
DOI: 10.20986/revesppod.2022.1634/2022
ORIGINAL
A new modification of the Winograd technique for the treatment
of ingrown toenail
Una nueva modificación de la técnica Winograd para el tratamiento de la uña encarnada
Flávio Oliveira1, Joaquín Óscar Izquierdo Cases2, António Silva Santos3, Sofia Ramos4 y Guillermo Lafuente Sotillos5
1Servicio de Podologia. Escola Superior de Saúde Cruz Vermelha Portuguesa. Braga, Portugal. 2Unidad de Cirugía Avanzada de Pie y Tobillo. Centro Clínico Quirúrgico Aranjuez, Madrid, España. 3Instituto Superior de Tecnologias Avançadas de Lisboa (ISTEC-Lisboa). Lisboa, Portugal. 4Universidade Lusófona. Lisboa, Portugal. 5Departamento de Podología. Universidad de Sevilla, España
Abstract
Introduction: Ingrown toenails are one of the most common nail pathologies, being the main reason for consultations for nail pain. The Winograd technique, commonly known as wedge excision, is one of the most used techniques due to the low rate of recurrences and overall patient satisfaction. We consider it possible to mitigate some possible disadvantages, reducing the already low risk of infection, as well as the risk of onycholysis, by modifying the incisional approach and using only adhesive approximation strips. The objective of this work is to proves the effectiveness of the modification of the original Winograd technique for the treatment of ingrown toenail.
Patients and methods: A retrospective study, with a sample of 111 patients and 159 digits were operated on between 2003 and 2019 in clinics in Vila Nova de Famalicão, Viana do Castelo and Lisboa (Portugal), with a follow-up period of more than 15 years. Data on: a) postoperative complications, b) the time elapsed to wound healing, c) the rate of recurrences, and d) general patient satisfaction were collected.
Results: The results revealed 1.8 % of heavy bleeding, 3.6 % of postoperative complications, 2.70 % of recurrences and 8.10 ± 0.76 of wound healing days. Patients reported very low postoperative pain (0.9 %) and high satisfaction results (99.1 % for the functional result; 94.6 % for the aesthetic result and 97.3% for patient satisfaction).
Conclusions: The modifications performed have better results than those reported with the conventional technique, in terms of recurrence, average period of time from surgery to wound healing and return to daily activities and general patient satisfaction, suggesting its safe current use in clinical practice for the treatment of grades II and III ingrown toenail.
Keywords: Ingrown toenail, patient satisfaction, recurrence, wound healing, wedge resection.
Resumen
Introducción: Las uñas encarnadas son una de las patologías ungueales más frecuentes y puede utilizarse la técnica de Winograd, entre otras, para su tratamiento quirúrgico. Propusimos reducir el riesgo de infección, onicolisis y tiempo de cicatrización, modificando el abordaje incisional y utilizando tiras adhesivas de aproximación. El objetivo de este trabajo es probar la efectividad de la modificación de la técnica original de Winograd para el tratamiento de la uña encarnada.
Pacientes y métodos: Se trata de un estudio retrospectivo, con una muestra de 111 pacientes y 159 dedos operados entre 2003 y 2019 en clínicas de Vila Nova de Famalicão, Viana do Castelo y Lisboa (Portugal), con un seguimiento de más de 15 años. Se recogieron datos sobre: a) complicaciones postoperatorias, b) el tiempo transcurrido hasta la curación total, c) la tasa de recurrencias y d) la satisfacción general del paciente.
Resultados: Los resultados revelaron 1.8 % de sangrado abundante, 3.6 % de complicaciones postoperatorias, 2.70 % de recurrencias y 8.10 ± 0.76 de días de curación total. Los pacientes reportaron dolor postoperatorio muy bajo (0.9 %) y un grado de satisfacción muy alto (99.1 % satisfacción muy alta para resultado funcional, 94.6 % para el resultado estético y 97.3 % para la satisfacción global del paciente).
