DOI: http://dx.doi.org/10.20986/revesppod.2024.1715/2024
UPDATES
Adaptation of Mueller and Maluf’s biomechanical paradigm to the physiology of stress in the overload lesion
Adaptación del paradigma biomecánico de Mueller y Maluf a la fisiología del esfuerzo en la lesión por sobrecarga
Fernando Pifarré San Agustin1
Valldeflors Pifarré Prats2
Xavier Ortas Deunosajut3
Carles Escalona Marfil3
Óscar Hernández Gervilla3
1Departamento de Presidència. Generalitat de Catalunya Centro de Medicina Deportiva. Lleida, España
2Servicio de Cirurgía. Hospital Universitarrio Arnau de Vilanova. Lleida, España
3Departamento de Podología. Universitat de Vic-Universitat Central de Catalunya. Manresa, Barcelona, España
Abstract
Biomechanical paradigms are theoretical and practical instruments that help us interpret, diagnose, and treat certain disorders of the musculoskeletal system, especially of the lower limbs. For some, they are scientific theories because they describe a working methodology, establish certain laws or theoretical principles, utilise measuring instruments and necessary techniques to make the paradigm’s laws applicable to the real world, and provide very general metaphysical principles that guide our work within the paradigm. The present paper is doing a correlation between phisiology of sports medicine and different biomechanical paradigms that explain overuse injuries. The paper reviews phisilogical parameters such us aerobic potency, aerobic threshold, anaerobic threshold and percentage of oxigen exploitation and how this measurements can be related with different overuse injuries in the lower limbs explained under the view of the Mueller and Maluf (physical stress theory). Finally, a rehabilitation protocol is outlined based in the functional recovery of patients with overuse injuries following the principles of physical stress paradigm that can be monitored by the physiology measurements explained in the paper.
Keywords: Overload injury, oxygen consumption, biomechanical paradigm, aerobic threshold, sport physiology, muscle
Resumen
Los paradigmas biomecánicos son instrumentos teórico prácticos que nos ayudan a interpretar, diagnosticar y tratar algunas alteraciones del aparato locomotor, especialmente de las extremidades inferiores. Para algunos son teorías científicas, ya que describen una metodología de trabajo, establecen unas leyes o principios teóricos, utilizan un instrumental de medición y técnicas necesarias para hacer que las leyes del paradigma se refieran al mundo real, y nos aportan unos principios metafísicos muy generales que guían nuestro trabajo dentro del paradigma. El presente trabajo pretende correlacionar el mundo de la fisiología del ejercicio con diferentes paradigmas biomecánicos que explican las lesiones por sobreesfuerzo, especialmente en el tejido muscular. Se repasan los parámetros fisiológicos de potencia aeróbica, umbral aeróbico y anaeróbico y porcentaje de aprovechamiento de oxígeno y cómo estos valores pueden estar relacionados con diferentes lesiones por sobreesfuerzo en los miembros inferiores explicadas según el modelo de Mueller y Maluf (teoría de estrés físico). Finalmente, se plantea un modo de rehabilitación concreto basado en la recuperación funcional, siguiendo los principios del modelo de estrés físico, que puede ser guiado o dirigido por todos los valores fisiológicos explicados.
Palabras clave: Lesión por sobrecarga, consumo de oxígeno, paradigma biomecánico, umbral aeróbico, fisiología deportiva, músculo
Corresponding author: Fernando Pifarré San Agustín
fpifarre@gmail.com
Received: 11-01-2024
Accepted: 11-18-2024
Introduction
When engaging in physical activity, not only do musculoskeletal structures come into play—such as bones, muscles, tendons, ligaments, joint capsules, and menisci—but also biochemical reactions, in the form of aerobic and anaerobic metabolism. These reactions are studied in exercise physiology laboratories by specialists in sports medicine. These laboratories are increasingly utilized in respiratory and cardiological clinics, chronic fatigue evaluations, as well as in sports contexts. This is because studying ATP production pathways gives us direct insight into how the body responds to various energy demands.
Biochemical reactions occur in muscle cells, either in the cytoplasm (anaerobic metabolism) or the mitochondria (aerobic metabolism). The muscle is one of the most widely injured structures in sports, making it valuable to understand its metabolism, especially in relation to overuse injuries, frequently observed in the lower limbs and feet. For example, Kevin A. Kirby references the work of Cavanagh and Williams on oxygen consumption and its relationship to stride length variation during distance running(1). Their 1982 study, conducted with a primitive gas analyzer (Douglas bag) with a single O2 module—unlike today’s equipment, which includes CO2 modules—was groundbreaking in highlighting the importance of ATP production in skeletal muscle.
This study aims to connect exercise and sports physiology with stress-induced muscle injuries in the lower limbs, specifically the leg-ankle-foot complex. It explores exercise physiology concepts relevant to podiatry and attempts to correlate them with the physical stress paradigm proposed by Mueller and Maluf(2), which offers a comprehensive perspective on the impact of physical stress on locomotor tissues and overuse injuries.
