DOI: http://dx.doi.org/10.20986/revesppod.2023.1660/2023
ORIGINAL
Thermography of the vasodilator effect of local anaesthetics
in ingrown toenail surgery
Termografía en el efecto vasodilatador de anestésicos locales para el bloqueo troncular
del primer dedo
Ana Belén López Gómez1, Jonatan García Campos2, Alfonso Martínez Nova1
1Universidad de Extremadura. Cáceres, España
2Facultad de Medicina. Universidad Miguel Hernández. Elche, Alicante, España
Abstract
Objectives: Local anaesthetics such as lidocaine or mepivacaine, commonly used in toenail surgery, have an associated vasodilator effect. Although is thought that lidocaine has a greater vasodilator effect than mepivacaine, there´s not strong in vivo evidence of this. So, the aim of this work was to assess the temperature increase experienced by the toes after be injected of 1 ml 2 % mepivacaine or lidocaine.
Patients and methods: 26 participants were randomly divided into two groups and a pre-anæsthetic thermal image (Flir E60bx camera) was taken. Patients in group A (n = 13) received 1 ml of 2 % lidocaine, while those in group B (n = 13) received 1 ml of 2 % mepivacaine at four points of the hallux. After 10 minutes a second thermal image (post-anæsthetic image). Mean temperatures were assessed at the proximal phalanx and the pad of the hallux.
Results: After application of the anæsthetic, the mean temperatures were 31.3 ± 3.07 °C at point 1 and 30.8 ± 3.08 °C at point 2 in the lidocaine group, and 31.3 ± 2.74 °C at point 1 and 29.5 ± 2.87 °C at point 2 in the mepivacaine group, with not statistically significant differences between them (p = 0.959 and p = 0.798). All the participants experienced temperature increases of between 5.13 °C and 6.91 °C, but there were no significant differences between groups (p = 0.7 and p = 0.0778).
Conclusions: Even though most of the literature suggests that lidocaine has more potent vasodilator effect than mepivacaine, the present results do not reflect any real clinical impact distinguishing one drug from the other in the field block of the big toe, as measured with infrared thermal imaging.
Keywords: Trunk anesthesia, ingrown toenail, lidocaine, mepivacaine, vasodilation.
Resumen
Objetivos: Los anestésicos locales de tipo amida empleados en cirugía podológica, como la lidocaína o mepivacaína, poseen cierto poder vasodilatador. Puesto que en algunas técnicas quirúrgicas puede haber sangrado postquirúrgico abundante, conocer si alguno de los dos anestésicos tiene mayor o menor efecto vasodilatador podría mejorar la respuesta postquirúrgica a estas técnicas. Así pues, el objetivo de este estudio fue comparar la respuesta térmica en el primer dedo tras la aplicación de los dos anestésicos al 2 %.
Pacientes y métodos: Veintiséis participantes sanos se ofrecieron voluntarios para participar en este ensayo clínico aleatorizado con doble ciego. Los sujetos fueron divididos en dos grupos: lidocaína 2 % (n = 13) y mepivacaína 2 % (n = 13). Ambos grupos recibieron 1 cc del anestésico indicado. Se realizó una fotografía termográfica previa y tras 10 minutos al bloqueo troncular del hallux para cuantificar el aumento de temperatura. No se registraron complicaciones ni reacciones adversas.
Resultados: Los dos grupos eran similares en cuanto a características antropométricas. No se observaron diferencias significativas entre grupos ni en la media de temperatura pre-anestésica (24.38 °C grupo lidocaína, 24.75 °C grupo mepivacaína, p = 0.918), ni en la media de temperatura postanestésica de los sujetos (31.3 °C para ambos grupos, p = 0.959). Los resultados de la diferencia pre-post anestésica fue de 6.91 °C para el grupo lidocaína y de 6.54 °C para el grupo mepivacaína, siendo esta diferencia estadísticamente no significativa (p = 0.7). Sin embargo, todos los sujetos (n = 26) mostraron un aumento de la temperatura tras la anestesia (p < 0.001).
Conclusiones: Ambos fármacos mostraron una elevación de la temperatura en los sujetos y, por tanto, su poder vasoactivo. En cambio, no se evidenciaron diferencias significativas entre grupos. Así bien, el efecto vasodilatador de la lidocaína al 2 % y la mepivacaína al 2 % fue similar entre sí y, por lo tanto, no se evidencia que exista un potencial beneficio del uso de uno en relación con las posibles hemorragias postquirúrgicas.
