DOI: http://dx.doi.org/10.20986/revesppod.2024.1676/2023
ORIGINAL
Use of Limb Occlusion Pressure as a method for calculation of intraoperative ankle tourniquet pressure in forefoot surgery: a prospective case series
Uso de Presión de Oclusión de Extremidad como método de cálculo de la presión intraoperatoria del torniquete en tobillo en cirugía del antepié: serie de casos prospectiva
Javier Pascual Huerta1
Leticia Palacio Fernández1
Lucía Trincado Villa1
Antonio González Fernández1
Eduardo Mongil Escudero2
1Clínica del Pie Elcano. Barakaldo, Vizcaya, España
2Servicio de Anestesia y Reanimación. Hospital Universitario de Galdakao, Vizcaya, España
Abstract
Objetives: The use of tourniquets in foot surgery can produce complications. It was assessed que quality of surgical field hemostasis and its complications with the use of an ankle tourniquet whose pressure was determined by using the Limb Occlusion Pressure (LOP) method.
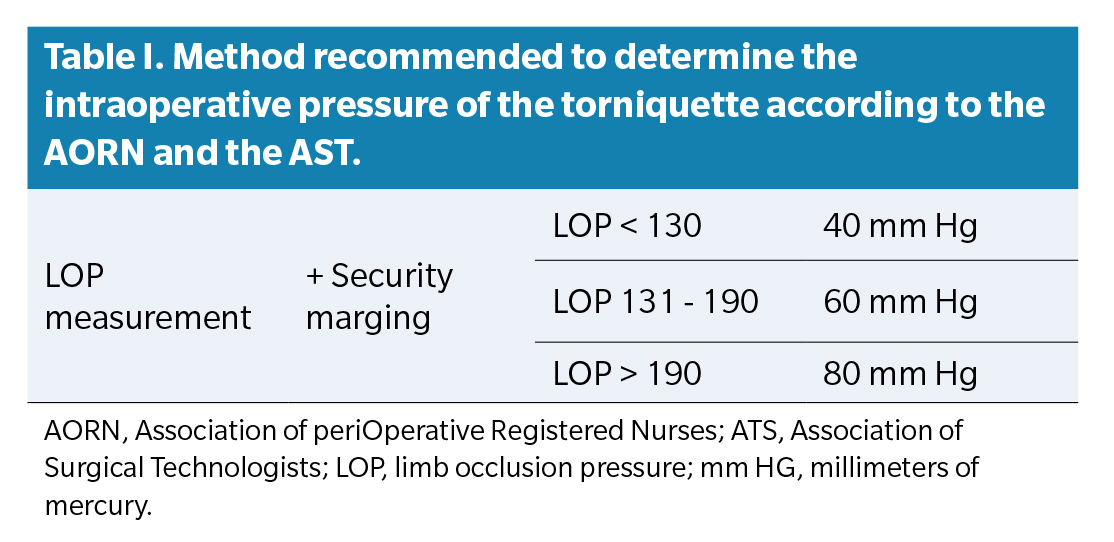
Patients and methods: Patients surgically treated with an ankle tourniquet were included. Pressure of the tourniquet was calculated using LOP method with a cuff at the ankle until Doppler stethoscope sound was not detected. A security margin was added of 40, 60 or 80 mm Hg if LOP value was less than 130, between 131-190 or more than 190 respectively. Quality of surgical field was graded as Excellent, Good, Fair and Bad.
Results: A total of 116 patients were included. Mean pressure was 192.73 ± 31.73 mm Hg and mean time of ischemia was 73.92 ±
33.09 minutes. Quality of the surgical field was Excellent in 84 cases (72.4 %), Good in 26 cases (22.4 %) and Fair in 6 cases (5.2 %) with no Bad cases.
Conclusions: The surgical field was considered Excellent or Good in 94.8% of the cases with ankle pressures noticeably lower than those traditionally used in the ankle for foot surgery. The use of LOP method to calculate tourniquet pressures at the ankle is a valid and safe method that allow a bloodless surgical field with minimal complications.
Key words: Pneumatic tourniquet, pressure, limb oclussion pressure, foot surgery, ischemia, ankle
Resumen
Objetivos: El uso de torniquetes en cirugía del pie puede presentar complicaciones. Se valoró la calidad del campo quirúrgico exangüe y la aparición de complicaciones con el uso de torniquete localizado en el tobillo, determinando la presión mediante el método de Presión de Oclusión de Extremidad (LOP).
Pacientes y métodos: Se incluyeron a pacientes intervenidos quirúrgicamente del pie con torniquete en el tobillo. La presión con método LOP se determinó con manguito en el tobillo hasta que se perdía el pulso con onda doppler, y al que se añadió un margen de seguridad de 40, 60 u 80 mm Hg si el valor LOP era menor de 130, entre 131-190 y mayor de 190 mm Hg, respectivamente. La calidad del campo quirúrgico fue catalogada como Excelente, Buena, Regular y Mala.