Distinctions across 3 widely confused concepts
The human body can exist in two states: rest or activity(3). During rest, the body relies on minimal energy expenditure, known as basal metabolism, expressed in METs (metabolic equivalents). When active, the body’s activity can be categorized into three types:
- Physical Activity (PA): Any body movement produced by skeletal muscles that results in energy expenditure above basal metabolism. Everyday activities, such as dusting or ironing, are considered physical activity.
- Exercise: A planned, structured, and repetitive form of physical activity aimed at improving or maintaining physical fitness. Examples include going to the gym or running.
- Sport: A form of physical activity performed as a game or competition, requiring training and adherence to rules and regulations. Playing in leagues or tournaments, or preparing for competitions, falls under this category.
The first 2 concepts are closely linked to health, while the third sometimes leads to overuse injuries (OIs).
Exercise physiology concepts
The musculoskeletal system generates energy (ATP) via anaerobic and aerobic systems. Anaerobic pathways provide quick but short-lived energy. There are two processes: the alactic system, which relies on ATP and phosphocreatine stores, and the lactic system, based on anaerobic glycolysis in the cell cytoplasm.
In contrast, aerobic pathways yield a substantial amount of longer-lasting energy, which involves the oxidation of carbohydrates, lipids, and proteins, which break down into molecules that bind to acetyl coenzyme A and enter the mitochondria, where cellular respiration occurs in the presence of oxygen. Skeletal muscles function like race cars, making it crucial to understand fuel consumption and when to “pit stop” for refueling. This is governed by physiological parameters such as maximum aerobic power (MAP), aerobic threshold (Vt1), anaerobic threshold (Vt2), O2 utilization percentage (%O2) during the aerobic-anaerobic transition, and mechanical efficiency (ME). These parameters are now precisely evaluated through direct exercise testing(4).
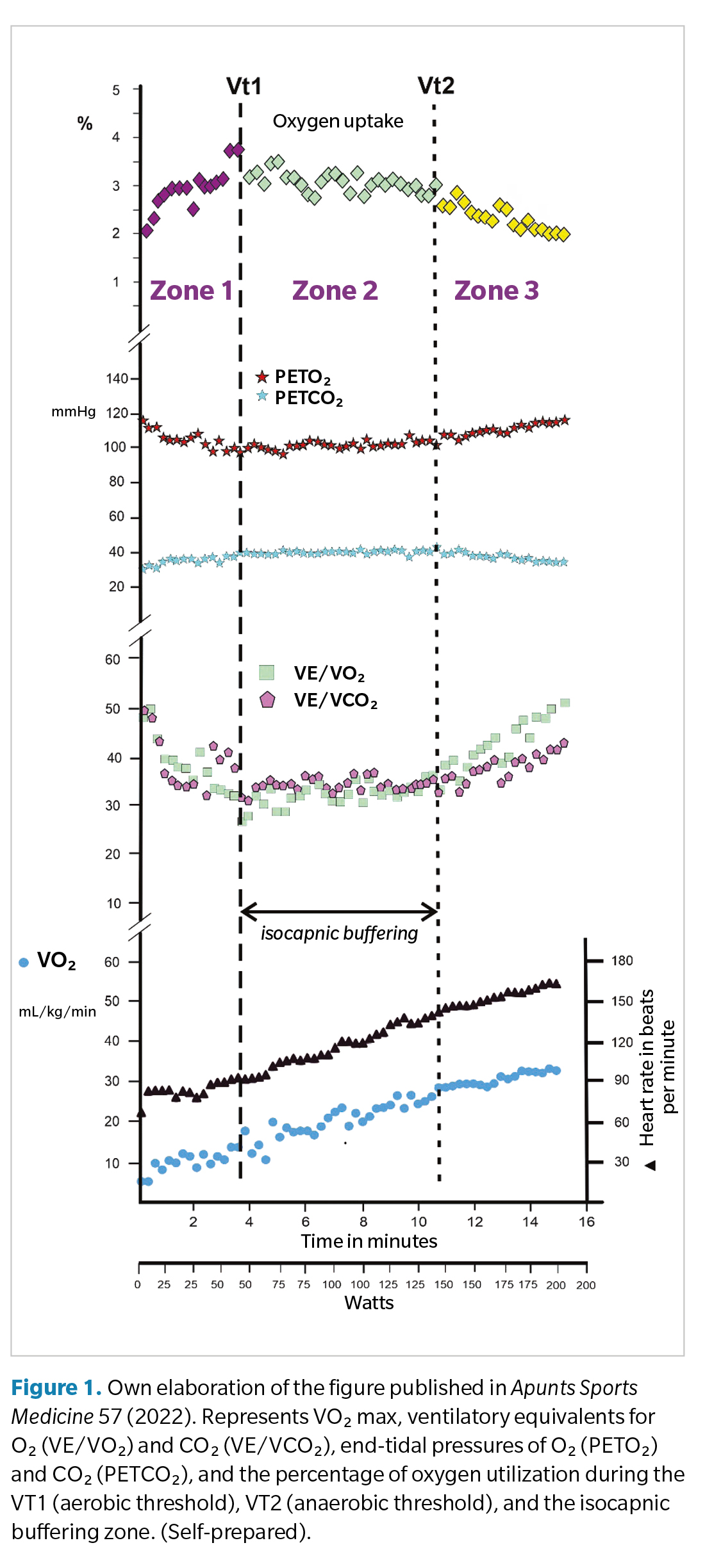
These physiological concepts are not commonly studied in podiatry programs. MAP is the maximum amount of oxygen the body can absorb, transport, and use per unit of time. Vt1 is the exercise intensity where lactate begins to accumulate in the blood, accompanied by a sudden increase in ventilatory parameters (oxygen consumption and CO2 production). Wasserman defined Vt2 as the exercise intensity(5) (above Vt1) where blood lactate concentration sharply increases, and ventilation becomes disproportionate relative to O2. The phase between Vt1 and Vt2 is called the aerobic-anaerobic transition phase, or isocapnic buffering, as the CO2 production-to-ventilation ratio remains stable.
