DOI: http://dx.doi.org/10.20986/revesppod.2024.1692/2024
ORIGINAL
Ultrasound-detected ankle tenosynovitis is associated with foot function disorders: a cross-sectional study
La tenosinovitis ecográfica de tobillo está asociada a la alteración funcional del pie: un estudio transversal
Anna Tribó Crespo1
César Díaz Torné2
Patricia Moya Alvarado2
Francesc Monés Serrano3
1Dpto. de Biomecànica. Centre Podològic Monés. Badalona, Barcelona, España
2Servei de Reumatologia. Hospital de la Santa Creu y Sant Pau. Barcelona, Barcelona
3Servei d’Endocrinologia i Nutrició. Hospital Germans Trias i Pujol. Badalona, Barcelona, España
Abstract
Introduction: This study aims to explore the association of static and dynamic foot disorders with ankle tendinopathy measured by ultrasound, more specifically of tibialis posterior tendon and peroneal ankle tendons, in healthy subjects.
Patients and methods: A cross-sectional descriptive and analytical study was designed and carried out in Rheumatology Unit, Hospital de la Santa Creu i Sant Pau, Barcelona. For each participant were registered: age, sex, Foot Posture Index (FPI-6), Foot Kinetic Index (FKI) and tibialis posterior and peroneals tendons ultrasound patological features. Logistic regression was used to evaluate the likelihood that postural or/and functional foot disorders is related to ankle sonographic features.
Results: Association between ultrasound tenosynovitis features and dynamic disorder resulted statistically significant (p = 0.00). Association between ultrasound affection and simultaneous, static and dynamic, foot disorders was also statistically significant (p = 0.03). Dynamic’s overpronation is associated to tibialis posterior tendon tenosynovitis (p = 0.012). Dynamic disorders were associated with the likelihood of ankle tendinopathy in unadjusted models (OR = 5.9).
Conclusions: This cross-sectional study reports association between foot function disorders and ankle sonographic features. It FKI highlights as a diagnostic score able to detect risk factors for inflammatory ankle pathology.
Keywords: Kinetic assessment, plantar pressures, gait analysis, tendinopathy, ankle tenosynovitis, foot ultrasound
Resumen
Introducción: Este estudio tiene como objetivo explorar la asociación de los trastornos estáticos y dinámicos del pie con la tendinopatía ecográfica del tobillo, más específicamente del tendón del tibial posterior y los tendones peroneos del tobillo, en sujetos sanos.
Pacientes y métodos: Se diseñó un estudio descriptivo, analítico, transversal que se llevó a cabo en la Unidad de Reumatología del Hospital de la Santa Creu i Sant Pau, Barcelona. Se registró la edad, sexo, índice de postura del pie (FPI-6), índice cinético del pie (FKI) y la característica patológica ecográfica, del tendón del tibial posterior y de los tendones peroneos. Se utilizó la regresión logística para evaluar la probabilidad de que los trastornos posturales y/o funcionales del pie estén relacionados con los hallazgos ecográficos de patología.
Resultados: La asociación entre las características ecográficas de tenosinovitis y el trastorno dinámico resultó estadísticamente significativa (p = 0.00). La asociación entre la afección ecográfica y los trastornos simultáneos, estáticos y dinámicos, del pie también fue estadísticamente significativa (p = 0.03). La hiperpronación dinámica se asocia a la tenosinovitis del tendón tibial posterior (p = 0.012). Se realizó un análisis complementario, de carácter exploratorio, para valorar la probabilidad de asociación entre trastorno dinámico y tendinopatía de tobillo que mostró un odds ratio de 5.9.
Conclusiones: Este estudio transversal informa sobre la asociación entre trastornos de la función del pie y características ecográficas de tobillo. El FKI destaca como diagnóstico numérico capaz de detectar factores de riesgo de patología inflamatoria del tobillo.