Resultados: Se incluyeron un total de 116 pacientes. La media de presión utilizada fue de 192.73 ± 31.73 mm Hg y el tiempo medio de isquemia 73.92 ± 33.09 minutos. La calidad del campo quirúrgico fue Excelente en 84 casos (72.4 %), Buena en 26 casos (22.4 %) y Regular en 6 casos (5.2 %) sin ningún caso de Mala calidad.
Conclusiones: El campo quirúrgico fue considerado como Excelente o Bueno en el 94.8 % de los casos con el uso de presiones sensiblemente inferiores a las clásicamente utilizadas en el tobillo para cirugía del pie. El cálculo de la presión del torniquete en el tobillo mediante el método LOP es un método válido y fiable que permite un campo quirúrgico exangüe con mínimas complicaciones.
Palabras clave: Torniquete neumático, presión, presión de oclusión de extremidad, cirugía del pie, isquemia, tobillo
Correspondence: Javier Pascual Huerta
javier.pascual@hotmail.com
Received: 10-09-2023
Acepted: 12-04-2023
Introduction
Surgical tourniquets are routinely used in limb surgery to improve visualization of the surgical field, allowing for more precise technical work in a safe and faster environment,(1,2) thereby avoiding injuries or technical errors due to lack of visibility and reducing blood loss.(3) Despite all these benefits and technological advances in tourniquet management,(4) their use is not without problems or risks, which are well documented in the literature (5,6,7,8,9)
Ischemia and pressure are the two main iatrogenic factors involved in the use of intraoperative tourniquets. Metabolic effects are associated with the sequelae produced by sustained ischemia, while nerve and muscle tissue injuries are directly related to local compression produced by the tourniquet itself and the duration of that local pressure.(10,11) As of today, there is no safe intraoperative pressure that can be used without risking injury to structures, and the most appropriate way to calculate that pressure remains unknown.
However, in recent years, the concept of LOP (limb occlusion pressure) has been developed, defined as the minimum pressure of the tourniquet to stop arterial flow distal to it, which would be the tourniquet pressure required to maintain a bloodless surgical field.(12) The Association of periOperative Registered Nurses (AORN) and the Association of Surgical Technologists (ATS) in the United States recommend calculating this value and using it as a system to estimate the intraoperative tourniquet pressure, with an added safety margin of 40, 60, or 80 mm Hg, depending on whether the LOP value is less than 130 mm Hg, between 131 and 190 mm Hg, and greater than 190 mm Hg, respectively (Table 1). (12,13). This system is known as the LOP method for calculating the intraoperative tourniquet pressure in each specific patient.
Several studies have shown that the LOP method is a valid system for achieving a bloodless surgical field, minimizing the risk of injuring tissues subjected to compression by the tourniquet in adults(14,15,16,17) and children. (18) However, in most of these studies, the cuff was placed in the thigh or arm, and the use of LOP in other locations, such as the leg or ankle, has been much less studied. Ankle tourniquet placement is very common in foot surgery performed by podiatrists, as it is usually better tolerated by patients and allows surgery to be performed with distal local anesthetic blocks in the foot without the need for general anesthesia or more proximal anesthetic blocks (popliteal or spinal). Pauers and Carocci(19) studied the effect of optimizing ankle tourniquet pressure using 200 mm Hg, a method different from LOP, so we do not know to date if this LOP system is a valid method for calculating intraoperative tourniquet pressure when the location is the ankle.
For all these reasons, the aim of this study was to evaluate the quality of the bloodless surgical field and the occurrence of complications associated with the use of ankle tourniquet for foot surgery, determining the tourniquet pressure using the method recommended by AORN and AST based on LOP calculation. The aim was to assess whether using this method at the ankle achieves a valid hemostasis system that allows for a bloodless surgical field while minimizing problems associated with tourniquet use due to pressure exerted on the ankle.
Patients and methods
Study design
This was a prospective, cross-sectional case series study conducted on patients undergoing foot surgery requiring the application of a surgical tourniquet at the ankle. The drafting of this article followed the recommendations of the STROBE guidelines for reporting observational studies. (20)
Study population
All patients consecutively undergoing foot surgery at Clínica del Pie Elcano (Bilbao, Vizcaya, Spain) who met the following inclusion criteria were included: 1) patients older than 18 years undergoing surgery in the forefoot, performed with a pneumatic tourniquet placed at the ankle regardless of the duration of its application, and 2) procedure performed using distal local anesthesia (ankle or foot) along with conscious sedation administered by an anesthesiologist. Cases of foot surgery where an ankle tourniquet was not used (for example, nail surgery) or where other types of hemostasis, such as vasoconstrictors (adrenaline) associated with local anesthetics, were used were excluded.
All patients were private patients at Clínica del Pie Elcano (Bilbao, Vizcaya, Spain) who voluntarily attended the center for the treatment of pain and/or deformities in the forefoot and who voluntarily accepted surgical treatment. Data collection was conducted from December 2018 through December 2022. The present study is classified as an observational case series study with prospective character. While conducting this study the routine clinical practice of such center was not altered whatsoever.