ME is the ratio of energy produced to mechanical work generated (O2 required to increase speed by 1 km/h on a treadmill or power output by 1 watt on a cycle ergometer). Without disease, it should be < 10 mL O2/min on a cycle ergometer and < 200 mL O2/min on a treadmill, as shown in our studies(4). It should be trained during the final phase of a training program (three weeks before competition).
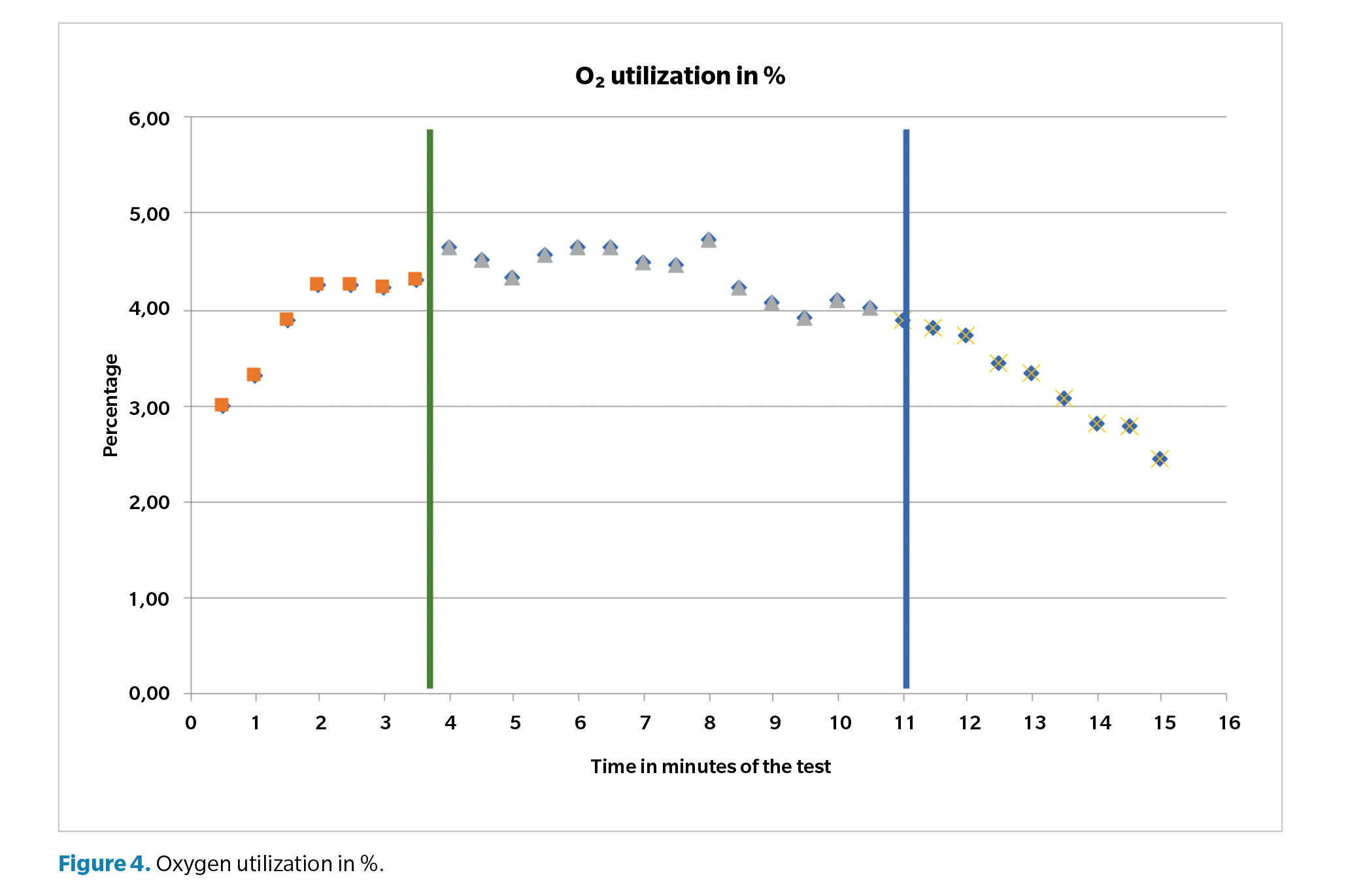
The final physiological concept is %O2 during the aerobic-anaerobic transition, considered good if > 3.2 %, as indicated in our research(4). However, this must be combined with the duration of the transition phase.