Palabras clave: Análisis cinético, presión plantar, estudio de la marcha, tendinopatía, tenosinovitis de tobillo, ecografía de pie
Correspondence: Anna Tribó Crespo
annatribo00@gmail.com
Received: 11/03/2024
Acepted: 10/04/2024
Introduction
The tissue stress theory explains that prior to an injury, fracture, of any tissue, organic or not, subjected to a certain effort, it will undergo a series of reversible changes within the area of elastic deformity, or irreversible if it is found already within its area of plastic deformity, still eliminating stress or suffering(1). These changes, within anatomical tissues, such as muscles or tendons(2), are progressively; hypertrophy, inflammation (with increased interstitial fluid, visualized specifically for tendons inside the pods), heterogeneity of fibbers and finally partial or complete rupture. All these changes are observable by ultrasound examination, which require a large learning curve for the evaluator, but it is a validated diagnostic method. It seems logical that to prevent injuries we must identify the effort or stress of the structure to be able to reverse it(3).
Specifically, if we evaluate diseases of ankle’s stabilizing muscles and tendons, we must be able to use systems for detecting its over-strengthening suffering. Visual exploration of patient’s posture provides information for static evaluation, without movement, but not for information during walking, because the executed movements are performed at a frequency higher than that which the human eye is able to detect. Biomechanical ankle and foot assessment systems can be kinematic(4) (with high frequency camera with 3D data extraction) or kinetics (based on force or pressure records using elements such as dynamometric or pressure sensor platforms). For static subject’s assessment only the Foot Posture Index (FPI-6) has been validated. For dynamical assessment different variables have been used, both in kinetic and kinematic exploration but no consensus or validity of any diagnostic method or value has been reached. Emphasize that economic cost required by a kinematic scanning lab, (high-frequency external cameras and distribution for 3D reconstruction) is higher than that is required by kinetic scanning, (pressure platforms or sensor insoles).
Biomechanical disorders, both static and dynamic, seem to be responsible for the stress of tissues on ankle stabilizing muscles(5). Our aim was to know how often that is quantitatively real. So, our outcome was to assess association between pathological gait and stress tissue on ankle. It was necessary to choose a postural assessment value and a dynamic assessment variable, both able to detect disorders, aim to relate them to the possible inflammatory disease.
It is necessary to know the importance of certain factors in relation to the appearance or not of a certain disease in order to decide whether to study them, in future projects, as possible risk factors. The fact of not having found bibliographic references on relationship between these three observations in particular (posture disorder, dynamic disorder and tendinous affection), led us to design a descriptive and analytical observational study, with exploratory nature.
The general outcome of the study was to explore the association of foot dynamic and static disorders with ankle’s tendinopathy, specifically of the tibialis posterior tendon and the peroneal tendons. As specific objectives, we tried to describe the frequency of the postural disorder variable, for its three possible categories: pronated, supinated and neutral, as well as the frequency of the dynamic disorder variable, for its three possible categories: pronated, supinated and neutral, and also describe the frequency of inflammatory disease variables, by ultrasound examination of the tibialis posterior tendon and peroneal tendons. Then we tried to determine statistical association, strength and relative risk, between the three possible variables and their different possible categories.
Patients and methods
This is a cross-sectional descriptive and analytical study. Dataset were collected between the months of January and August 2017, in the city of Barcelona, Spain. Participants in the study were recruited from among students, professionals, partners and familiars next to “Hospital de Sant Pau i la Santa Creu” from Barcelona. Participants were recruited according to the following selection criteria: being over 18 years old, having no clinical symptoms, absence of medical history for osteoarticular diseases, traumatic or surgical history of foot and ankle. Participants using foot insoles treatment during the last year(6), were excluded.
Fifty-five participants were analysed. Total sample size results n = 104 valid feet. Each foot was evaluated independently, even though it belonged to the same participant(7).
Sample size was determined in a non-probabilistic way, for convenience for exploratory purposes. Highlight that sample size has sufficient statistical power to answer the objectives.
That study was carried out in accordance with recommendations contained in the “Statement for Improving the Reporting of Observational Studies in Epidemiology”, STROBE, Strengthening the Reporting of OBservational studies in Epidemiology.
Tools and procedures
Any man or woman over 18 years of age, without symptoms in the lower limb, who had some relationship with the Rheumatology Department was candidate for the study. In a single visit, for each participant, the following data were collected: demographic characteristics, age, weight, height and medical or podiatric treatments, postural assessment, dynamic assessment and ankle’s ultrasound examination.
