DOI: http://dx.doi.org/10.20986/revesppod.2024.1689/2024
REVISIÓN
Efficacy of arthroscopy in hallux rigidus: a sistematic review
Eficacia de la artroscopia en el hallux rígidus: una revisión sistemática
Diego Mosquera Canosa1
Óscar Miguel Álvarez-Calderón Iglesias2
1Servicio Gallego de Salud, Hospital Arquitecto Marcide A Coruña, España
2Facultad de Enfermería y Podología. Fundación HM de investigación
Abstract
Introduction: Hallux rigidus limits movement and causes stiffness in the joint of the first toe. Arthroscopy is a minimally invasive surgical technique that can facilitate its treatment. Although improvement in pain, function, and progression of hallux rigidus has been observed, the effectiveness of arthroscopy is not conclusively established. This systematic review analyzes the use of arthroscopy in hallux rigidus, evaluating the reduction of pain and the increase in functionality of the first toe in patients undergoing arthroscopic techniques.
Methodology: A comprehensive search was conducted in PubMed, Web of Science, and Scopus following PRISMA guidelines and using JBI scales to assess the quality and risk of bias in the studies.
Results: Seven articles with 138 patients were included. The quality of the studies was moderate, with a moderate risk of bias. Dorsal arthroscopic cheilectomy was the most frequent technique (63.7%). The average follow-up was 22.8 months, showing significant improvements in postoperative range of motion. Improvement in pain and functionality was observed according to AOFAS, VAS, and VPS scales. Satisfaction was high, and the majority would consider undergoing surgery again. Arthroscopy proved effective in improving movement, pain, and functionality of the foot in hallux rigidus compared to conventional surgical techniques. Surgeon skill and pre-surgical evaluation are crucial. Prospective studies with robust methodologies are needed to confirm the efficacy and safety of arthroscopy compared to traditional techniques.
Keywords: Hallux rigidus, arthroscopy, arthroscopic surgery, minimally invasive surgery
Resumen
Introducción: El hallux rigidus limita el movimiento y causa rigidez en la articulación del primer dedo del pie. La artroscopia es una técnica quirúrgica mínimamente invasiva que puede facilitar su tratamiento. Aunque se ha observado mejoría en dolor, función y progresión del hallux rigidus, la eficacia de la artroscopia aún no está concluyentemente establecida. Esta revisión sistemática analiza el uso de la artroscopia en el hallux rigidus, evaluando la reducción del dolor y el aumento de la funcionalidad del primer dedo del pie en pacientes sometidos a técnicas artroscópicas.
Metodología: Se realizó una búsqueda exhaustiva en PubMed, Web of Science y Scopus siguiendo las directrices de PRISMA y utilizando escalas JBI para evaluar la calidad y el riesgo de sesgo de los estudios.
Resultados: Se incluyeron 7 artículos con 138 pacientes. La calidad de los estudios fue moderada, con riesgo moderado de sesgo. La queilectomía dorsal artroscópica fue la técnica más frecuente (63.7 %). El seguimiento promedio fue de 22.8 meses, evidenciando mejoras significativas en el rango de movimiento postoperatorio. Se experimentó mejoría en dolor y funcionalidad según las escalas AOFAS, EVA y VPS. La satisfacción fue alta, y la mayoría consideraría someterse nuevamente a la cirugía. La artroscopia se mostró eficaz en mejorar el movimiento, dolor y funcionalidad del pie en hallux rigidus en comparación con técnicas quirúrgicas convencionales. La destreza del cirujano y la evaluación prequirúrgica son cruciales. Se necesitan estudios prospectivos sólidos para confirmar la eficacia y seguridad de la artroscopia frente a técnicas tradicionales.
Palabras clave: Hallux rigidus, artroscopia, cirugía artroscópica, cirugía mínimamente invasiva
Correspondence: Diego Mosquera Canosa
moscanosadiego@gmail.com
Received: 02-04-2024
Aceptado: 05-20-2024
Introduction
Hallux rigidus (HR) is a painful and degenerative condition of the first metatarsophalangeal joint (MTP) characterized by a progressive decrease in the range of motion and the formation of osteophytes. This disease is the most common form of osteoarthritis in the foot, and its incidence increases with age. The prevalence of HR is more common in females and is more likely to present bilaterally rather than unilaterally(1,2). It was first described by Davies-Colley in 1887, who described it as a plantar flexion of the proximal phalanx in relation to the metatarsal head, which he called hallux flexus. Later, in 1888, Cotterill described it as an HR characterized by painful limitation of movement of the first MTP. DuVries and Moberg indicated that after hallux valgus, HR is the most common pathology affecting the first MTP(3).
The primary cause of HR development is acute trauma or repetitive microtraumas, which can cause an intra-articular fracture. Acute traumas are commonly associated with unilateral involvement and younger patients, while microtraumas are associated with bilateral involvement and older patients. Some authors have proposed correcting the metatarsus primus elevatus as a treatment for HR. However, there are studies describing metatarsus primus elevatus as a consequence of the arthritic progression and loss of range of motion (ROM) of the MTP(3).
Patients with HR present with clinical symptoms manifested by pain during dorsiflexion (DF) or plantarflexion (PF) of the first MTP. Initially, pain occurs in the extreme movements of DF or PF of this joint, but as the disease progresses, pain may also occur in smaller ranges of movement. The characteristic clinical sign is a reduction in the ROM of the affected joint, resulting in an inability to perform plantar flexion during the push-off phase or to stand on tiptoes. A painful dorsal prominence often appears, causing discomfort when in contact with footwear.