Protocol and procedures
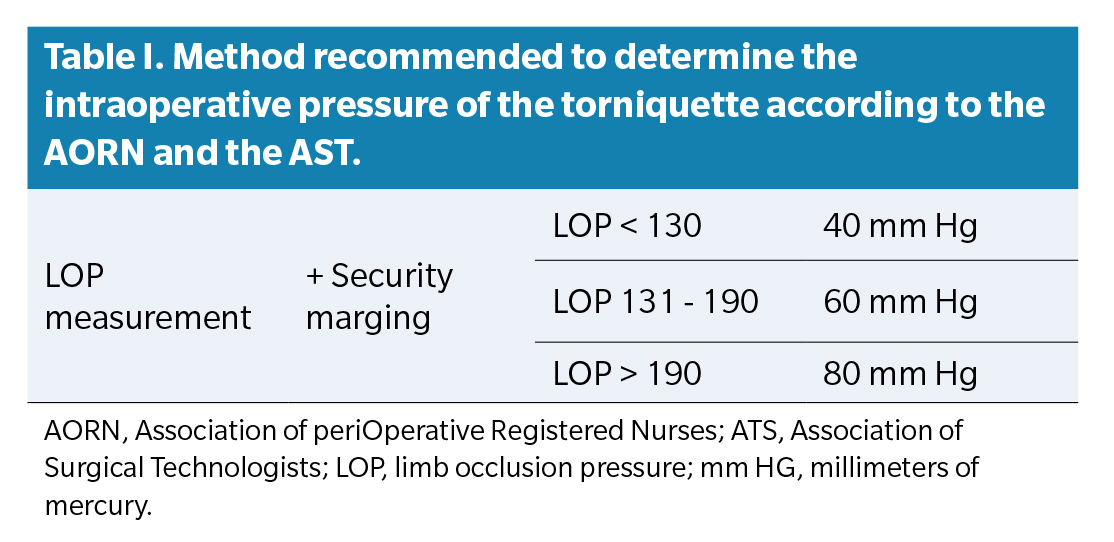
Once the patient was in the operating room, a peripheral vein was cannulated with an IV catheter in the arm, and 0.9% saline solution was administered along with drugs for the conscious sedation procedure performed by the anesthesiologist (E.M.E.). This procedure involved administering midazolam and fentanyl at low doses adjusted to the patient’s weight and continuous infusion of propofol throughout the procedure (target-controlled infusion system between 0.5-1.5 mg/ml) to achieve sedation with the patient asleep and on spontaneous breathing, who could be awakened by tactile or verbal stimulation (Ramsay scale level 3).21 Immediately after administering this drug for conscious sedation, and before performing the local anesthetic block in the foot, the LPO value was calculated in the limb to be operated on. The LOP value was obtained by placing an automatic pressure cuff that calculated the arterial pressure at the ankle (HEM-M3-7131E; OMRON HEALTHCARE Co., Ltd., Kyoto, JAPAN), and with a bidirectional Doppler using an 8 MHz probe (Sonoline B, Contect Medical Systems co., Ltd.; China), the flow of the distal pedal artery to the pressure cuff was located. In cases where the pedal artery could not be located (there is a percentage of around 5% of the population with absent or vestigial presence of the anterior tibial and pedal artery),22 the posterior tibial artery was used for this measurement. Once the artery was perfectly located with the Doppler probe, the ankle pressure cuff was inflated to a pressure at which the Doppler wave sound disappeared, indicating complete collapse of the artery. Afterwards, the automatic pressure cuff began to calculate the arterial pressure by gradually decreasing the pressure in the ankle at a rate of approximately 3-5 mm Hg per second. When the Doppler signal recovered, the marked pressure was estimated as the LOP pressure (Figure 1). This procedure was always performed with the patient in a supine position (not sitting and with the heart approximately at the level of the artery of the foot to be explored) and was repeated 2 times consecutively in each patient to ensure the reliability of the measurement. The highest pressure of the 2 measurements was always taken as the LOP pressure. However, in cases where a difference of more than 10 mm Hg was observed between the first and second readings, a third reading was used to determine the LOP pressure. All LOP calculations were performed by 2 podiatrists who were authors of the article (J.P.H. and L.P.F.), and who had previously practiced together the protocol that should be followed for the LOP calculation. All patients were constantly monitored by the anesthesiologist for their heartbeat, blood pressure, and oxygen saturation during the procedure.
In all cases, a 13 cm-wide manual pneumatic tourniquet (Komprimeter, Riester®, Phoenix, AZ, USA) with a straight design (not contoured to the limb) was used. The tourniquet was applied after previously emptying blood by sweeping with a Smarch tape applied to the foot. The application time of the tourniquet never exceeded 120 minutes. In cases where the procedure lasted more than 120 minutes, either the technique went on without a tourniquet (“wet”) until the surgery was finished, or a reperfusion pause of, at least, 20 minutes was taken before reapplying the tourniquet at the ankle. The new application of the tourniquet never exceeded 30 minutes.