Postural assessment
For evaluation of foot postural disorders, each participant was examined in static standing and the Foot Posture Index-6 (FPI-6) )(8,9)value was determined for each foot. This interview and first evaluation were always carried out by the same examiner, a podiatrist with more than two years of clinical experience, who filled in a data collection sheet. The collection was blinded of the clinical data, of the dynamic study (FKI) and of the ultrasound examination.
Foot Posture Index-6 is a validated static foot posture assessment index for the quantitative determination of the patient’s posture, by observing and consequently scoring 6 criteria. FPI-6 considers forefoot, hind foot and midfoot in the three anatomical planes. The scoring system used is the 5 points of the Likert-type scale (from +2 to -2) where the maximum positive score will be awarded to the criteria of greater pronation and the maximum negative values to those of greater supination. The FPI is therefore obtained as add up of scores (-2, -1, 0, 1 or 2) given to each of the six criteria. According to the results it is categorized as neutral foot (from 0 to 5), pronated foot (from 6 to 9), highly pronated (from 10 to 12), supinated foot (from -1 to -4) and highly supinated foot (from -5 to -12).
Dynamic assessment
For dynamic disorders evaluation, Foot Kinetic Index (FKI) was used. For this, each participant was walking barefoot at a comfortable speed. Subject could walk free in a straight line, in which platform thickness did not interfere, in both directions, for approximately 6 meters, and minimum 5 repetitions, in a comfortable and lightly room. Dynamic participant’s pressures during gait analysis were recorded using a 49 X 49 cm mat of capacitive sensors (AmCube, Gargas, France). Centre of Pressures trajectory (Cop) )(10,11,12)and Maximum Pressure points line were evaluated using the FootWorkPro software, by AMCube. Several steps were recorded for each foot, but only the three most representative steps were saved. From these Foot Kinetic Index (FKI) value was obtained. Process of record and score the different items to obtain the FKI was always carried out by the same and evaluator, a podiatrist with more than fifteen years of clinical experience, and was blinded of clinical data, of posture study (FPI-6) and of ultrasound assessment.
Foot Kinetic Index (FKI) is a quantitative index to assess dynamic foot function, based on comparison of Centre of Pressure trajectory (Cop) to Maximum Pressure path. The Foot Kinetic Index (FKI) is a clinical examination method, not validated, for the quantification of the dynamic foot functionality through observation and consequent scoring of rear foot, midfoot and forefoot respect the four gait phases; loading response, midstance, terminal stance and pre-swing. It is an index that allows to score the moments of force in the frontal plane, pronator and supinator, also taking into account their duration. FKI scoring system award maximum positive score to criteria of greater pronation and maximum negative values to those of greater supination. According to the results it is categorized as neutral foot (from -3 to 3), pronated foot (from 4 to 12) and supinated foot (from -4 to -12).
Tendinopathy Assessment
Regarding ankle ultrasound evaluation, a General Electric Logic 5 Pro ultrasound machine (GE HealthCare, California, USA) with a compact linear transducer of 10 MHz frequency was used)(13). For evaluation of tendinopathy, the echo-structure of the tendon was observed, classifying it as homogeneous or heterogeneous. It was also assessed whether or not there was rupture, if so, it was classified as partial or total. Finally it was described whether or not an increase in fluid was observed in tendon sheaths, considering the finding of up to 1.5mm of fluid in sheaths as normal, and identification of a width of fluid accumulation in sheaths greater than 1.5 mm as pathological, representative of inflammation. The presence of any of the above alterations was considered positive for the variable; “Ultrasound-detected tenosynovitis”. Ankle ultrasound examination was performed in all anatomical planes. Tibialis posterior tendon)(14) and the tendons of the peroneus longus and brevis muscles of the medial and lateral ankle compartments, respectively, were considered. Both the exploration, the evaluation and data recording were carried out by a rheumatologist sonographer with more than eight years of experience, and it was blinded to the clinical data, to the study of posture (FPI-6) and to kinetics dataset (FKI).
Variables of study
Primary outcome variables were categorical; Postural disorder existing or not, dynamic disorder existing or not, and inflammatory disease of Tibialis posterior and/or Peroneal tendons existing or not.
Secondary outcome variables were; patient’s age, as a continuous variable, and the foot classification, both static and dynamic, in pronated foot, supinator foot or neutral foot, thus resulting in three categories.