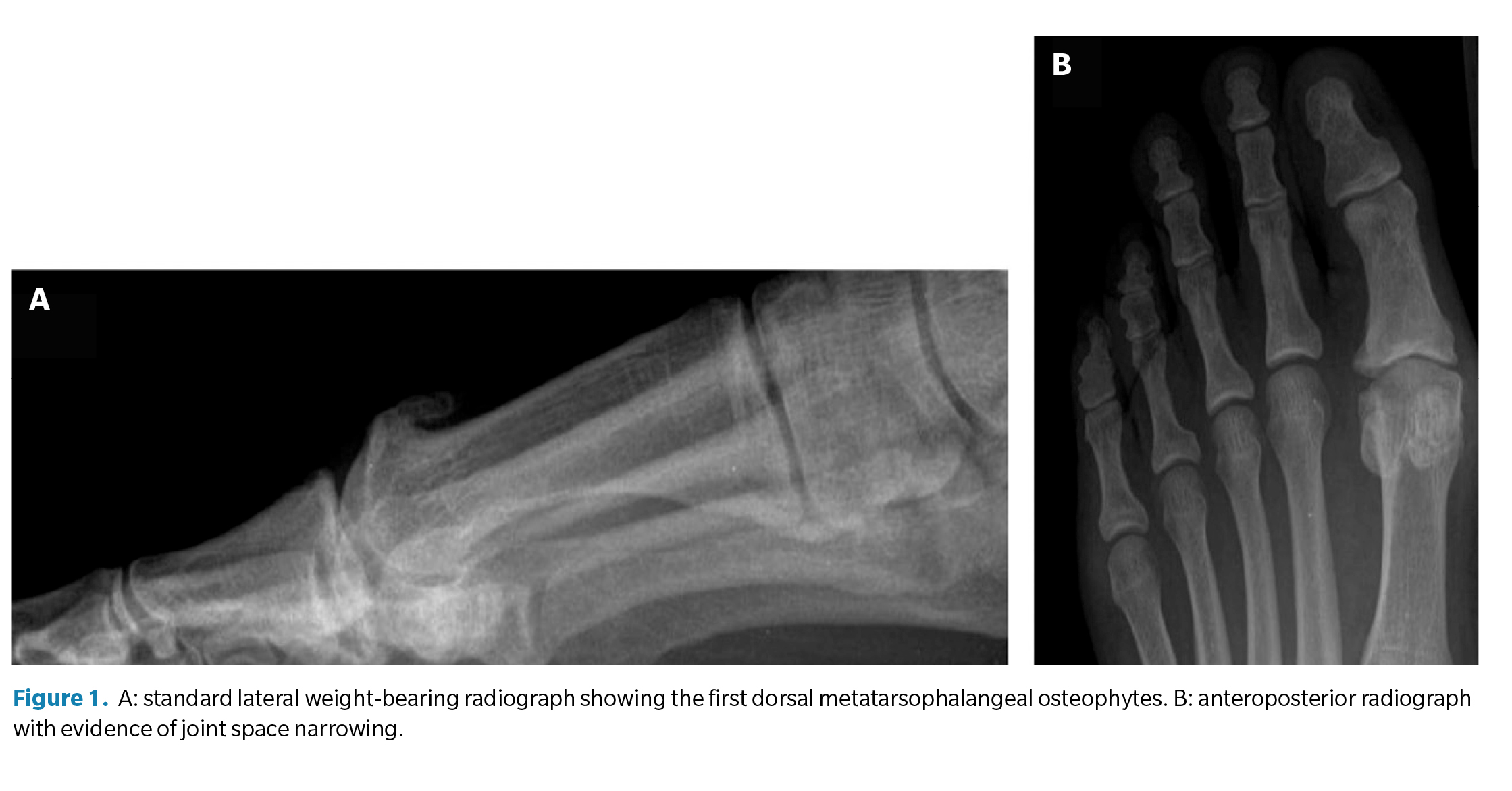
Radiological evaluation of HR is based on an anteroposterior and lateral weight-bearing radiograph (Figure 1). These imaging tests inform surgical decision-making, focusing on joint preservation techniques (cheilectomy), capital osteotomies, arthroplasties, or joint fusion techniques (arthrodesis) in more advanced cases. Lateral radiographs are recommended for identifying dorsal osteophytes and assessing the reduction of the first MTP joint space.
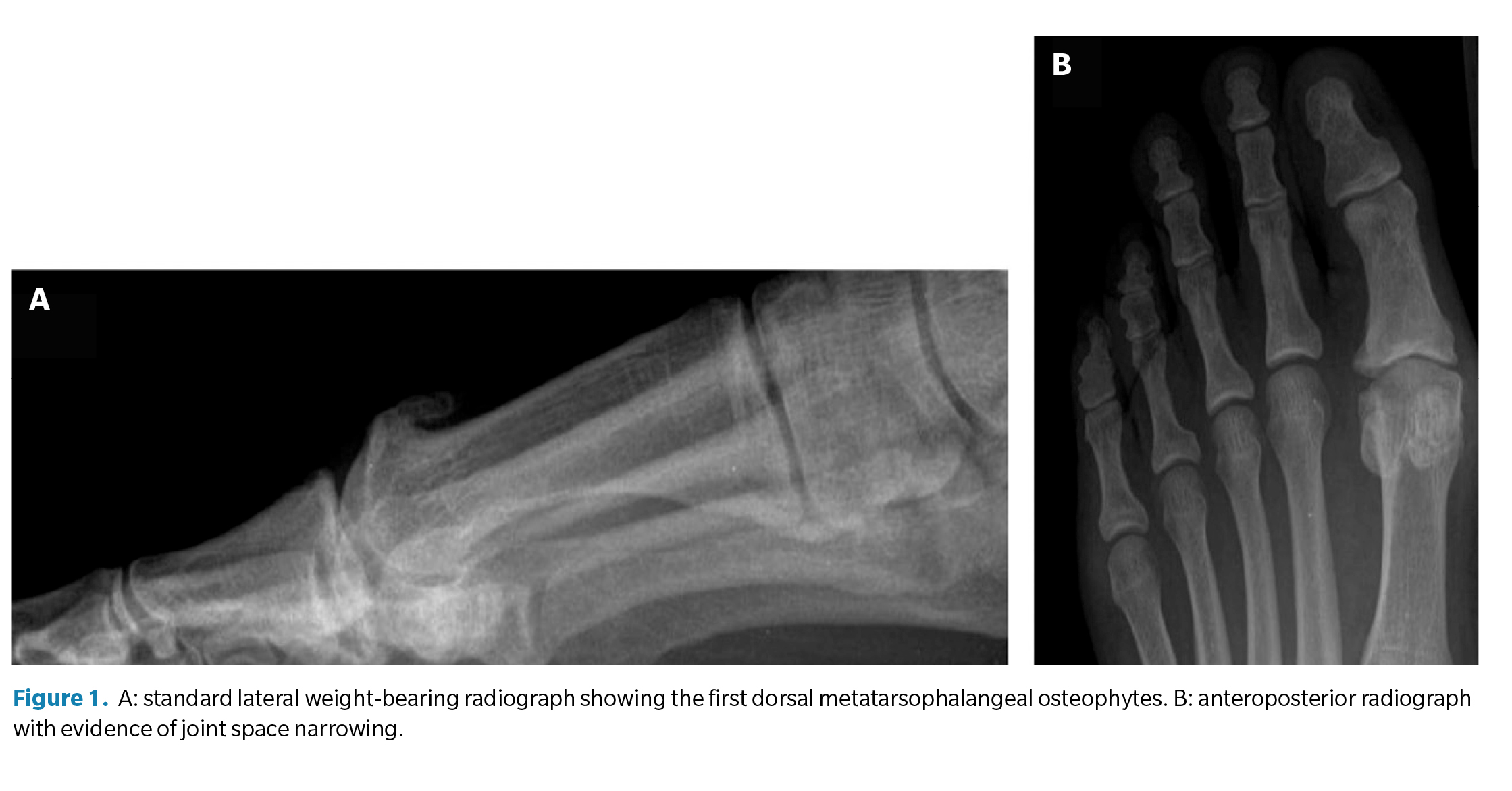
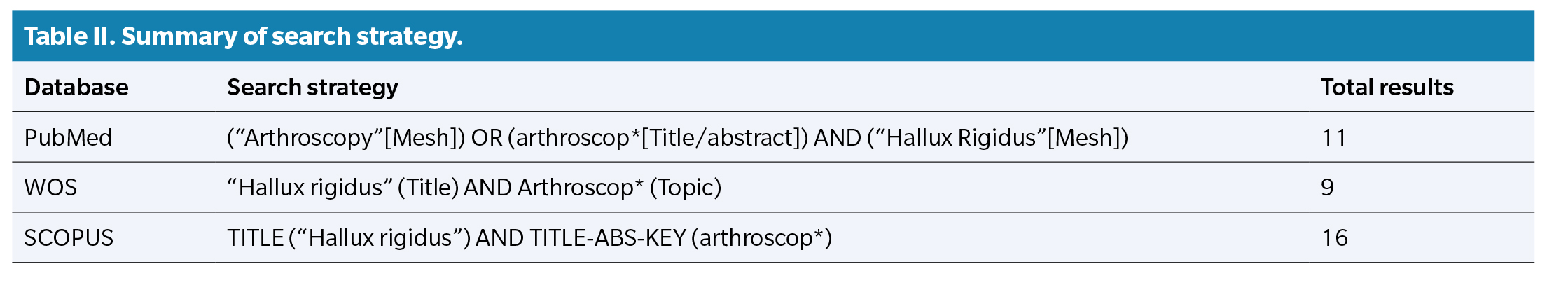
Coughlin’s classification is a useful tool for evaluating HR, combining clinical and radiographic findings. It is based on five severity grades, ranging from minimal loss of motion in the first MTP to complete joint ankylosis. This classification helps establish a treatment plan and determine the best surgical option for the patient. It considers clinical criteria such as the limitation of passive DF, and radiographic criteria, like the presence of osteophytes and the reduction of the first MTP joint space. The five severity grades of Coughlin’s classification are shown in Table 1.
Management of HR involves two approaches: conservative and surgical. Conservative treatment is reserved for the initial grades of Coughlin’s classification, while surgical treatment is applied in more advanced stages. Conservative management may include manipulation under local anesthetics and intra-articular steroid injections to break capsular adhesions, alleviating the flexion contracture seen in HR. Studies have reported³ pain improvement and symptomatic relief for up to 6 months post-treatment, with about one-third of patients eventually requiring surgery.