Palabras clave: Anestesia troncular, uña incarnada, lidocaína, mepivacaína, vasodilatación
Received: 27-04-2023
Accepted: 26-05-2023
Correspondence: Alfonso Martínez Nova
podoalf@unex.es
Introduction
Local Anæsthetics such as lidocaine or mepivacaine, commonly used in toenail surgery, have an associated vasodilator effect. Although concentrations of 1:100,000 epinephrine in 2 % mepivacaine solutions have been shown to be safe in patients without vascular risk1, the need for additional use of ischæmia bands or rings means that they are not commonly used to perform nail surgery. Incisional techniques such as Suppan, Frost, or Winograd present some post-surgical bleeding, often abundant, due to reactive hyperæmia after removing the tourniquet ischæmia1, which should not exceed 20 minutes2. Some studies have established that lidocaine has a greater vasodilator effect than mepivacaine3, although it has not been clinically evaluated for distal zones. If a lesser vasodilator effect were demonstrated for mepivacaine, it could be the chosen anæsthetic to avoid excessive bleeding. This potential vasodilator effect may be indirectly reflected in the temperature increase experienced by the toe, an increase which could be measured by infrared thermography4. Thus, the objective of this study was to evaluate the differences in the thermal response in the big toe after the application of 1 ml of either 2 % lidocaine or 2 % mepivacaine, a response which could be related to the two drugs vasodilator potential.
Patients and methods
This study was designed as a double-blind randomized clinical trial, with a sample of convenience of 26 participants (18 woman and 8 men; age 21.8 ± 2.2 years, weight 65.8 ± 12.4 kg, height 168.7 ± 9.4 cm) being selected. The inclusion criteria were 1) participants with not systemic, cardiovascular, or circulatory disorders and 2) no allergy to local anæsthesia. Subjects that 1) had not previously been infiltrated with lidocaine or mepivacaine were excluded and were unaware of a possible allergic reaction. All participants signed an informed consent. The participants were randomly divided into two groups, going to one of two adjoining rooms with identical environmental conditions (temperature 24 °C and ambient humidity 45 %). A thermal image (Flir E60bx thermal imaging camera, Flir systems) was taken of the foot that was to be anæsthetized (pre-anæsthetic image). The principal investigator (A.M.N.) prepared the anæsthetic solutions, being the only one who knew the type of anæsthetic that was infiltrated in each room. All the anæsthetic procedures were performed by the same professional (first author: A.B.L.G.) to follow the same protocol and avoid bias. Patients in group A (n = 13) received 1 ml of 2 % lidocaine, while those in group B (n = 13) received 1 ml of 2 % mepivacaine. The choice of the foot to be anæsthetized was random. In both groups, the anæsthetic technique used was a trunk block at four points of the hallux, depositing 0.25 ml in each of the plantar and the dorsal areas of the peroneal and the tibial canals. After injection of the anæsthetic, 10 minutes were allowed to pass, and a second thermal image (post-anæsthetic image) was taken in accordance with the protocol described above. This time allowed the correct diffusion of the anesthetic and was a sufficient latency period for both anesthetics (mepivacaine 2-4 minutes and lidocaine 1-3 minutes). Mean temperatures were recorded in two areas – the proximal phalanx (Zone 1) and the pad of the Hallux (Zone 2, Figure 1).
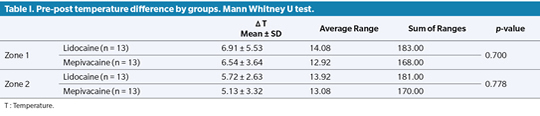
Statistical analysis was performed with the SPSS Statistics 25 software. Due to the limited sample size available, a Shapiro-Wilk test was performed to check for normality of the data distribution. Since the p values were less than 0.05, nonparametric (Mann-Whitney U) tests were performed. Values of p≤0.05 were considered statistically significant.
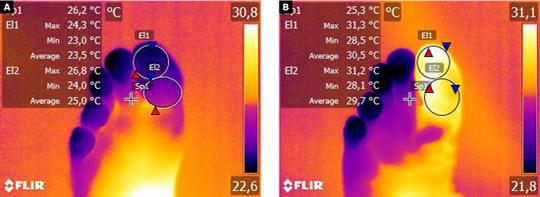
Figure 1. Pre- (A) and post- (B) anæsthetic thermal images. Zone 1: proximal phalanx of the big toe. Zone 2: pad of the hallux.