Statistical analysis
Excel database and the statistical package SPSS, 24.0®, (IBM®, USA) were used. Descriptive analysis of the variables, frequencies for the categorical and mode, median and standard deviation for the continuous one was performed. To analyse statistical association between ultrasound disease variable and static or dynamic disorders variables, the Chi-square test for contingency tables was used, the level of significance adopted was p > 0.05.
Logistic regressions was used to calculate the odds ratio (OR) and 95 % confidence interval (CI) for tendinopathy based on postural or/and dynamic foot disorders. It was calculated, with exploratory character, aimed to find statistical association strength and relative risk between the observations: static or dynamic alterations and ultrasound disease.
A binary logistic regression unadjusted was used to calculate Odds ratio between static or dynamic disorders or both (as exposure) and ultrasound disease (as outcome). From this was obtained the Odds Ratio (OR) as the risk of appearing or not posterior Tibialis and/or Peroneal tendinopathy depending on whether or not the participant presented static or dynamic disorders. For each binary logistic regression model, its goodness of fit and the confidence intervals were taken into account, and the calibration was verified using the Hosmer-Lemeshow test.
Results
We registered 104 feet from 52 participants. Women were 67.3 % of the sample. Mean age was 42.17 years, (19-88).
Frequency of appearance of ultrasound disease among the 104 feet studied was 45.2 % (47 feet). Thirty-five feet presented tibialis posterior ultrasound-detected tenosynovitis, 12 feet showed peroneals tendons ultrasound affection, and 10 feet simultaneous disease of both structures.