Surgical approaches for HR explore various techniques(4), including dorsal cheilectomy, dorsiflexion osteotomy, interpositional arthroplasty (hemiimplant), and arthrodesis. Dorsal cheilectomy, commonly used in early stages, involves removing the dorsal exostosis and part of the metatarsal head to improve the range of dorsiflexion and relieve pain. Different modalities are employed, such as open, percutaneous, or arthroscopic techniques.
Arthroscopic treatment of HR has emerged as a viable option in studies(5), offering early recovery and rapid rehabilitation, relieving pain, and improving the range of motion of the metatarsophalangeal joint. Compared to open procedures, arthroscopy presents benefits like a lower incidence of wound complications, quicker rehabilitation, and shorter hospital hospital stays. It can be used for diagnostic purposes, combined with other surgical procedures, or performed simultaneously with others. Surgical indications for arthroscopy in HR include persistent pain unresponsive to conservative treatments, significant stiffness affecting the ability to walk or perform daily activities, and limitation of mobility and flexibility of the toe. Arthroscopy is contraindicated in cases of active infection in the foot or MTP, significant bone damage unaddressable by arthroscopy, and chronic diseases affecting bone healing, such as osteoporosis.
Although the number of comparative studies between open and arthroscopic techniques for HR is limited, some reports indicate that arthroscopy may offer significant advantages. This study aims to evaluate the use of arthroscopy in HR and assess its effectiveness.