Conclusiones: Las modificaciones realizadas tienen mejores resultados que los reportados con la técnica convencional en cuanto a la tasa de infección, tiempo de cicatrización y satisfacción general del paciente, lo que sugiere su uso actual seguro en la práctica clínica para el tratamiento de la uña encarnada grados II y III.
Palabras clave: Uña encarnada, satisfacción del paciente, recurrencias, curación total, resección en cuña.
Received: 23-03-2022
Accepted: 10-11-2022
Correspondence: Flávio Oliveira
investigacao.podiat@gmail.com
INTRODUCTION
Ingrown toenails are one of the most common and painful nail problems, with symptoms ranging from swelling and inflammation to infection, and medical care is often sought for this condition1. The nail plate traumatizes the nail canal and invades the surrounding soft tissue, leading to infection in some cases, potentiating granulation tissue formation2-4. There is a vicious and recurrent cycle of swelling, pain and infection, which considerably affects morbidity, and absenteeism from work is common as a consequence of this condition5-7.
For many years the severity of ingrown toenail was classified into three stages according to Heifetz8, defining as stage 1 a slight erythema and swelling of the nail grooves in the nail bed, stage 2 in a presence of acute infection and suppuration, and stage 3 when present a chronic infection, with the formation of granulation tissue surrounding the nail groove and hypertrophy of the surrounding tissues8. The number of stages was progressively increased to highlight the level of inflammation of the nail canal9, or the chronicity of the deformity of the nail structure10. More recently, Kline11 developed a new classification system with five stages of severity, from I or mild, when presents a local irritation of the nail fold, with good nail attachment, and without signs of drainage or granulation tissue at the edge of the nail; II or inflammation, with nail border more inflamed and drainage, pus and granulation tissue; III or infection, with exacerbation of symptoms and the presence of pus and granulation tissue, but without onycholysis; IV or infection with onycholysis of a single nail border, with granulation tissue and drainage; V or infection with onycholysis of both nail borders and even the nail plate.
The most common causes of this pathology are biomechanical changes, pathological nail plate curvatures, incorrect cutting, etc.7,12,13. In general, patients seek treatment when this condition becomes symptomatic14. Treatment will depend on the severity of the problem and can range from conservative treatment in less severe cases to the use of surgery in relapsing and more severe cases. Surgical treatment is more effective and shows better results in a very significant way compared to conservative treatments3,14.
The Winograd technique is one of the most used surgical techniques in Kline stage II and III ingrown toenail2-3,12. It is often used when the nail fold is hypertrophic and needs to be excised15. Its advantages are the low level of recurrences, control of the amount of tissue removed, painless postoperative period, reduced healing time, and good aesthetic and functional results, with good overall patient satisfaction16,17. The disadvantages of this technique are that it is difficult to perform compared to chemical matrixectomy, it needs more specific equipment, it requires wound healing by first intention, and it may delay return into activities of daily living due to possible suture infection16,17.
Some authors reporting on this technique, have presented recurrence rates of 12 %2,12, an average postoperative infection rate of 10 %12, and a high degree of functional and aesthetic patient satisfaction, both above 90 %, as verified by large-scale studies12 18,19.
To mitigate some problems related to its disadvantages, an approach was developed that suggests two modifications to the originally described technique20. The first is to abolish detachment of the nail plate and to make direct incisions in the biological material to be extirpated. The second, to decrease the infectious potential of the sutures by completely replacing them with adhesive approximation strips, which also promote primary closure of the incision, without invading the tissues and without risk of damaging the nail matrix.
In the present study, we intend to analyze the modified Winograd technique in terms of a) postoperative complications, b) time elapsed until wound healing, c) symptomatic recurrence rate, d) overall patient satisfaction. Likewise, we intend to study whether this technique can be used to mitigate the weaknesses of the conventional Winograd technique by comparing these data with those reported by other authors.