Frequency of postural disorder (FPI-6) within the sample was 51 % (53 feet), of these 41 feet had excessive static pronation and 12 feet had excessive static supination. Dynamic disorder (FKI), appeared in 69.2 % (72 feet), 57 feet in excessive dynamic pronation and 15 feet in excessive dynamic supination. Frequency of simultaneous postural and functional defect (of both indices: FKI and FPI-6) was also recorded, resulting in 33.7 % (35 feet from the 104 studied).
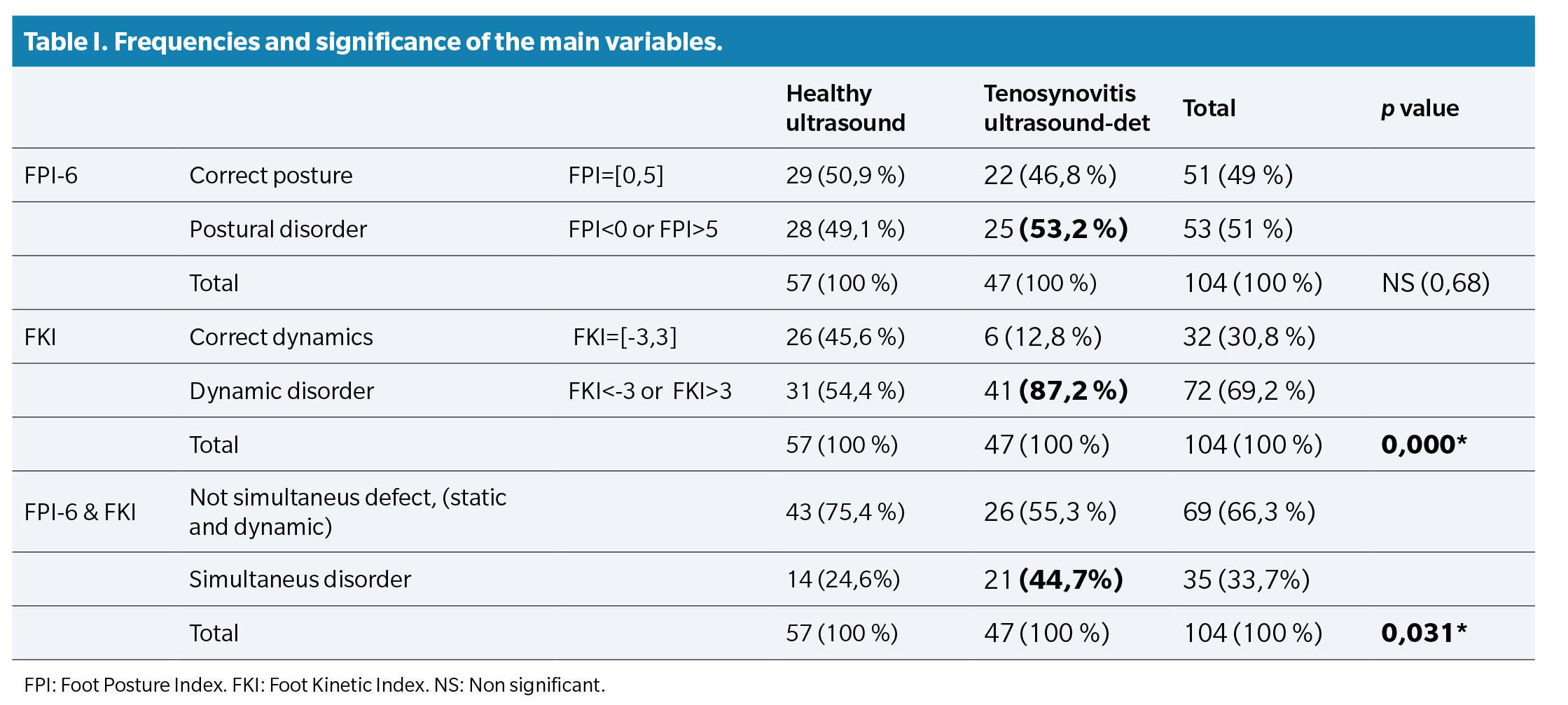
Regarding association between the three main variables to each other, trough contingency tables, association between dynamic disorder (FKI) and ultrasound-detected tenosynovitis appeared statistically significant (p = 0.000), finding that for 47 feet with ultrasound disease 41 feet (87.2 %) also presented dynamic disorder (FKI). (Table 1).
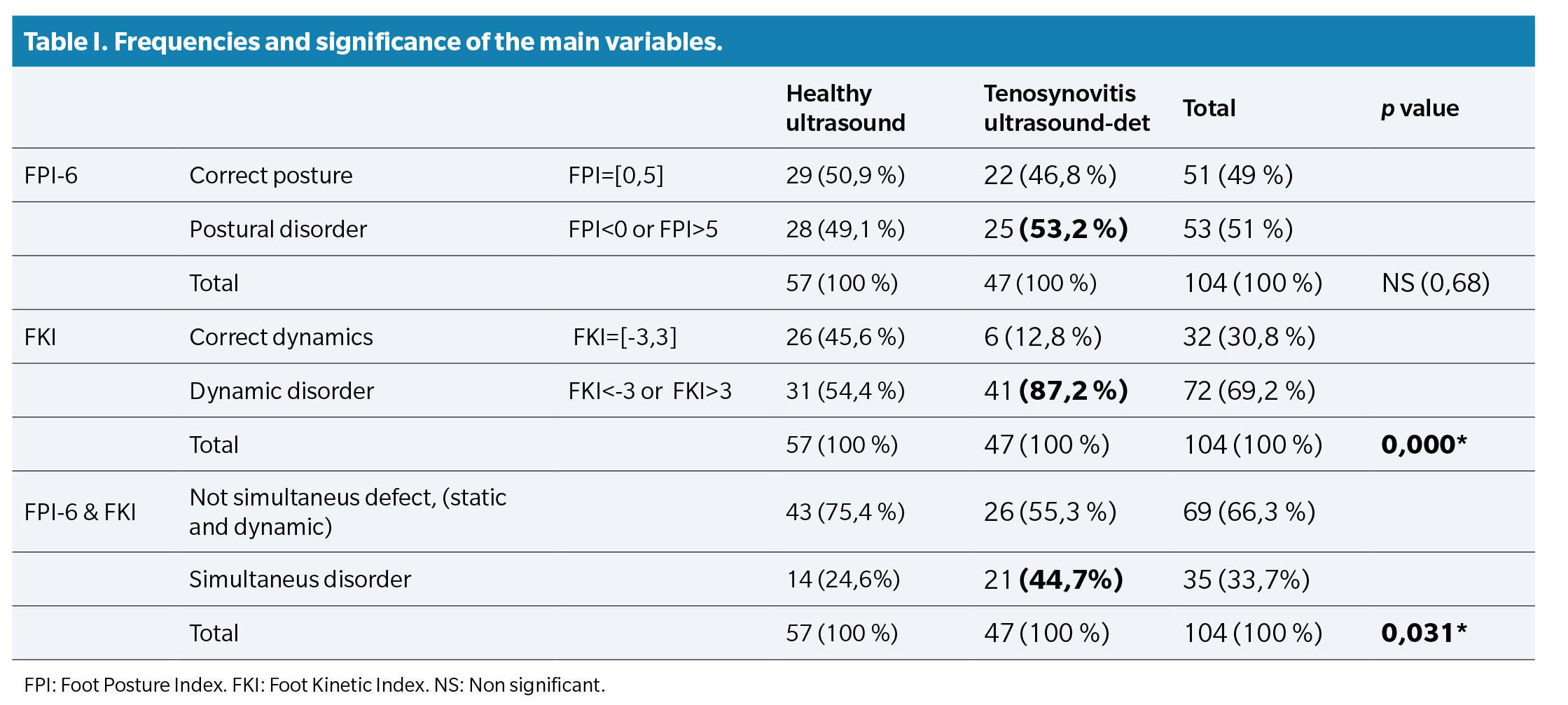
Association between static disorder and ultrasound disease was not statistically significant (p = 0.68), and showed that for the 47 feet with ultrasound disease only 25 feet (53.2 %) presented static disorder (FPI). There was not statistical significance (p = 0.89) in the association between static alteration and dynamic alteration of the foot.
Association between ultrasound disease and simultaneous disorder, both static and dynamic of the foot, was also analysed, and it was also statistically significant (p = 0.031). For 47 feet with ultrasound-detected tenosynovitis, 21 feet (44.7%) presented simultaneous disorder of FPI-6 and FKI (Table 1).
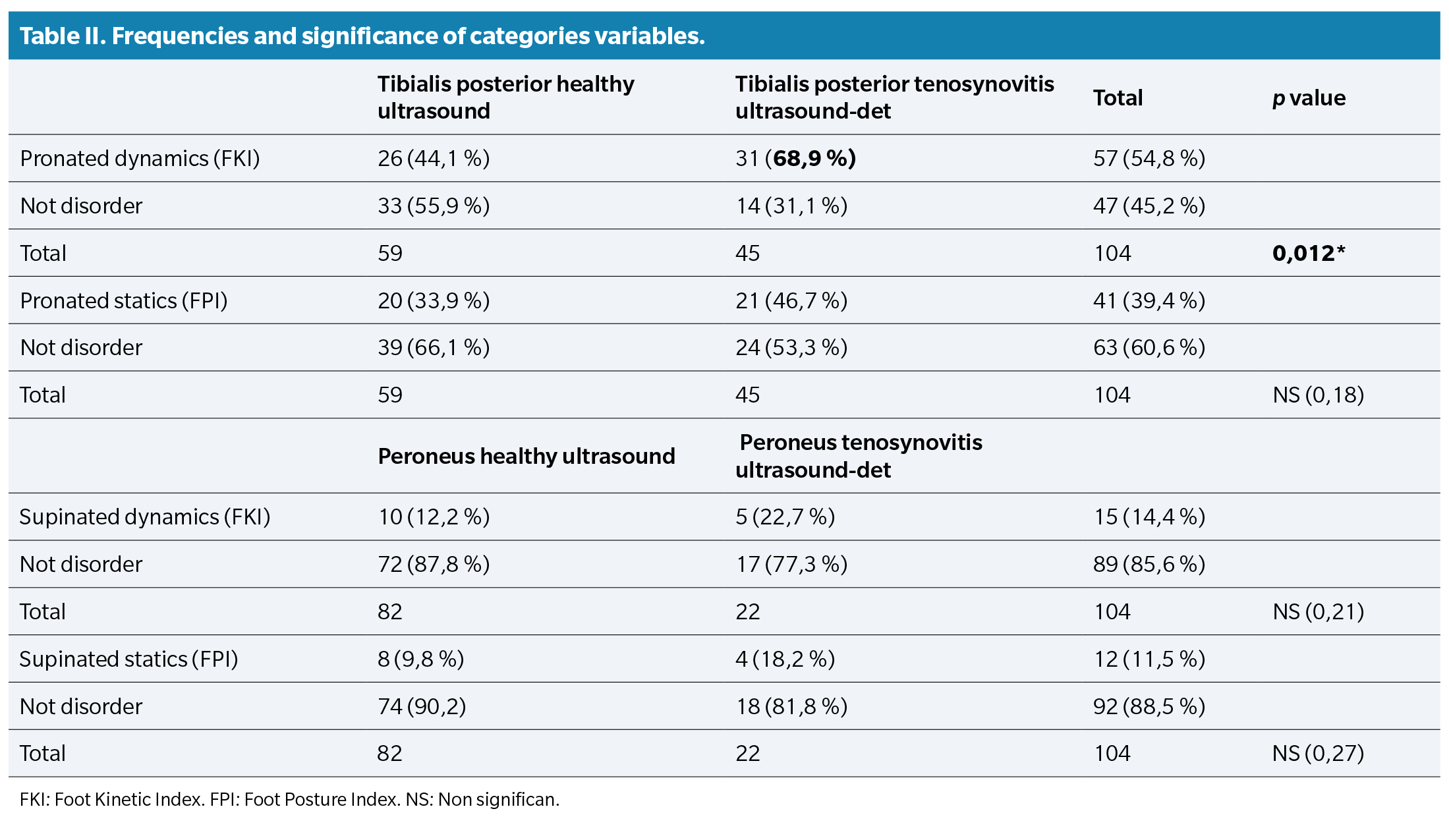
Association between tibialis posterior ultrasound-detected tenosynovitis and pronation disorder was studied. The same with the correspondence between peroneal tendons ultrasound affection and supination disorder. Results showed that only dynamic pronation complaint association to tibialis posterior ultrasound-detected tenosynovitis. (p = 0.012). Other associations were not statistically significant (Table 2).