Material and methods
Formulation of the study question
The general objective of this study is to analyze the results obtained in the literature regarding the use of arthroscopy in the treatment of HR through a systematic review.
The specific objectives are to assess the reduction of pain and the increase in functionality of the hallux in patients with hallux rigidus treated using arthroscopic techniques.
Following the PICO (population, intervention, comparison, outcome) methodology, the following question is formulated: What is the efficacy of arthroscopy in the treatment of HR? The following items were identified: (P) Population: Adult patients with HR; (I) Intervention: Performing arthroscopy in the management of HR; (C) Comparison: Patients treated for hallux rigidus with non-arthroscopic techniques; (O) Outcome: Efficacy of arthroscopy in terms of pain and functionality from the initial state of the patient.
The study follows the guidelines of the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) 2020 guide(6). The steps taken during the literature search to answer the study question are described below.
Inclusion and exclusion criteria
The inclusion criteria for this systematic review were: adult patients up to 80 years old diagnosed with HR, use of arthroscopy for therapeutic purposes, alone or in combination with other techniques, publication date within the last 10 years (2023-2013), published in English or Spanish.
The exclusion criteria were: animal studies, studies on cadaveric specimens, systematic reviews, case series with fewer than three cases, letters to the editor, or expert opinions.
Search strategy
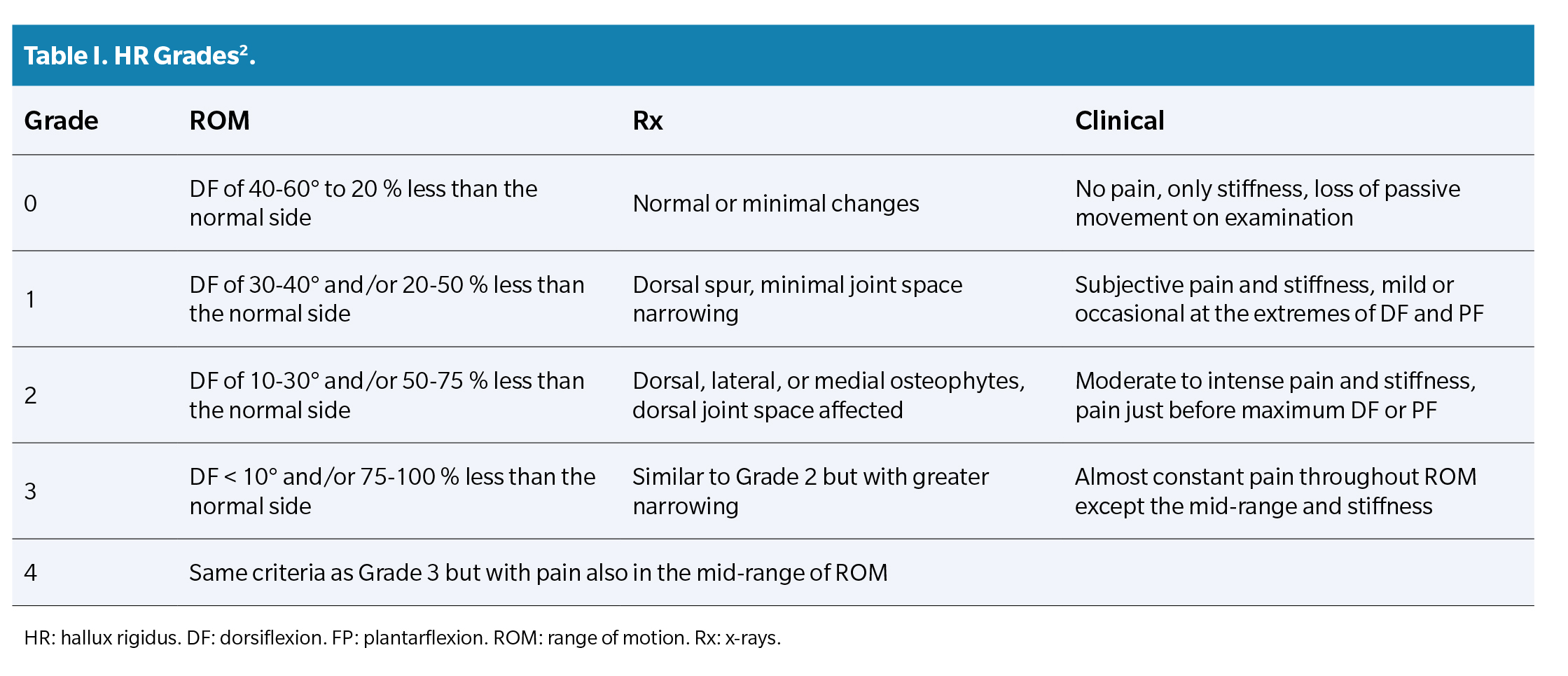
The literature search was conducted in the PubMed, Web of Science, and SCOPUS databases from February through March 2023. The last search was conducted on March 5, 2023. The search strategy in each database is summarized in Table 2, along with the results obtained after applying the aforementioned filters.
Study selection process
The selection of articles for the review was carried out in several phases. First, duplicates were screened using Zotero v. 6.0.21 for removal and organization of bibliographic references. Then, titles and abstracts were filtered, followed by a full reading of the articles for inclusion in the review.
If the abstract did not provide sufficient information, the full article was read to evaluate its inclusion. The study selection process is presented in the following diagram (Figure 2).