PATIENTS AND METHODS
Study population
An initial sample of 261 patients who underwent intervention with the Winograd technique between February 2003 and September 2019 in clinics in Vila Nova de Famalicão, Viana do Castelo and Lisbon, in Portugal was collected. Sixty-one patients were excluded because it was not possible to contact them to answer the questionnaire about the surgical outcome. Of the 200 patients, it was decided to take a representative sample, using a random probability cluster with an error of 5 % for a confidence level of 95 %. The selected sample of this retrospective study includes 111 patients (66 [59.46 %] females and 45 [40.54 %] males), with mean patients age of 39.86 ± 18.49 (range to 12 to 80) years.
All patients who gave informed consent for surgery and research study, were fully mentally and physically able, had a diagnosis of ingrown toenail grades II or III, according to Kline’s classification11, had the complete quantification of the variables in the clinical process and that answered the entire questionnaire were included11. On the other hand, patients with bone lesions, cystic lesions, or any other condition that could interfere with the application of the technique; pregnant or lactating women; patients who did not respect the indicated postoperative dressing schedule; patients with connective tissue pathologies or with a history of pathological healing, either atrophic or hypertrophic were excluded.
Surgical technique
The foot was prepared with a previous washing with a chlorohexidine sponge, subsequently emulsified with povidone-iodine and local anesthesia of the hallux was performed using the Frost H technique with 3 % Mepivacaine Hydrochloride. Hemostasis was performed with an ischemic ring or Smarch strap, and the periungual hypertrophic soft tissue to be removed was evaluated, using a sterile surgical field.
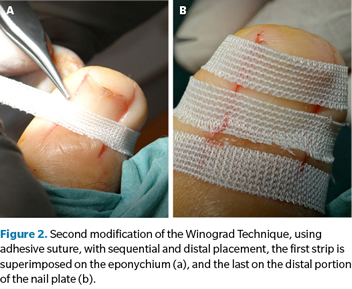
The first modification was performed at the time of incision. Instead of detaching the nail plate, three incisions were made: 1) a first dorsal incision with a No 15 scalpel blade (Figure 1a and 1b), in a posteroanterior direction, from the posterior eponychium to the distal eponychium. It was essentially a marking incision that was oriented yet not deep; 2) a second incision made with the cutting bevel of the blade oriented dorsally (Figure 1c), in anteroposterior direction with the first incision, in depth relative to surface area to be excised, from the hyponychium to the cortex of the dorsal base of the distal phalanx; 3) a third parabolic incision (Figure 1d), from the proximal eponychium to the hyponychium, this being the only incision common with the conventional Winograd technique. The third incision was performed with the bevel of the scalpel blade in plantar orientation with an oblique deviation towards the second incision, connecting the two incisions in depth. At the end of these three incisions, we were able to excise the anatomical piece, consisting of a portion of nail matrix and lamina, portion of nail bed, granulation and/or fibrous tissue, and some residual adipose tissue.

After the tissue was excised, the second modification was to apply adhesive strips to approximate the incisions (Figure 2a), the first adhesive strip was placed distally to the eponychium (Figure 2a), the second in the posterior eponychium, and the third in the distal portion of the nail plate (Figure 2b). All were applied with spaces of about two millimeters between them to allow normal drainage of these incisions (Figure 2b), without over lapping to prevent over constriction in the plantar area of the digit, regarding possible edema of the toe. The strips were covered with non-sticky dressing, replaced every 48 hours and at eighth day the patients returned to all normal activity.
In the postoperative period, patients were advised to keep their feet elevated (at the level of the pelvic girdle), to walk for five minutes every hour from 12 hours after intervention, to wear postoperative footwear and not to remove or wet the dressing and that these procedures should only be carried out in a controlled environment, i.e. a clinical one. From the first dressing change, amount of bleeding, inflammation, infection, or any other note of particular interest was assessed. After total recovery, three follow-up visits were carried out, at six months, one and two years.