Variables and measurements
All surgical procedures were performed by the same podiatrist, the author of this article (J.P.H.), who was in charge of the patients during the surgical process. Once the surgery was completed, this author assessed the quality of the bloodless surgical field at the end of the procedure. This assessment of the bloodless field was performed qualitatively and was based on a four-category scale: 1) Excellent: bloodless intraoperative surgical field with excellent visualization; 2) Good: slight or minimal bleeding allowing the technique to be performed without having to change the tourniquet pressure; 3) Fair: intraoperative bleeding requiring increasing the tourniquet pressure during surgery, not because the cuff pressure has decreased, but because the calculated pressure does not allow working due to lack of field visibility; 4) Poor: abundant intraoperative bleeding requiring repeating foot exsanguination. Similarly, all incidents or complications that could be related to the use of the tourniquet during surgery were noted during the postoperative period: local pain in the tourniquet placement area, postoperative neurological symptoms compatible with nerve injury due to the tourniquet, skin injury due to compression exerted by the tourniquet, and thrombophlebitis and deep vein thrombosis. The existence of immediate cardiovascular or respiratory events after tourniquet deflation was also noted.
Data were filled in during the preoperative period and immediately after surgery on a data sheet for each patient, which were then transferred to a database along with the patient’s age and sex, systolic blood pressure in the arm, systolic blood pressure in the ankle, ankle/brachial index (ABI), LOP value, tourniquet pressure used during surgery, and quality of the surgical