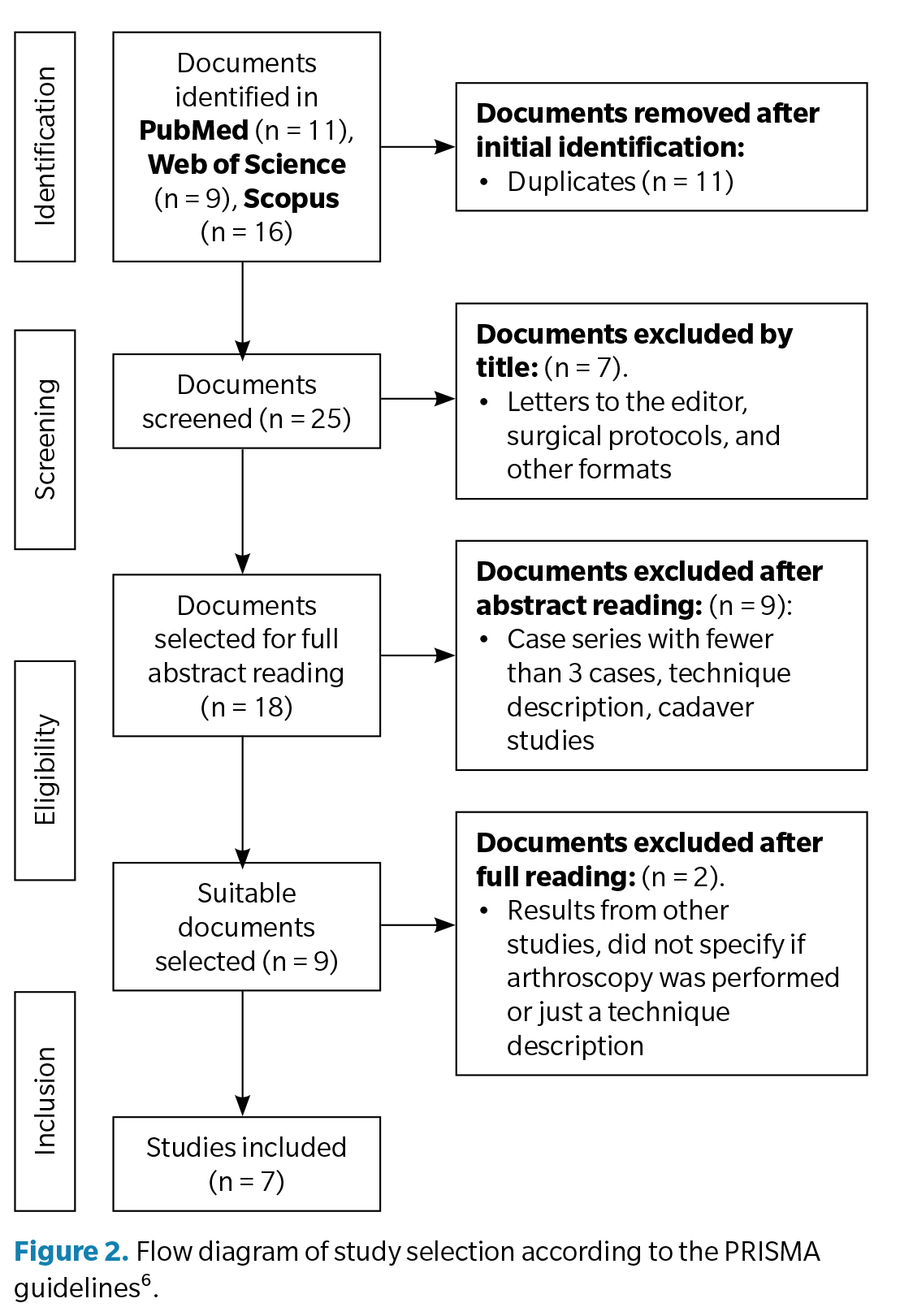
Searches were conducted in PubMed, WOS, and Scopus using pre-established search criteria, obtaining a total of 36 studies. After removing duplicates, 25 studies remained, of which 18 were selected for full abstract review. Nine studies focusing on cadaver techniques or describing the arthroscopic technique and its benefits were excluded. After the first full reading of the studies, two more were excluded for not specifying the use of arthroscopy in the surgical technique or for being technique descriptions. Finally, seven articles were selected for complete analysis.
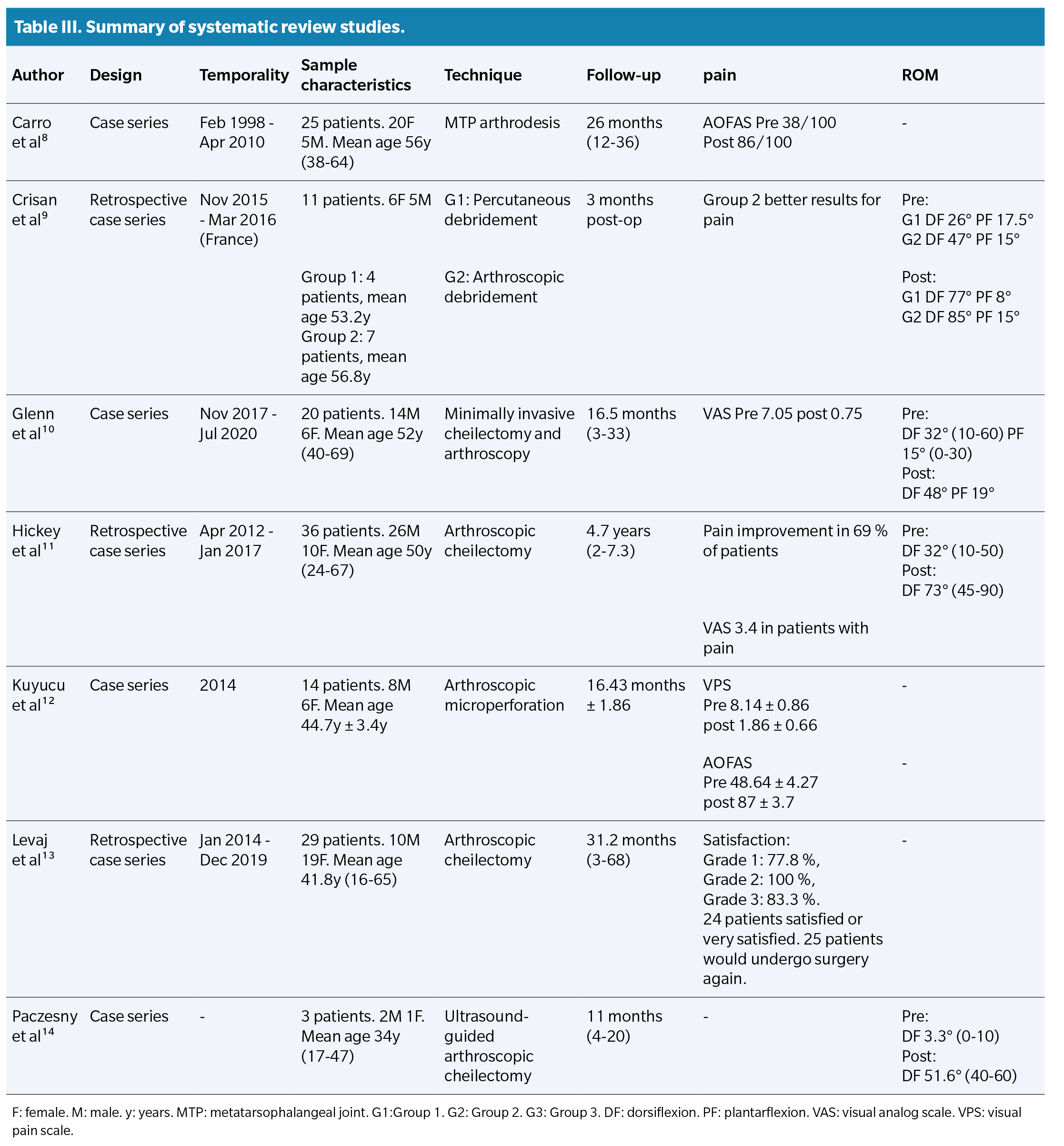
Establishment of variables
From the studies selected in the systematic review, the following variables were established to analyze the results (Table 3): study design and duration, sample characteristics (number of participants, mean age, sex), technique performed, follow-up (months) and results related to pain and ROM.
Quality control and risk of bias
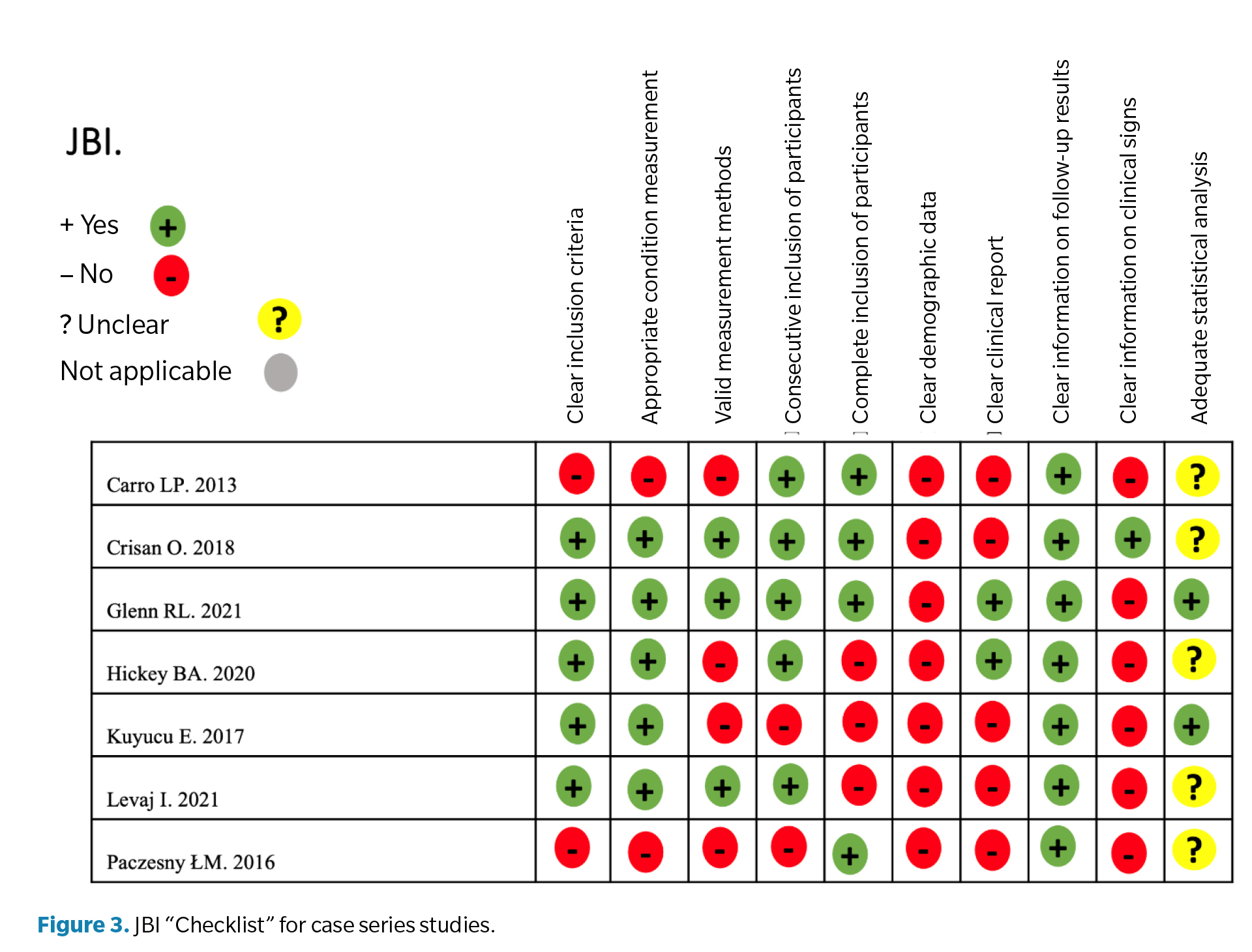
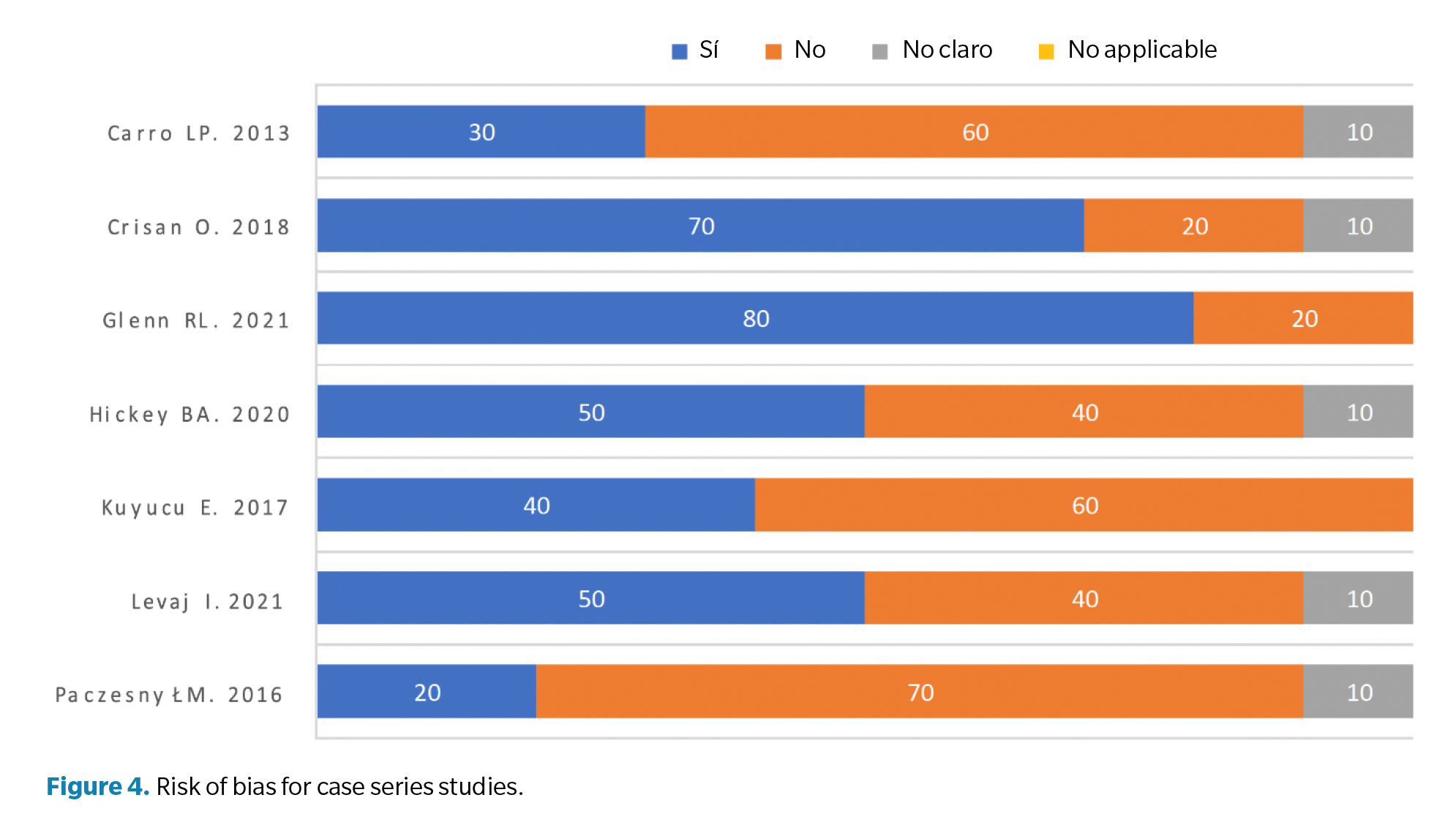