When performing a gas analysis exercise test (GAET), VO2 (oxygen consumption) progressively increases until it plateaus, reaching its maximum. To ensure a GAET is maximal, four criteria must be met: heart rate > 90 % of theoretical max; respiratory exchange ratio (RER) > 1.1; VO2max stabilizes at the test’s end; and evident or volitional fatigue(6). RER, the ratio of gas exchange (VCO2/VO2), > 1 during anaerobic phases, indicating greater CO2 ventilation relative to O2. Once the plateau has been reached, increasing exercise intensity will no longer increase VO2, known as VO2max (maximum oxygen consumption). VO2max is genetically determined by approximately 80% and is minimally trainable.
In the 1980s, VO2max was heavily emphasized. Later, Vt1 and especially Vt2 gained importance due to their trainability. Performing physical activity between these thresholds, especially slightly above Vt1, maximizes health benefits. However, exercising above Vt2 should be monitored, as this zone is speculated to be where most overuse injuries occur(7). Vt2 can be measured in heart rate (bpm), speed (km/h), or power (watts). Several methods exist to determine this value: the V-slope method (disproportionate ventilation increase), ventilatory equivalents for O2 and CO2, %O2, end-tidal oxygen and carbon dioxide pressures, heart rate deflection point (least accurate), and blood lactate concentration (> 4 mmol/L) (5) (Figure 1).
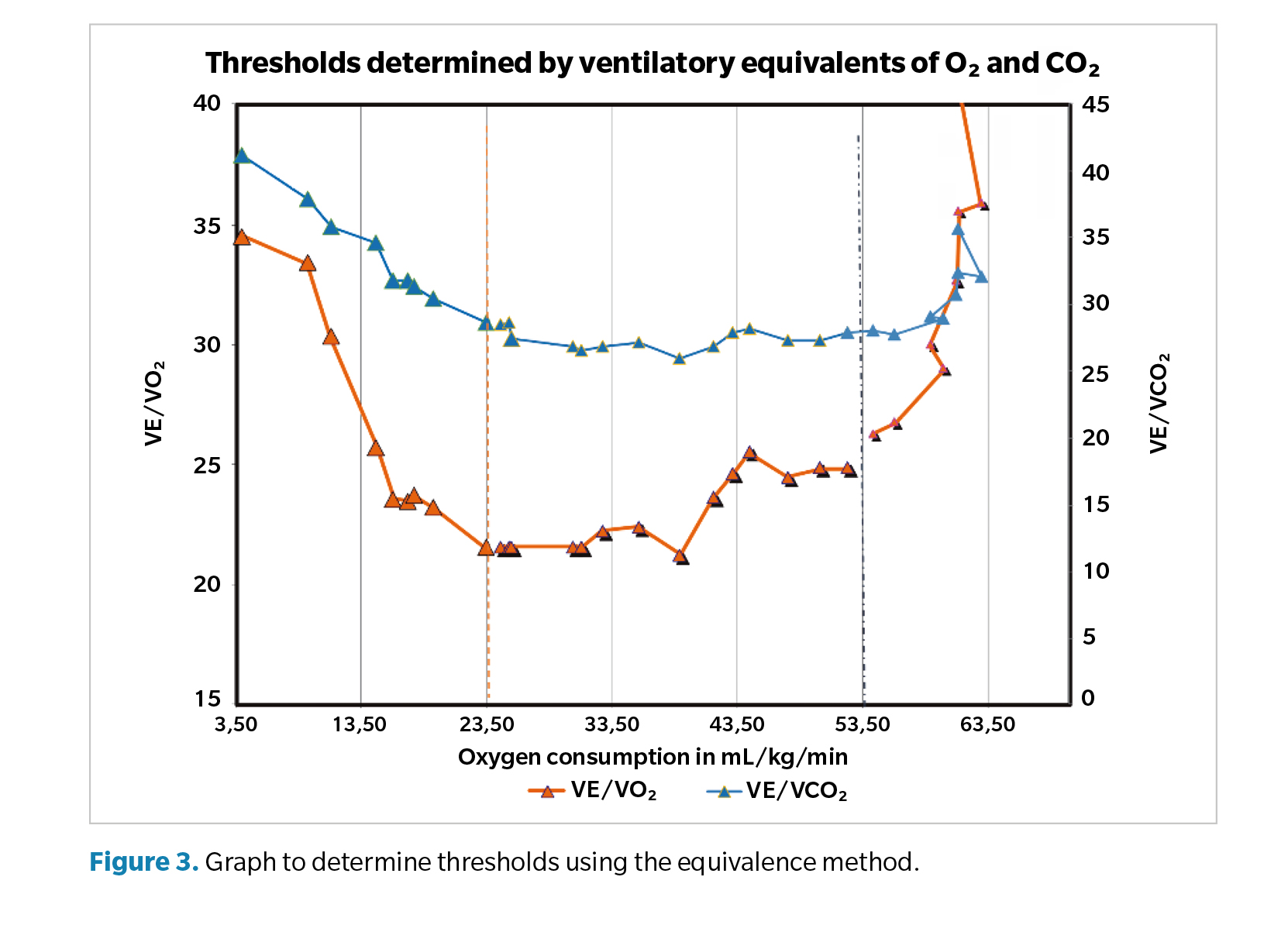
Training zones
Cardiopulmonary exercise testing (CPET) is routinely performed by a sports medicine physician before the pre-season begins. At the start of the season, the athlete begins their preparation and fine-tuning through progressive training, starting with extensive aerobic work. The exercise test allows precise determination of the athlete’s aerobic and anaerobic thresholds as well as their VO2max, enabling the definition of training zones and VO2 percentages. These parameters evolve during the season, ultimately achieving optimal physical fitness.