field. Follow-up of all patients was conducted during the usual postoperative course following the standard protocols of the center where the study was conducted. Postoperative consultations were conducted until discharge, which occurred, at least, 12 months after surgery. Any incidents during this period, especially related to tourniquet use, were tracked, and recorded in the database.
Statistical analysis
The mean ± standard deviation of quantitative variables and simple percentages for categorical variables were calculated. An estimation of the quality of the bloodless surgical field was obtained using simple percentages, while differences in the values of the pressure used and systolic pressure in the arm and ankle were analyzed in the different groups of surgical field quality (Excellent, Good, Fair, and Poor) using a hypothesis contrast test through the Kruskal-Wallis H test (the non-parametric equivalent to the ANOVA test). P values < 0.05 were considered statistically significant. All calculations were performed using the IBM SPSS Statistics® program (version 26).
Results
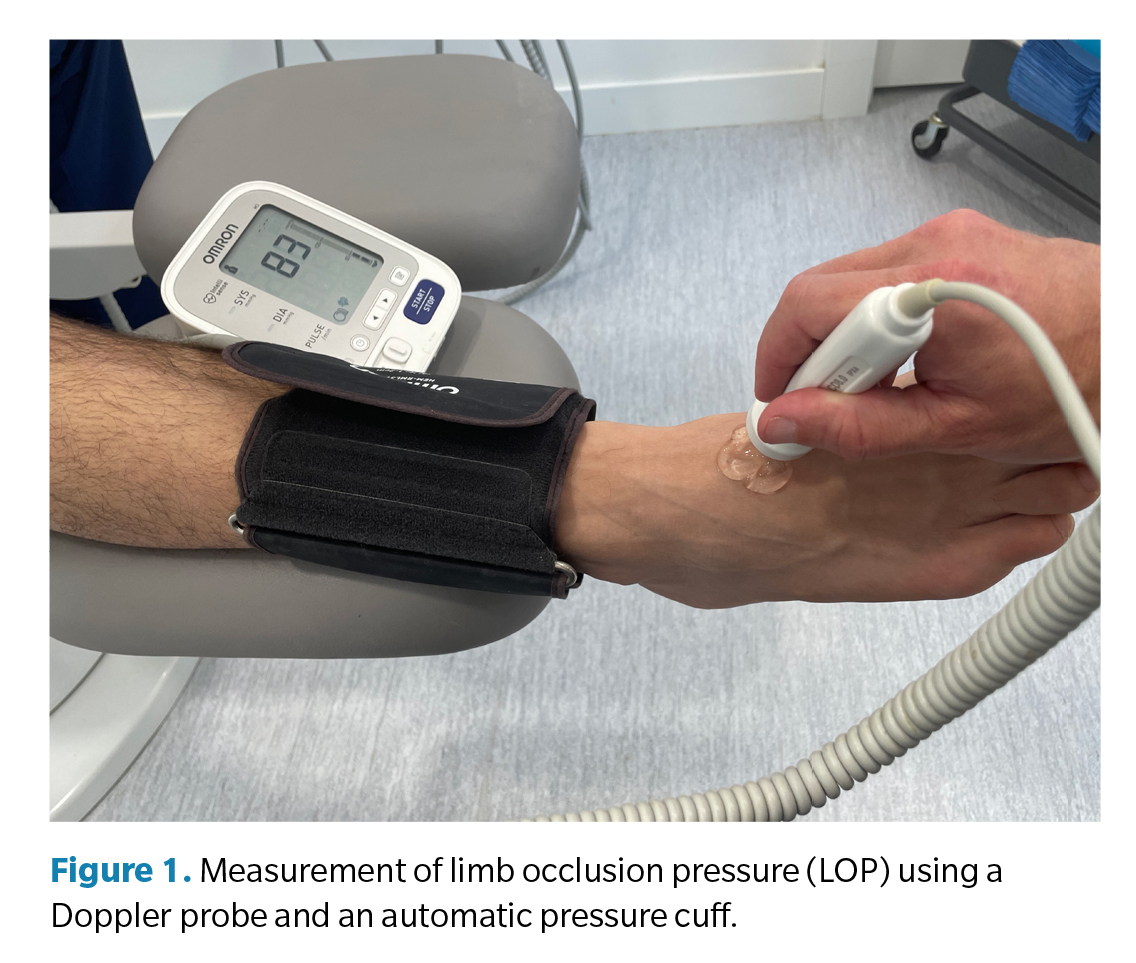
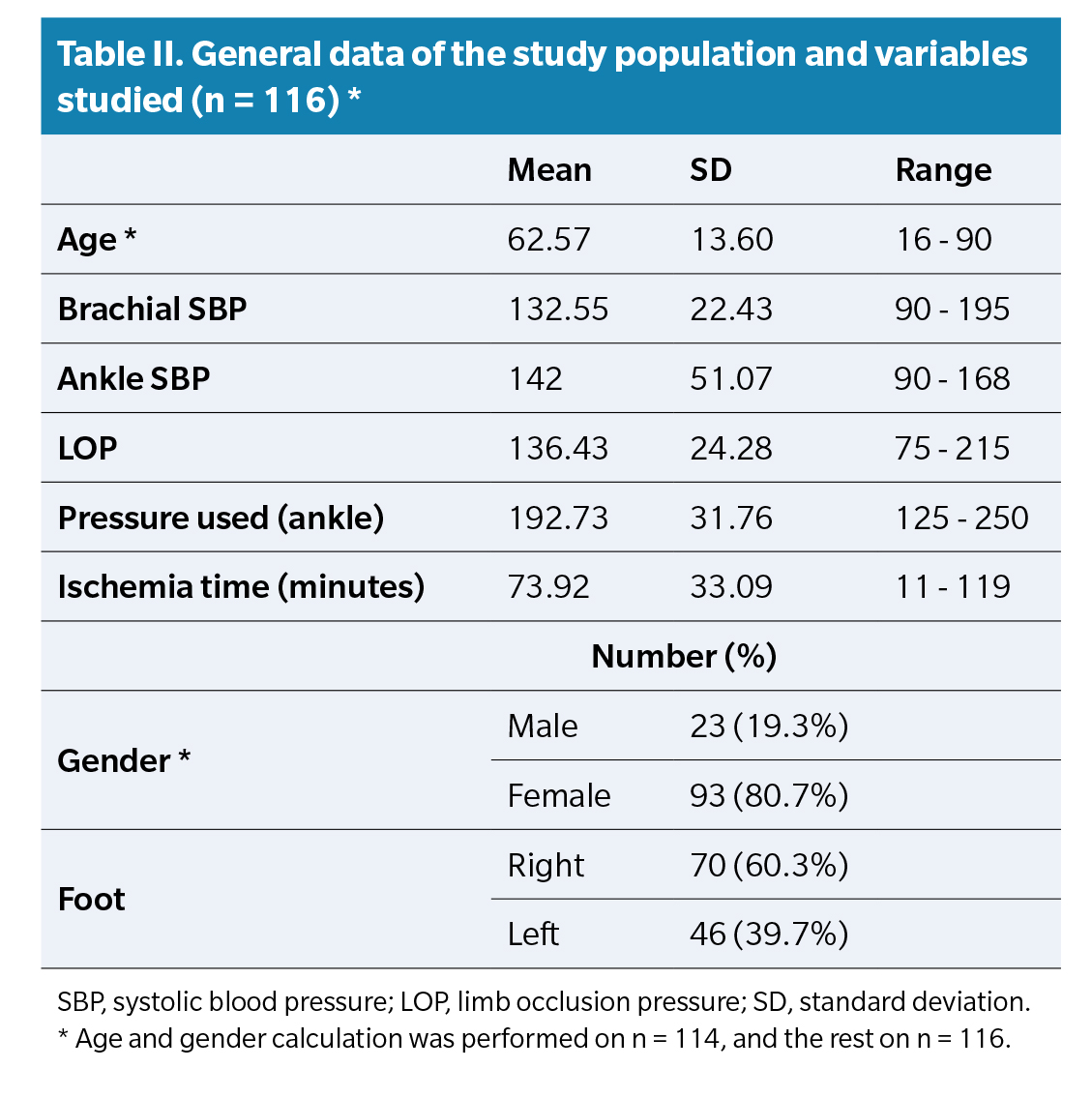
A total of 124 patients were analyzed, 8 of whom had missing measurements that prevented their inclusion in the study, resulting in a final sample of 116 patients. In 2 out of the 116 cases, it was impossible to locate their age and gender on the data collection sheet, although the rest of the values were correctly filled out, so they were included in the pressure analysis and variable calculation but not in the calculation of age and gender for the sample. Table 2 shows the basic population data and study variables. The mean pressure used in the total sample was 192.73 ± 31.76 mm Hg, and the mean ischemia time used was 73.92 ± 33.09 minutes.