Based on unadjusted binary logistic regression model there was a significant trend for higher likelihood of ankle tendinopathy across participants with pathological gait. The unadjusted odds of tendinopathy in dynamic alterations feet was OR = 5.9 (95 % CI 2.15-16.26) compared to correct gait feet. (p = 0.001). Other binary logistic regressions results, for static or both disorders respect to ultrasound disease, did not show significance.
Discussion
This study showed statistically association between dynamic disorders and ankle tendinopathy measured by ultrasound a finding consistent with our hypothesis. The 87.2 % of feet with dynamic disorders have ultrasound-detected tenosynovitis. And 44.7 % of feet with both, static and dynamic disorders, have ultrasound-detected tenosynovitis. But static disorders have not statistically association to ankle tendinopathy, a new biomechanical approach.
Feet with dynamic disorder could have more likelihood of tendinopathy from an ultrasound perspective. This might be the first report of dynamic disorders as risk factor of tendinopathy. Some authors have searched relationship between static and dynamic foot posture and running biomechanics, as Hollander’s review summarize(15), but there are not precedents for seeking to associate these two alterations, kinetic gait disease and ankle tendinopathy, in literature.
Our findings grant credibility to Foot Kinetic Index (FKI) to determine dynamic foot disorders, so it could be considered as an innovative measurement of gait. It will be necessary to develops new trials to asses sensitivity and specificity of Foot Kinetic Index (FKI) as a diagnostic method. Cop progressions and characteristics have been studied in literature before but it’s observation has not been shown to be able to diagnose dynamic disorders during walking(16).
Implications of our findings are important for several reasons. First, because it is necessary to have a quantifiable value of the dynamic alteration both in the field of the research and within clinical practice aimed at determining specific diagnoses. Foot Kinetic Index offers that. Second, clinical decision-making and treatment designs need to be focused on modifying dynamic alterations, results suggest it. Third, like dynamic alteration is a modifiable factor that could be a target for preventive strategies to attenuating tendinopathy complications, especially in fields like rheumatology, paediatric or sports medicine. To control risk factors improve health outcomes.
Our study is not without limitations. Ultrasound findings recorded in this study were asymptomatic, one of the criteria for inclusion of participants was no pain, no symptoms. Therefore we analysed a subclinical inflammatory stage that in the field of ultrasound diagnosis is already considered a pathological alteration despite not showing obvious clinical evidence. At the same, it is necessary to carry out a cohort study to confirm Odd Ratio results obtained (OR = 5.9 95 % CI: 2.15,16.26) in our work, designed with exploratory character, due to absence of bibliographic precedents. Moreover, the non-existence of a validated dynamic gait diagnostic method, such as a gold standard for comparisons with Foot kinetic Index, led us to design this work using the validated ultrasound diagnostic method as a system for comparing with and locating associations.