Variables
To evaluate the modifications of Winograd’s technique the following variables were defined:
A Visual Analog Scale was used to assess postoperative pain level, which was considered relevant if it was ≥ 7. For the functional outcome, the ability to wear shoes, to practice physical activity, to support the foot on the floor without pain or discomfort in the treated toe was evaluated. For the aesthetic result, the maintenance of the width and color of the nail was evaluated, as well as the appearance of the scar on the treated finger. Finally, global satisfaction assesses the entire treatment process and outcomes perceived by the patient. A classification ≥ 9 was considered very satisfactory for these outcomes. A percentage of relevant outcomes were presented.
Statistical analysis
Over the course of more than 15 years we performed interventions with the Winograd technique on all patients in the sample, analyzing bleeding, postoperative complications, time to wound healing and number of recurrences with their respective symptoms. Except for mean time to wound healing, a continuous variable that requires mean and standard deviation, the remaining categorical variables were analyzed and relative and absolute frequencies were calculated. Overall patient satisfaction was calculated using the median and interquartile range, from the percentual rating scale coming from the questionnaire distributed after wound healing. Patients who had already completed recovery before the beginning of this research study were contacted by phone and asked to fill out the questionnaire in person or via e-mail. All data were statistically treated using SPSS 25.0 software (IBM SPSS Statistics for Windows, version 25.0. Armonk, NY: IBM Corp).
RESULTS
A total of 111 patients and 159 toes were operated on, 42 (27.03 %) were operated on the right hallux, 47 (29.73 %) on the left hallux, and the remaining 70 (43.24 %) were operated bilaterally (both big toes). Of the 78 left hallux procedures, two (2.56 %) involved the tibial lateral, five (6.41 %) the fibular lateral and the remaining 71 (91.03 %) both borders, whereas of the 81 right hallux procedures, three (3.40 %) involved the tibial lateral, six (7.41 %) the fibular lateral and the remaining 72 (88.89 %) both borders.
Regarding surgical history of the toes, 18 (16.22 %) had undergone previous surgery on which there was a high need for reoperation. Twelve patients had undergone total temporary nail removal, two had nail fold plasty, two had undergone partial matrixectomy without nail fold plasty, and finally two had undergone partial matrixectomy with nail fold plasty.
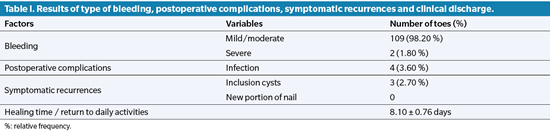
Clinical results showed low index of abundant bleeding (1.80 %), low index of infection rate (3.60 %) as postoperative complications, low recurrence rate (2.70 %) and a short wound healing time (8.10 ± 0.76 days) (Table I).
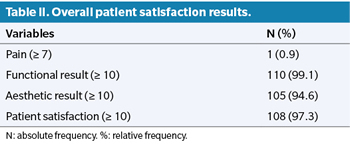
Regarding overall patient satisfaction, a very low postoperative pain and high functional and aesthetic outcomes, as well as high patient satisfaction were recorded (Table II).
DISCUSSION
Ingrown toenail is a common factor of morbidity, with an impact on work absenteeism and on the quality of life of the individual. When conservative therapies do not solve the problem, surgical procedures must be used, and the Winograd technique or wedge excision is one of the most common. This study aims to prove the effectiveness of a variation of the original Winograd technique for the treatment of ingrown toenail, mitigating some postoperative and recurrence complications, increasing overall patient satisfaction, and decreasing recovery time. These modifications, in incisional approach and adopting adhesive approximation strips, are easy to perform from the technical point of view.
In terms of bleeding, in 98.20 % of the cases it was mild or moderate and in 1.80 % it was severe. As for postoperative complications, 3.60 % showed signs of infection. Recent studies using the conventional Winograd technique reveal signs of infection in 7.69 %12, 6.89 %21 and 3.2 %22 and edema in 3.08 % of patients12. Considering infection as a postoperative complication, the modifications presented do not increase this rate, remaining in agreement with other studies.