The JBI “Checklist for Case Series” (7) was used to control the quality and risk of bias of the studies. This qualitative analysis involves 10 sections evaluating: clear inclusion criteria for the case series, standardized and reliable condition measurement for all participants, valid methods to identify the condition in participants, consecutive inclusion of participants, complete inclusion of participants, clear demographic data of participants, clear clinical reports of participants, clear information on follow-up outcomes, clear information on the clinics where the study is conducted, and appropriate statistical analysis. Each section was categorized as “Yes” (low risk of bias; +), “Unclear” (moderate risk of bias; ?), “No” (high risk of bias; -), or not applicable as per the corresponding case (Figure 3). Studies were classified as high risk of bias if there were fewer than 50 % “Yes” responses, as moderate risk of bias if the proportion of “Yes” responses was 51-70 %, and as low risk of bias if there were more than 71 % “Yes” responses (Figure 4).
Results
In this systematic review, a total of 7 articles were included, describing a total of 138 patients affected by HR. The quality of the articles was determined to be moderate, with a moderate risk of bias (Figure 4). Of the 138 patients, 86 were women (62.3 %) and 52 were men (37.6 %), with a mean age of 48.3 years (34-56.8).
Various arthroscopically-assisted surgical techniques were used. Among these, the most widely used technique was arthroscopic dorsal cheilectomy, performed on 88 patients (63.7 %). This was followed by MTP arthrodesis in 25 patients (18.1 %), joint microfractures in 14 patients (10.1 %), and arthroscopic and percutaneous debridement in 11 patients (7.8 %). The mean follow-up for the patients was 22.8 months, with a minimum of 3 months and a maximum of 56.4 months.
In a total of 70 patients (50.7 %), the MTP ROM was evaluated both in the preoperative and postoperative periods. It was observed that the mean preoperative DF range was 28 degrees (3.3°-47°), while after the selected surgical technique, the mean postoperative DF range was 66.9 degrees (16°-51°), representing a mean increase of 38.9 degrees in the postoperative DF range.