Our data reinforce several important new biomechanical approaches. First, there is not association between excessive static or dynamic supination and peroneals tendons disease, external ankle compartment. Second, there is not association between excessive static pronation and Posterior Tibialis tendon disease, internal ankle compartment, but there is association between excessive dynamic pronation with Tibialis posterior ultrasound disease. Third, the highest association (87.2 %, p = 0.000) is between dynamic disorder (in pronation, in supination or both) and ultrasound disease (for Tibialis posterior, for Peroneus tendons, or for both). Results suggest that ankle movements control in sagittal axis, pronation or supination, are not regulated by a single tendon muscle group, of the internal compartment or external compartment of the ankle, respectively, but that both are capable of stabilizing prone/supination defects. However, results show maybe the most responsible in that role is Tibialis posterior tendon because it seems to be who suffers the most stress or overstrain. Perhaps for this reason it is the target tendon of osteoarthritic disease lesions.
About limitations and research perspectives about the paper highlight that Foot Kinetic Index (FKI) is not a validated index. We were unable to find any validated assessment index or diagnostic system for dynamic disorders in scientific literature. There are pathological classification criteria depending on the ranges of joint mobility recorded by high-frequency video cameras, including the construction of 3D models for the evaluation of dynamics. We consider, however, excessive the economic cost and the investment in time that these examination systems require, for this reason we advocate for the incorporation of an affordable and generalizable clinical diagnosis method of dynamic diseases, such as the Foot Kinetic Index.
Explain that records and evaluation were carried out exclusively by a single observer, for each one of them, and therefore inter-observer validity could not be compared. Specify, however, that this was not the objective of our study.
We consider logistic regression models carried out in this study have strength to provide initial data that could help to design, based on them, other analytical observational studies or cohorts or cases and controls, able of determining risk factors and their respective ORs.
In conclusion, foot function disorders during walking are statistically associated with tibialis posterior and/or peroneals ultrasound-detected tenosynovitis. Foot postural disorders have not been found to be associated to ankle tendons ultrasound disease. Tibialis posterior ultrasound-detected tenosynovitis is associated with foot and ankle dynamic’s overpronation during walking. Foot function disorders increase the likelihood of ankle ultrasound-detected tenosynovitis. An innovative measurement of gait, the Foot Kinetic Index, appears as a diagnostic score capable to detect dynamic disorders. This requires a validation process, with different pressure systems, larger sample size and multicentre design. After that FKI could be used as a diagnostically tool to facilitating clinician decision-making and to improve treatments.
Acknowledgements
Thank to Joan Teva for his good work, patience and free interest. He collected static assessment data of all participants, ever rigorous and efficient; PhD Maria Teresa Puig Reixach for her availability and scientific rigor to critique and improve both the design and the definitive version of this study; also PhD Carmen Moragues for the effort of time in ultrasound assessments initial sample collection.
Ethics approval and consent to participate
Ethical approval for this study was requested to CEIC from “Institut de Recerca de l’Hospital de la Santa Creu i Sant Pau”, in Barcelona. Code number: IIBSP-KPE-2017-48. Ref. HSCSP: 17/281 (OBS). Authorization was requested from Rheumatology Department management. and signed informed consent of each participant was collected, prior to their for- mal acceptance as a participant in the study.
Conflict of interest
All authors declare no financial or other relationship that could lead to a conflict of interest related to this work. The authors alone are responsible for the content and writing of the manuscript. There are no conflicts of interest among any of the authors of this article.
Funding
This research did not receive any specific grant from founding agencies in the public, commercial or not-for-profit sectors.
Declarations of interest
None
Availability of data and materials
The dataset used and/or analysed during the current study are available from the corresponding author on reasonable request.
Authors’ contributions
Conception and study design: ATC, CDT.
Data collection: ATC, PMA, FMS.
Result analysis and interpretation: ATC, FMS.
Creation, drafting, and preparation of the initial draft of the paper: ATC.
Review and final acceptance: ATC, CDT, PMA, FMS.
References