Recurrence rates vary widely between studies and are directly related to the follow-up time. For a one-year follow-up, Khan, and Kumar21, who performed 29 interventions, recorded 10.34 % recurrence rate requiring a second intervention, Kose et al.23, with 75 interventions, had 13.2 % recurrences, and Acar24, with 50 interventions, found 6 % recurrence rate. Recurrence, however, developed in 3.2 % of 39 cases Huang et al.22 and in 9.4 % of 85 cases in Guler et al.19, both with a follow-up of about 15 months. In the present study, with a retrospective follow-up period of more than 15 years, we only recorded 2.7 % recurrence rate, all with inclusion cysts, resulted in a relevant reduction compared to the other studies, suggesting that the modification of incision approach could be more effective.
The mean time from surgery to wound healing is another element to consider when choosing a procedure, since the longer the healing time interval, the less effective the treatment becomes and the higher the risk of inflammation, infection and recurrence. Huang et al.22, with 39 procedures using the Winograd technique, showed mean wound healing time of 2.8 ± 1.2 weeks. Guler et al.19 reported 13.8 ± 2.26 days until return to daily activities, similar to Ali et al.12 and Acar24, who reported a mean of 13.62 and 10 days, respectively. Also, in this case, the mean wound healing time decreased, with about 8.10 ± 0.76 days, which may be due to the type of closure used, without the need for invasive suture.
Regarding overall patient satisfaction, Kose et al.23 reported that 97 % of patients were satisfied with the treatment, although 2.67 % had complaints of intermittent postoperative pain and 2.67 % rated the esthetic result as poor, due to scar and nail narrowing, 91.18 % rated it as excellent and 5.88% as average. Huang et al.22 and Ali et al.12 showed 5.26 % and 7.69 % of complaints due to the aesthetic result, although the overall satisfaction was 92.6 % and 92.30 %, respectively, similar Acar24, with 92.0 %. The level of satisfaction in Guler et al.19 was more modest, with 82.4 %, and in Khan and Kumar21, with 69.56 %, with complaints regarding the esthetic appearance remaining. The modifications proposed presented 0.9 % of postoperative pain, 99.1 % for functional outcome, 94.6 % for aesthetic outcome, and 97.3 % for patient satisfaction. Comparing with outcomes presented for conventional Winograd technique, modifications tested showed better overall patients satisfaction.
This study has limitations, starting with the fact that it is a retrospective study. Another limitation was that we were not able to sensitively quantify possible variations in opinion between the time of surgery and the questionnaire results. Although we had clear answers and expressive values in the variables assessed by the questionnaire, it should have been presented to the patient at the time of surgery, and the results of the data should have been interpreted there. It was also not possible to determine in which interventions tourniquet digital ring or Smarch strap hemostasis were applied, and whether they would alter the results of our variables. Finally, we believe that it is a limitation of the study that we did not include a sample of patients operated with the original Winograd technique performed by the same surgeon, in order to be able to compare the results by always controlling the postoperative and other intraoperative parameters in the same way.
In conclusion, Winograd’s technique for ingrown toenail results in high satisfaction rates, low recurrence rates, and low complication rates. The changes presented here in incision and suture have been shown to have better outcomes in terms of recurrences, healing time, and overall patient satisfaction compared to data reported by other authors. More studies are needed to determine the effectiveness of these modifications to the Winograd technique, and a long-term, prospective design for the same variables would raise the level of scientific evidence.
CONFLICTS OF INTEREST
The authors registered no conflicts of interest.
FINANCIAL DISCLOSURE
None reported.
ETHICAL DECLARATION
All procedures were performed with informed consent, with approval from the Ethics Committee of the University Institute of Health Sciences – CESPU, registered with 35/CE-IUCS/2020, according to the Helsinki declaration.
REFERENCES