanical manifestations in JDM. Most were case reports (n = 5), followed by narrative/clinical reviews (n = 4) and one case series (n = 1). No controlled trials or analytic observational studies (eg, cohorts or case-control) specifically focusing on podiatric or gait manifestations in JDM were identified.
Study type and level of evidence
By Oxford levels, case reports/series represent level V evidence, and clinical/narrative reviews are level IV, lacking statistical analysis and variable control. None reached levels I–III, limiting causal inference and generalizability.
Methodologic quality
Quality was assessed qualitatively (clarity of description, coherence between aims and results, clinical relevance). A total of 40 % were of acceptable quality, 30 % good, and 30 % had significant limitations (eg, limited clinical context, ambiguous methods, low applicability).
The higher-quality studies were Cox et al. (2017), a well-documented case series on plantar cutaneous findings (“hiker’s feet”), and Harjacek (2024), who proposed an integrated diagnostic approach to pediatric limp—including JDM—with musculoskeletal ultrasound; both were rated good quality with low risk of bias.
Risk of bias
Risk was low in three studies (30 %), moderate in five (50 %), and high in two (20 %). Low-risk studies provided clear clinical descriptions, adequate follow-up, and consistent interpretation; moderate/high-risk studies lacked variable control and methodological detail or showed potential selection/publication bias typical of nonsystematic reviews and isolated reports.
Main findings
Overall, JDM can produce a wide range of musculoskeletal and podiatric manifestations directly affecting gait and biomechanics in children. Frequently reported alterations included:
Despite these findings, there is a notable scarcity of studies focused specifically on podiatric and biomechanical repercussions of JDM; most address general/systemic complications, with few analyzing functional gait or whole-body mechanics in children with this condition.
Discussion
JDM is a rare autoimmune disease characterized by muscle inflammation and cutaneous lesions, with clinical manifestations across multiple systems, including musculoskeletal and skin. In podiatry, management is critical due to implications for foot function, mobility, and quality of life. This analysis addresses podiatric implications based on findings from multiple studies on JDM.
Cox et al.(9) described “hiker’s feet,” characterized by erythema and scaling of the feet in inflammatory myopathies such as JDM, underscoring the value of careful podiatric evaluation because these lesions may precede other symptoms and serve as early diagnostic markers.
Razmi et al.(10) highlighted nails as potential indicators of disease activity; trachyonychia—rough, brittle nails—may signal active systemic inflammation, supporting routine nail assessment in podiatric evaluation. Musculoskeletal signs such as weakness and dystrophic calcifications have direct implications for foot function. Black and Kanat(11) reviewed soft-tissue calcifications, which can occur in the foot and restrict mobility; in children, they may alter arch development and gait. Naranje et al. (12) addressed limp as a common pediatric presentation in inflammatory conditions. In JDM, proximal weakness combined with inflammation and pain may lead to gait alterations requiring podiatric interventions such as custom orthoses or assistive devices.
Vascular complications are frequent and involve pedal tissues: Ueda-Hayakawa et al.7 reported necrotizing cutaneous vasculitis—including acral areas—predisposing to ulceration and requiring specialized care to prevent infection and improve healing. Gül et al.13 noted acral signs (eg, edema and erythema) in collagen vascular diseases; in JDM, these may mimic other conditions, reinforcing the need for careful podiatric diagnosis.
While immunosuppressants and physical therapy are central to treatment, podiatric management is essential for quality of life. Harjacek et al. (14) emphasized the utility of musculoskeletal ultrasound for soft-tissue assessment in children with JDM—useful to monitor inflammation and guide noninvasive interventions.
Foot calcifications may require specific approaches, including footwear adaptations and off-loading. Belaube et al. (15) and Golovchenko et al. (16) documented JDM cases with malignant lesions involving the feet, highlighting the importance of podiatric evaluation within multidisciplinary care.
JDM significantly affects children’s quality of life because of its functional and cosmetic impact. Podiatric assessment focuses not only on function but also on appearance and comfort, aspects that are crucial to the psychological well-being of pediatric patients. Tosti et al. (17) documented the psychological impact of severe nail disorders, underscoring the importance of addressing these concerns in the clinical setting.
Limitations
This review provides an overview of podiatric, musculoskeletal, and biomechanical manifestations in pediatric JDM but has important limitations. First, specific and up-to-date literature on this topic is scarce. Most included studies are case reports or narrative reviews with low levels of evidence (Oxford level IV–V), limiting causal inference and generalizability. No clinical trials or observational studies with representative samples directly assessing podiatric function or gait in this population were identified.
Second, methodologic heterogeneity was substantial. Variability in clinical approaches, lack of standardized tools to measure biomechanical alterations, and nonuniform diagnostic/follow-up criteria hinder comparisons. Risk of moderate or high bias was present in a considerable proportion of studies, particularly those lacking clear methodology or prone to publication bias. Finally, analysis was limited to English and Spanish publications, potentially excluding relevant evidence in other languages.
Conclusions
JDM exhibits a characteristic pattern of musculoskeletal involvement with major podiatric repercussions, notably proximal weakness, chronic inflammation, and vascular alterations that affect foot biomechanics and gait, compromising autonomy and quality of life. Common alterations include flexible flatfoot, mild equinus, and digital deformities from joint contractures, limiting ankle and forefoot mobility. Weakness of intrinsic and proximal muscles produces an inefficient gait with claudication, slowness, higher energy expenditure, and postural compensation. Cutaneous signs such as “hiker’s feet” cause pain, hyperkeratosis, and mechanical overload, while chronic complications such as subcutaneous calcinosis produce pain, stiffness, and functional limitation requiring targeted orthopaedic interventions. Podiatric care should be early, preventive, and multidisciplinary, with periodic gait and postural assessments using biomechanical tools. There is a marked lack of podiatry- and gait-focused studies in children with JDM, underscoring the need for research on podiatric consequences and the effectiveness of therapeutic interventions.
Conflict of interest
None
Funding
None
Contributions of the authors
Conception and design: ECB
Data collection: RPP
Analysis and interpretation of results: ECB, RRM
Creation, writing and preparation of the draft: RRM
Final review: ECB, AMRP
Ethics declaration
This study analyzed existing literature only and did not involve human subjects or require ethics approval
References