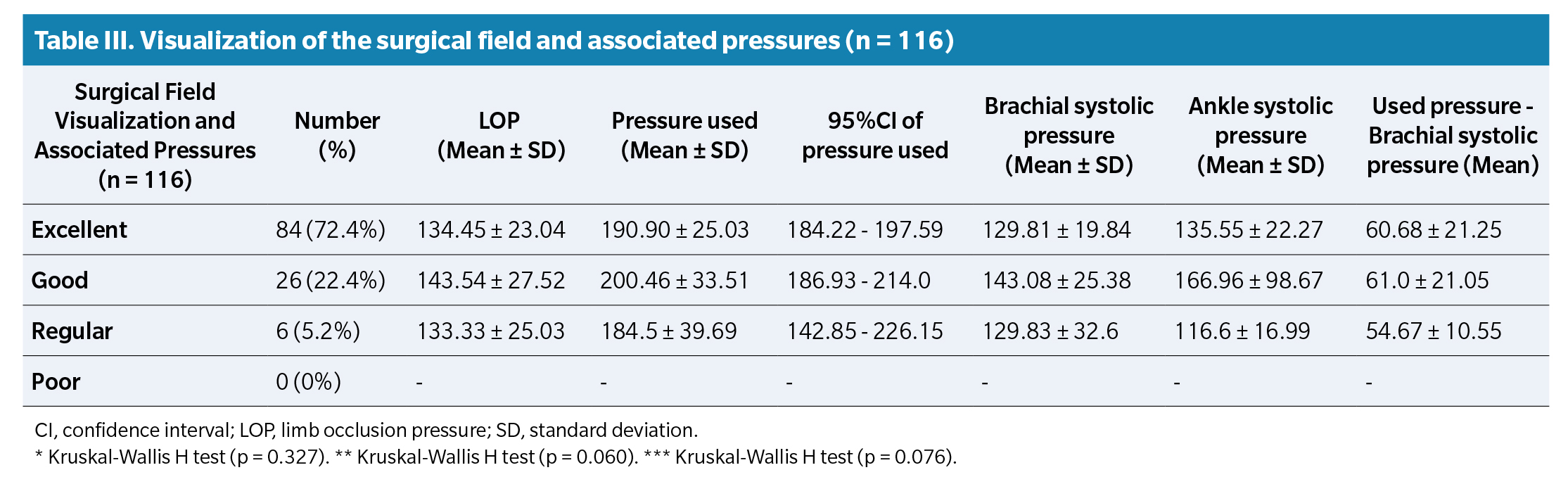
Table 3 shows the percentages of surgical field quality and systolic blood pressure values in the arm and ankle, as well as the LOP in each category. Using the method described with the LOP value, the quality of the surgical field was Excellent in 84 cases (72.4%), Good in 26 cases (22.4%), and Fair in 6 cases (5.2%). No cases of poor-quality surgical field were ever reported. The Kruskal-Wallis test did not show statistically significant differences between the Excellent, Good, and Fair quality field groups, both in the pressure used (p = 0.327) and in the systolic blood pressure in the arm (p = 0.060) and ankle (p = 0.076).
In 9 cases, the initial hemostasis time of 120 minutes was exhausted, and hemostasis reutilization with a tourniquet was performed during surgery with a previous reperfusion period of the foot between 20 and 30 minutes (mean, 27.5 ± 5.2 minutes), followed by a second hemostasis time lasting between 5 and 30 minutes (mean, 22.2 ± 8.2 minutes). None of the cases required a third use of hemostasis.
No cardiovascular or respiratory events were recorded during exsanguination and tourniquet deflation in the study patients. Complications were reported in 2 patients in the study that could be related to tourniquet use: one of them was the presence of localized deep vein thrombosis in the intervened leg, which was conservatively treated on an outpatient basis and followed up by their primary care physician. This patient had a pressure of 195 mm Hg for 120 minutes and was one of the patients in whom ischemia was reapplied for 30 minutes after a 30-minute reperfusion window. The second was the presence of postoperative neurological pain at the tourniquet application site, which subsided favorably 4 to 6 weeks after the intervention without sequelae. In this case, the tourniquet pressure used was 165 mm Hg for 102 minutes.
Discussion
Injuries to vessels, nerves, or other tissues, whether temporarily or permanently, are complications due to the incorrect use of the tourniquet during limb surgery. Most of the literature maintains that mechanical trauma due to tourniquet pressure is the most important factor in the pathogenesis of these injuries related to its use.(23,24,25,26,27) Classic studies by Ochoa et al. concluded that nerve injuries were caused by increased pressure at the edge of the cuff, which was the location where nerve lesions histologically occurred with displacement of the Ranvier nodes, showing that it was compression neuropraxia rather than ischemic neuropathy the cause of the paralysis produced by the tourniquet.(28,29) Within this context of compressive nerve injury, lesions can appear as a consequence of incorrect tourniquet placement, incorrect size of the tourniquet, excessive pressure, and/or prolonged use, generally exceeding 2 hours. Determining the appropriate tourniquet pressure sufficient to create a bloodless field and, at the same, time avoid tissue damage due to compression is a difficult task whose answer remains elusive. The present study aimed to assess the quality of the bloodless field in foot surgery with the tourniquet placed on the ankle, using the method recommended by AORN and ATS which uses the LOP value as a reference. As far as the authors know, this is the first study ever conducted to measure the clinical effectiveness of using LOP as a method of calculating the pressure used by the tourniquet when located on the ankle. This clinical assessment had been performed in other studies using the LOP method in the thigh(14,16,17) but not in the ankle.