Among the various surgical techniques performed, it was observed that arthroscopic cheilectomy showed a mean improvement of 31.6 degrees (3.3°-73°) in the DF ROM. On the other hand, arthroscopic debridement showed a mean improvement of 38 degrees in DF movement (47°-85°), while percutaneous debridement showed a mean improvement of 51 degrees in DF movement (26°-77°).
Results related to pain and perceived functionality were evaluated using various validated scales, such as the AOFAS scale (American Orthopaedic Foot and Ankle Society), the VAS scale (Visual Analog Scale), the VPS scale (Visual Pain Scale), and different surveys of personal satisfaction perceived by patients. In a total of 102 patients (73.9 %), pain, functionality, and satisfaction were evaluated.
On the AOFAS scale, a mean improvement of 43.5 points (43-86.5/100) was observed after the surgical technique. The results on the VAS scale indicated a pain reduction of 6.3 points (7.05-0.75), while the VPS scale showed a reduction of 6.28 points (8.14-1.86).
Regarding the personal satisfaction surveys, in a sample of 29 patients who underwent arthroscopic cheilectomy, it was found that 77.8 % of patients with grade 1 HR and 100 % of patients with grade 2 HR were satisfied with the operation. Additionally, 82.7 % were satisfied or very satisfied with the result, and 86.2 % of patients would be willing to undergo the same surgical technique again.
Discussion
The studies presented evaluate different arthroscopically-assisted surgical techniques for the management of HR. Although each study has its own limitations, overall, an improvement in patient symptoms and an increase in MTP mobility after surgical interventions were observed, which is consistent with previously published studies(15,16,17).
In all the included studies, significant improvement in MTP ROM was observed in patients with HR. The technique that demonstrated the greatest improvement in ROM degrees was percutaneous joint debridement, followed by dorsal joint cheilectomy. These findings are consistent with previous research exploring the use of open surgical procedures in the treatment of HR. Specifically, both dorsal cheilectomy and corrective osteotomy of the first metatarsal have shown the best results in terms of efficacy and clinical improvement(18,19).
Moreover, there was a notable improvement in functionality and a reduction in pain in patients undergoing the various evaluated arthroscopic surgical techniques. These results suggest that the interventions were effective in improving function and alleviating pain in patients with HR.
The mean improvement in degrees achieved with arthroscopically-assisted cheilectomy was 31.6 degrees, significantly surpassing the results obtained in other studies using a combination of cheilectomy and Moberg-Akin osteotomy without arthroscopy, with a mean improvement of 16.1 degrees; a cheilectomy using a dorsolateral approach, with a mean improvement of 12.7 degrees; or performing a cheilectomy with a dorsal approach(20,21,22). These findings highlight the superiority of arthroscopically-assisted cheilectomy in terms of ROM improvement and support its efficacy as a treatment option compared to other surgical techniques.
On the other hand, patient satisfaction was high, with a large percentage expressing willingness to undergo the same surgical technique again if necessary. These findings support the efficacy and positive impact of arthroscopy in surgical interventions on the quality of life and well-being of patients with HR.
The results obtained on the AOFAS scale for evaluating arthroscopically-assisted surgical techniques showed a mean improvement of 43.5 points after the intervention vs mean improvements of 31 and 24.6 points in techniques where cheilectomy combined with Moberg-Akin osteotomy and cheilectomy with dorsolateral approach were performed respectively(20,21). In other studies where dorsal cheilectomy was performed, a mean improvement of 53 points was obtained(20).
Regarding pain improvement, a mean improvement of 6.3 points was observed in arthroscopic techniques, which is consistent with findings from other studies where isolated open cheilectomy was performed, showing a mean improvement of 6.35 points(23). However, the results of arthroscopic techniques showed significantly greater pain improvement in other studies, with a mean pain improvement of only 3.8 points(23).
In different studies(8,12,13), the lack of measurement of MTP functionality can be considered a significant limitation, as it is one of the parameters that best evaluates the function of the MTP after surgery.
The lack of a prospective design and the lack of long-term results are also very important limitations(9). In the study by Gleen and collaborators(10), although no major complications were recorded, the need for subsequent fusion in one patient indicated the need for long-term follow-up. The overall follow-up period may not be long enough to fully evaluate the long-term efficacy of the surgery. In the study by Kuyucu and collaborators(12), the outcome scores are not presented in detail, making it difficult to fully assess the magnitude of the improvement.
The studies conducted by Kuyucu et al. and Paczesny et al.(12,14) presented small sample sizes, which implies a limitation in the validity and generalization of the results obtained. Additionally, it is important to consider that the experience of the surgeon performing the surgical technique can influence the results of these studies, as their skill and dexterity may vary among different professionals.
The lack of classification and segregation of surgical outcomes based on the degree of HR in the analyzed studies may complicate the comparison of results between studies. It can be summarized that each surgical technique has its own advantages and limitations, and the choice of treatment should be based on the individual characteristics of the patient and the surgeon’s experience, which can significantly influence the outcome of the surgery.
In conclusion, the findings of this study have demonstrated that arthroscopically-assisted surgical techniques in the treatment of HR are effective and appear to provide an improvement in postoperative ROM compared to surgical techniques performed without this method. There is substantial improvement in pain relief and foot functionality when using arthroscopic techniques compared to traditional open surgery techniques. There is no clear consensus on which arthroscopically-assisted surgical technique is superior in the treatment of HR. The efficacy of the intervention and the occurrence of postoperative complications are significantly influenced by the surgeon’s skill during the technique’s execution, as well as the preoperative study of the patient. Prospective cohort studies with good methodology, sufficient sample size, and adequate statistical power are needed to confirm the efficacy and safety of arthroscopic surgery.
Conflict of interest
The authors declare no conflicts of interest regarding this paper.
Funding
None.
Authors contribution
Conception and design: DMC.
Data collection: DMC.
Results analysis: DMC.
Creation and redation of initical draft: DMC.
Final Review: OMA-CI.
References