Results
The mean temperature prior to application of the anæsthetic was 24.38 ± 4.17 °C at point 1 and 25.13 ± 3.83 °C at point 2 in the group anæsthetized with lidocaine. In the mepivacaine group, the corresponding mean pre-anæsthetic temperatures were 24.75 ± 3.94 °C at point 1 and 26.11 ± 3.86 °C at point 2. For neither zone were the temperatures significantly different between the two groups (p = 0.918 and p = 0.920). After application of the anæsthetic, the mean temperatures were 31.3 ± 3.07 °C at point 1 and 30.8 ± 3.08 °C at point 2 in the lidocaine group, and 31.3 ± 2.74 °C at point 1 and 29.5 ± 2.87 °C at point 2 in the mepivacaine group. Again, there were no statistically significant differences between the two groups (p = 0.959 and p = 0.798).
All the participants experienced temperature increases (Δ) of between 5.13 °C and 6.91 °C, but there were no significant differences in these increases between the two groups (p = 0.7 and p = 0.0778 for points 1 and 2, respectively, Table I).
Discussion
Our results indicate that both lidocaine and mepivacaine at 2 % cause similar increases in local temperature after anæsthetic injection in the hallux, and it could not be demonstrated that one anæsthetic had a more marked vasodilator effect than the other. This contrasts with what was reported by Trepal & Jules5 in a review on local anæsthetics (LAs) in podiatric surgery in which the authors noted the similarities between the two drugs in terms of onset of action and duration, but also highlighted that while vasodilation associated with lidocaine is moderate that associated with mepivacaine is only mild. Similarly, in a meta-analysis done by Su et al.3, in comparing the efficacy and safety of the two drugs, the authors conclude that mepivacaine is just as potent anæsthetically as lidocaine but has a milder vasodilator capacity. Contrary findings were reported by Sung et al.6 in an in vitro study aimed at determining the vasoconstriction induced by different LAs of the amide group, including lidocaine and mepivacaine, with the order of vasoconstrictor potency being levobupivacaine > ropivacaine > lidocaine > mepivacaine. In this case, therefore, mepivacaine was found to be more vasoactive than lidocaine. Even though most of the literature suggests that lidocaine is slightly more vasodilatory than mepivacaine, the present results do not reflect any real clinical impact distinguishing one drug from the other in the field block of the big toe, as measured with infrared thermal imaging.
This study present some limitations, the main one being the small sample size. Maybe with a wider sample the results could take another direction and detect some differences.
In conclusion, both drugs, mepivacaine and lidocaine, showed a temperature increase of around 6ºC in all subjects, and therefore demonstrated their vasoactive power. Nevertheless, there was no evidence that there exists any potential benefit of using one or other in relation to avoiding possible post-surgical bleeding.
Ethics Declaration
The execution of this research process was approved by the Bioethics and Biosafety Committee of the UEX (Id: 54//2021).
Conflict of interest
The authors declare that they have no conflict of interest relevant to the conduct of this study.
Funding
None.
References
- Diz Mellado C, Rayo R, De Francisco F, Martínez-Nova A. Effect of Anesthesia With or Without a Vasoconstrictor in Mechanical Matricectomy. Dermatol Surg. 2019;45(12):1735-8. DOI: 10.1097/DSS.0000000000001886.
- Becerro De Bengoa Vallejo R, López López D, Losa Iglesias ME, Sanchez Gomez R, Palomo López P, Morales Ponce A, et al. Effects of tourniquet ischaemia and time safety in toe surgery. J Eur Acad Dermatol Venereol. 2015;29(7):1442-3. DOI: 10.1111/jdv.12487.
- Su N, Liu Y, Yang X, Shi Z, Huang Y. Efficacy and safety of mepivacaine compared with lidocaine in local anaesthesia in dentistry: a meta-analysis of randomised controlled trials. Int Dent J. 2014;64(2):96-107. DOI: 10.1111/idj.12087.
- Gatt A, Formosa C, Cassar K, Camilleri KP, Raffaele C De, Mizzi A, et al. Thermographic Patterns of the Upper and Lower Limbs: Baseline Data. Int J Vasc Med. 2015;2015(831369). DOI: 10.1155/2015/831369.
- Trepal MJ, Jules KT. Anestésicos locales en cirugía podológica. Local anesthetics in podiatric surgery. Rev Int Ciencias Podol. 2007;1(1):49-74.
- Sung H, Ok S, Sohn J, Son YH, Kim JK, Lee SH, et al. Vasoconstriction Potency Induced by Aminoamide Local Anesthetics Correlates with Lipid Solubility. J Biomed Biotechnol. 2012;2012:170958. DOI: 10.1155/2012/170958.