In podiatry foot surgery, tourniquets have historically been used for years on the ankle with a minimal rate of complications. In a study on the use of pneumatic tourniquets on the ankle in 3027 podiatric surgery procedures performed in the United States, only 5 complications were described.30 However, determining the tourniquet pressure used on the ankle is not performed under fixed or standardized parameters. Historically, this has generally been done using 3 methods. The first method consists of always using a fixed pressure that is not changed, usually 350 mm Hg in the thigh and 250 mm Hg on the ankle. The second method consists of adjusting the pressure relative to the patient’s systolic blood pressure, adding an increment that varies between 75-150 mm Hg depending on the anatomical location of the tourniquet, always avoiding exceeding 250 mm Hg on the ankle.31 The third method consists of using the LOP method, recommended by AORN and ATS,(12,13) which is the one used in the present study, by calculating the patient’s LOP value in the immediate preoperative period and adding a safety margin (Table 1)
As f, this is the first study that has measured the clinical effectiveness of using LOP (Estimated Occlusion Pressure) as a method for calculating the pressure used by the tourniquet when located at the ankle. This clinical assessment had been carried out in other studies using the LOP method in the thigh, but not at the ankle.
Historically, ankle tourniquets have been used for years in foot surgery by podiatrists with a minimum complication rate. In a study on the use of pneumatic tourniquets at the ankle in 3027 podiatric surgery procedures performed in the U.S., only a total of 5 complications were described. However, determining the tourniquet pressure used at the ankle is not done under fixed or standardized parameters. Historically, this has generally been done using three methods. The first method consists of always using a fixed pressure that is not changed, typically 350 mm Hg in the thigh and 250 mm Hg at the ankle. The second method consists of adjusting the pressure based on the patient’s systolic blood pressure, adding an increment ranging from 75-150 mm Hg depending on the anatomical location of the tourniquet, always avoiding exceeding 250 mm Hg at the ankle. The third method consists of using the LOP method, recommended by the AORN and the ATS, which is the method used in the present study, calculating the patient’s LOP value in the immediate preoperative period and adding a safety margin (Table 1).
The present study has shown that the use of the LOP method for calculating tourniquet pressure at the ankle is a method that allows working under a bloodless surgical field with pressures significantly lower than those historically used of 250 mm Hg at the ankle. In the present study, in 110 out of 116 patients (94.8%), the surgical field was categorized as Excellent or Good using this method, and the mean pressure used was 190.90 ± 25.03 mm Hg in cases where the surgical field was considered Excellent (72.4% of the overall sample) and 200.46 ± 33.51 mm Hg in cases where the surgical field was considered Good (22.4% of the overall sample). These results are similar to those reported by Pauers and Cacori, who used a slightly curved tourniquet inflated to 200 mm Hg, in which in 90% of cases adequate hemostasis was achieved with minimal postoperative complications.19 The results of the present study suggest that using a fixed pressure of 250 mm Hg at the ankle overestimates the pressure needed to achieve a bloodless surgical field in which one can work comfortably. Similarly, using a safety margin of 100 mm Hg above the systolic blood pressure(32,33) can overestimate, in many cases, the pressure needed to produce a bloodless surgical field. In the present study, the difference between systolic blood pressure and the pressure used at the ankle using LOP calculation was 60.43 ± 21.64 mm Hg for the total sample, and Table 3 shows that value in the different groups of surgical field quality. In light of these results, it seems that using this rule (systolic blood pressure + 100 mm Hg) for calculating tourniquet pressure may not be ideal.
The LOP value is related to various variables of the patient, such as systolic blood pressure, ankle-brachial index, limb size, and external variables such as tourniquet design (straight or contoured) and tourniquet width, among others. Several authors have tried to establish formulas to aid in the calculation of this value, often based on brachial systolic blood pressure. Diamond et al.(33) established the formula: (systolic blood pressure x 1.5) + age as the minimum occlusion value. Massey et al. (34) studied various predictive factors to determine arterial occlusion pressure in the foot using an ankle tourniquet and using various physiological and anthropometric variables of the participants; their final regression equation was: (116 x ankle/brachial index) + (1.37 x systolic blood pressure) -159. Tuncalli et al. developed the concept of arterial occlusion pressure using the following formula [systolic blood pressure + 10]/tissue damping coefficient. (35,36) On the other hand, McEwev et al. noted that the LOP value can vary widely with respect to systolic blood pressure measured in the arm and that this variability suggests that calculating tourniquet pressure using only systolic blood pressure in the patient’s arm may not be optimal in many cases.(14) In the present study, no differences were found in systolic blood pressure among the different groups of surgical field quality: Excellent, Good, and Regular; although a greater dispersion of data was observed in the Regular group with respect to the Good group and between these two (Regular and Good) with respect to the Excellent group, as shown by the values of the standard deviation of brachial systolic blood pressure (Table 3). This aspect is also reflected in the dispersion of the final pressure used according to the data from the confidence intervals (Table 3).