The training zones include regenerative training, extensive and intensive aerobic training, extensive anaerobic training (lactate tolerance I), and intensive anaerobic training (lactate tolerance II). Today, heart rate monitors equipped with algorithms can indirectly calculate these zones, defining them as “zones”(8). However, these methods are highly inaccurate. Following them without scientific oversight often results in various overloads during the season (Table 1).
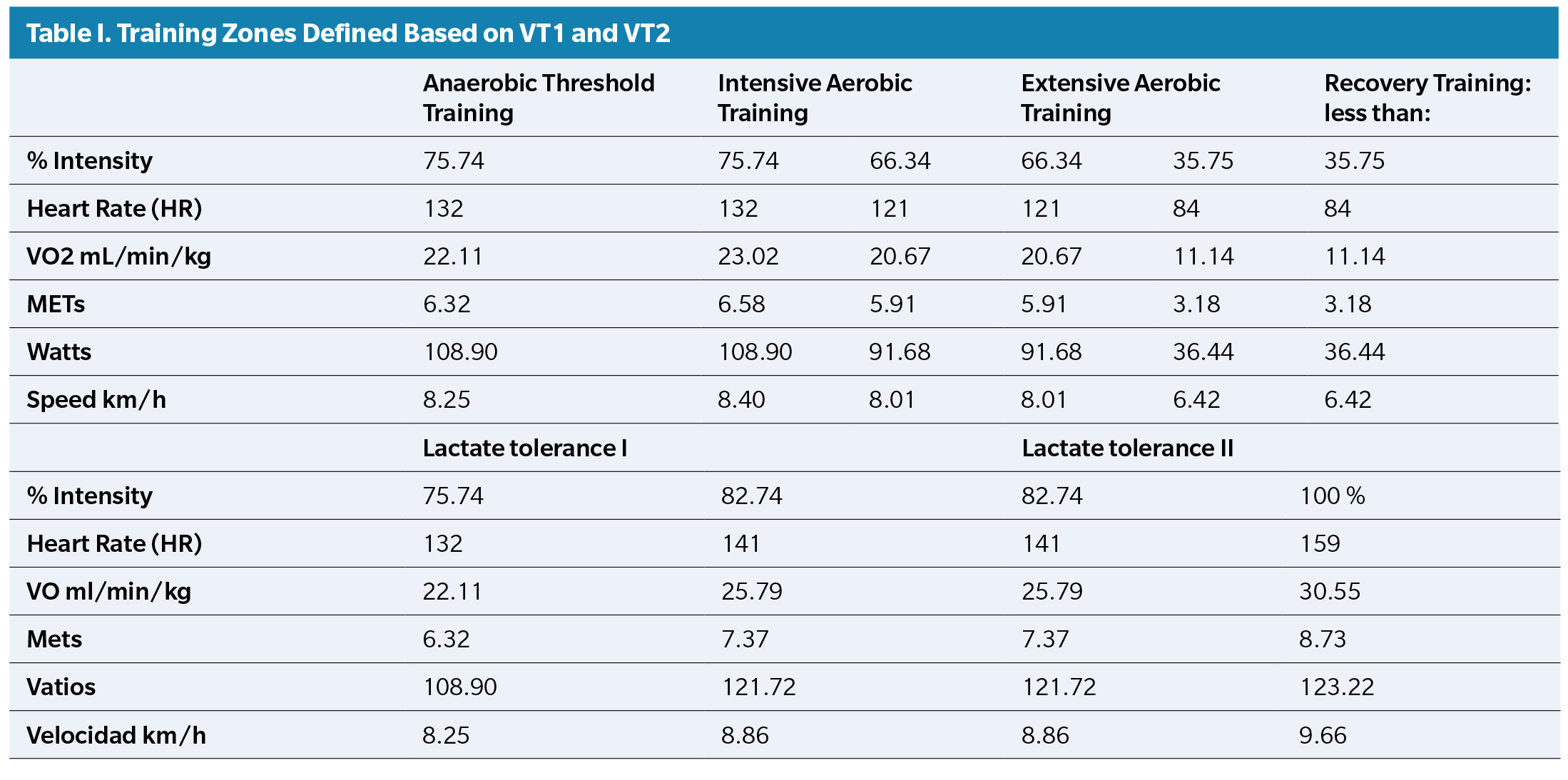
Calculation of Vt2
As previously explained, during an exercise test or progressively intensive physical activity, VO2 increases until reaching a point where ventilation also rises, entering the isocapnic buffering phase. At this initial increase in ventilation, the aerobic threshold (Vt1) is reached, corresponding to a blood lactate concentration of 2 mmol/L. If exercise intensity continues to increase, a sudden surge in ventilation occurs, corresponding to a blood lactate concentration of 4 mmol/L, which is the anaerobic threshold (Vt2). At this point, the isocapnic buffering phase ends, and the body enters a state of clear anaerobiosis, eventually achieving VO2max.