One aspect to note in the present study is the use of conscious sedation in all patients by an anesthesiologist. Regardless of whether blood pressure measured in the arm is relevant to the calculation of the LOP value, it should remain stationary throughout the entire surgical procedure with minimal variations. The fact that the patient was constantly monitored and under conscious sedation by the anesthesiologist helped maintain a stable level of blood pressure during the surgical procedure in all the study patients. In this regard, the results obtained in the present study should be viewed in the context of constant blood pressure monitoring and may not be applicable to other studies that did not have close monitoring of the patient’s blood pressure during the intraoperative period.
Apart from preventing pressure-related injuries, there is another relevant aspect regarding the use of tourniquets that speaks od the presence of intraoperative pain caused by the tourniquet, which tends to increase with the duration of its use.(37) This is an important aspect, as it allows surgery to be performed safely and comfortably for the patient with distal nerve blocks and IV sedation without need for general anesthesia or more proximal blocks (popliteal or spinal). Finsen and Kasseth(38) concluded that the use of ankle tourniquets is better tolerated by patients than when they are used on the leg. It is the subjective opinion of the authors of this article that the use of lower tourniquet pressures, along with the use of IV sedation, delays the onset of tourniquet-associated pain during the surgical procedure. Unfortunately, this aspect was not studied in the present work, and future studies would be needed to test this hypothesis.
The immediate period just after exsanguination of the limb and deflation of the tourniquet potentially carries a risk of creating hemodynamic instability to the patient. Tourniquet deflation produces systemic cardiovascular, hematological, respiratory, and metabolic effects due to the residues originating in the tissue once ischemia is removed and passes into the central circulation. (39,40) Similarly, there is a risk of creating embolization phenomena just after the deflation of the extremity tourniquet, which have been clearly reported in the literature. (41,42,43,44) In the present study, all patients were closely monitored, and none suffered any cardiovascular or respiratory events in the immediate intraoperative and postoperative periods with the inflation and deflation of the tourniquet. In this regard, we should mention that most of these events have been reported with tourniquets in more proximal locations such as the thigh, where there is a larger volume of blood exsanguination and deflation, and a greater amount of exposed ischemic tissue, especially muscular, compared to the use of the tourniquet at the ankle, where the only anatomical area exsanguinated is the foot. In fact, a recent study in patients undergoing hallux valgus/limitus surgery with the use of a thigh tourniquet showed that the most significant ischemic changes occurred in muscular tissue, not in subcutaneous or bone tissues. (45) For all these reasons, we consider ankle location to be very safe in terms of systemic cardiovascular, respiratory, and metabolic effects.
The present study has certain limitations, so the interpretation of the results should be approached with caution. Firstly, the assessment of surgical field quality was done subjectively by grading it into 4 values (Excellent, Good, Regular, and Poor). Although this measurement has been used in previous studies,(14,16,36) there is inherent subjectivity to this assessment that may have interfered with the results obtained. Secondly, the LOP measurement method takes time in the operating room and requires certain skills and practices from the operator in charge to be precise. Therefore, it is a method that is rarely used in the routine clinical practice, and we believe these aspects could be a limitation to expanding its use routinely in clinical practice in foot surgery.
In conclusion, the present study has determined the quality of the surgical field using a method for quantifying tourniquet pressure (LOP method) when the location is at the ankle in forefoot surgery. The mean pressure used by the tourniquet in the present study was 192.73 ± 31.73 mm Hg, which represents pressures lower than those historically used at the ankle as standard for foot surgery. The quality of the surgical field was considered Excellent or Good in 94.8% of cases. Calculating tourniquet pressure at the ankle using the LOP method adding a safety margin is a valid and reliable method that yields excellent and good surgical field quality in most cases and with minimal complications. The authors believe that the pressure calculation method should be done on an individual basis, and the routine use of a constant pressure of 250 mm Hg in all cases should be avoided.
Ethical statement
This study was conducted after being approved by the center’s management and following all the recommendations of the Declaration of Helsinki, and after informed consent from all participants was obtained after a verbal explanation of the project. While this study was being conducted, it did not alter, exceed, or change in any way the usual or routine clinical practice for this type of patients in the health care center where it was conducted, so no approval was sought from a central committee for clinical research ethics.
Conflicts of interest
None declared.
Funding
None declared.
Authors’ contributions
Conception and study design: JPH, LPF, LTV.
Data collection: JPH, LPF, LTV, EME.
Result analysis and interpretation: JPH, AGF.
Creation, drafting, and preparation of the initial draft of the paper: JPH, AGF, EME.
Review and final acceptance: JPH, LPF, LTV, AGF, EME.
References