Vt2 can be determined in several ways: total ventilation (VE): As shown in Figure 2, VE follows a linear function represented by a regression line. On the graph, the x-axis represents time (in minutes), and the y-axis represents total ventilation (in liters/minute). A point appears where the two regression lines intersect. This point is Vt2. In the given example, this occurs at a VE of 95.78 liters, at minute 11 and 29 seconds, with the heart rate at 169 bpm.
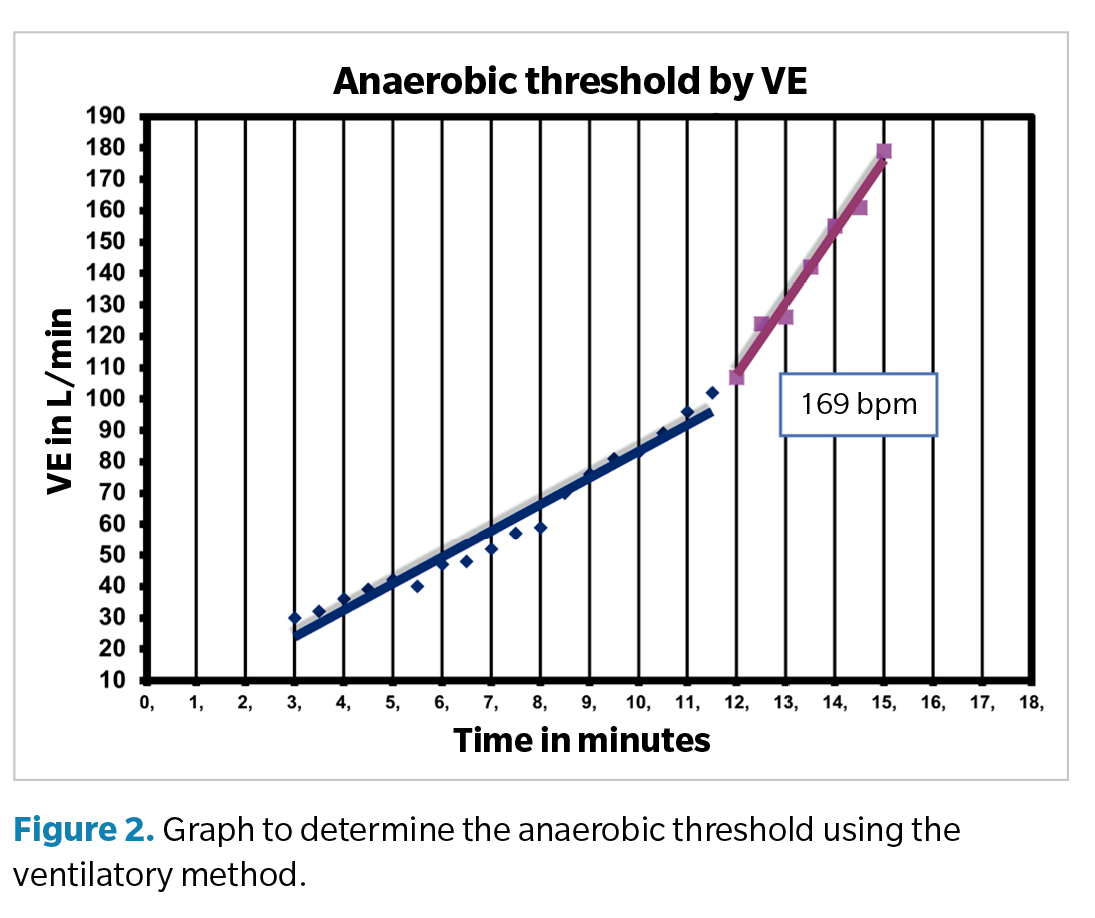
Ventilatory equivalents for O2 and CO2: the ventilatory equivalent for O2 is the VE/VO2 and CO2 ratio. As shown in Figure 3, plotting all values from the gas analyzer reveals that the VE/VCO2 ratio initially decreases (corresponding to Vt1), then stabilizes, and finally rises (corresponding to Vt2). The behavior of VE/VO2 similarly starts with a significant decrease (corresponding to Vt1), stabilizes, and then sharply increases (corresponding to Vt2).
Vt1 and Vt2 can also be assessed through blood lactate concentration. However, this relationship is not linear but rather exponential.
O2 utilization percentage (%O2)
One of the emerging concepts in exercise physiology is understanding the percentage of oxygen utilization (%O2)(9). When graphing its values, two distinct points corresponding to the aerobic threshold (Vt1) and anaerobic threshold (Vt2) can also be observed (Figure 4). After conducting over 3000 CPETs across a variety of populations—including high-performance athletes, sedentary individuals, patients with cardiovascular diseases, chronic fatigue, and lung cancer—we determined that a good %O2 during the aerobic-anaerobic transition phase is 3.2 % or higher(4). It is striking that, despite ambient oxygen concentration being approximately 20.95 % (with the remainder primarily nitrogen at 78 %), the body utilizes only about 3.2 % of oxygen. This percentage is a critical indicator of mitochondrial function in muscle cells and reflects the metabolic efficiency of the muscle. In cases of physical muscle injuries (e.g., rupture, overuse), metabolic deterioration is the first effect due to enforced rest in the affected area. After this rest period, physical therapy is initiated, followed by functional readaptation. Achieving a minimum %O2 of 3.2 % is essential for successful functional readaptation. This level is achieved through aerobic training during the initial stages of recovery. Starting with anaerobic training would be catastrophic. In addition to %O2, the duration of the transition phase is critical. Multiplying these factors (% and time) yields a value where higher scores indicate better oxygen utilization. Currently, this metric aids in diagnosing chronic fatigue(10) and predicting outcomes for lung cancer. Treatment decisions—whether to proceed with surgery or chemotherapy alone (associated with poorer prognosis)—depend on oxygen utilization. Similarly, %O2 helps determine candidates for lung transplants, independently of compatibility studies.
Another novel parameter is mechanical efficiency (ME), calculated by correlating power output (watts) or speed with MAP or VO2max. ME is vital for training programs, particularly in the pre-competitive or competitive phases.
As evident, exercise physiology extends far beyond elite sports, now having applications in cardiac and respiratory pathologies, chronic fatigue diagnosis, persistent COVID diagnosis, lung transplantation, and lung cancer treatment decisions.
Overuse injuries and the physical stress paradigm
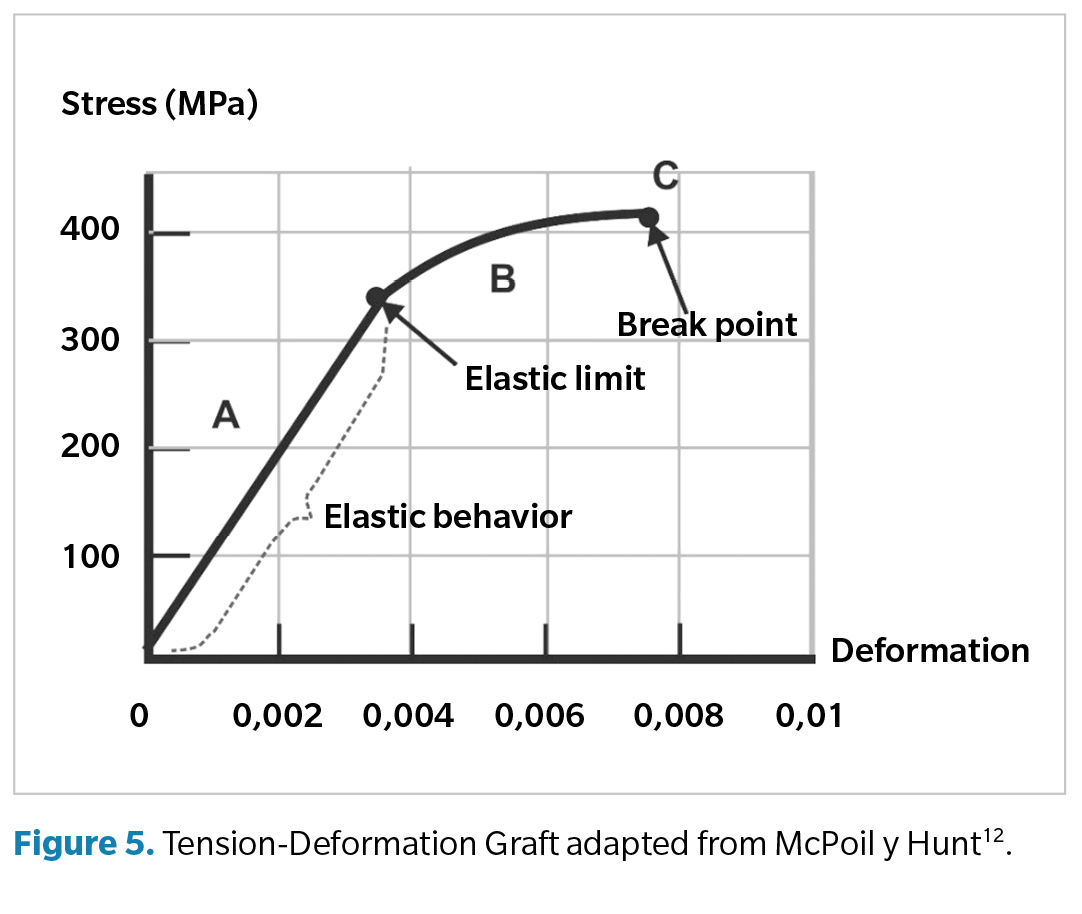
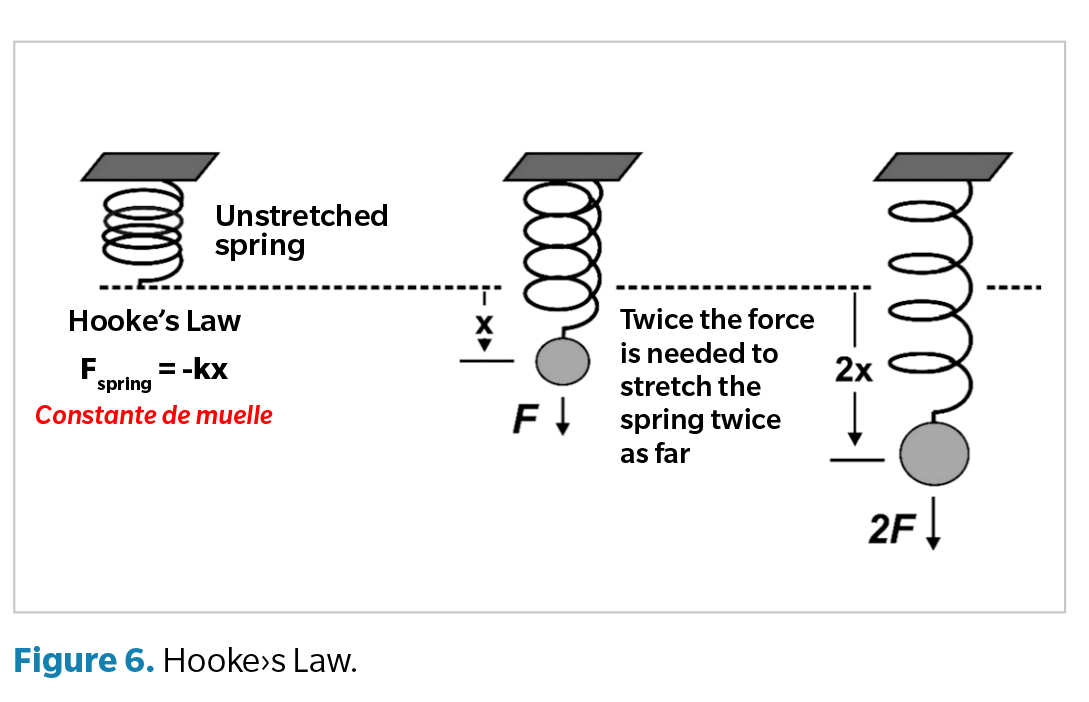
Several biomechanical paradigms explain lower limb (LL) overuse injuries(11). A common theoretical foundation among these paradigms is the law governing elastic material behavior. This concept is illustrated by Hooke’s Law (1635–1703), which examines how external force deforms an elastic material(11).
Applying this basic physics principle to musculoskeletal tissues underpins the tissue stress paradigm proposed by McPoil and Hunt(12). They identify the mechanical forces (internal or external tension) affecting lower limb tissues, the symptom duration (acute or chronic injury), pain onset, and functional limitations. Figure 5 illustrates this through a stress-strain curve for various musculoskeletal tissues, including bones, tendons, ligaments, joint capsules, and skin. McPoil and Hunt advocate reducing tissue stress using orthopedic measures or physical therapies to promote healing. Additionally, they recommend programs to improve elasticity and muscle strength for full recovery from overuse injuries(13).
Kevin Kirby further described the foot’s mechanical behavior based on the spatial positioning of the subtalar joint axis (STJ). He categorized feet into those with medially deviated STJ axes (predominantly pronatory moments) and those with laterally deviated STJ axes (predominantly supinatory moments) (14). Similarly, Eric Fuller proposed a classification resembling Kirby’s, using the medial or lateral deviation of the center of pressure (CoP) relative to the STJ axis, based on the weighted average concept(15). In Spain, Martín Rueda, a pioneer in sports podiatry, theorized a model akin to Michaud’s paradigm(16), known as the hinge joint model. This model posits that most LL joints, except for the midtarsal joint, function as hinge joints. Personally, I am very familiar with the topic, as during my residency in Sports Medicine at Residencia Blume in Barcelona, my department head, Dr. Ramón Balius Juli, and the director of the High-Performance Center (CAR) in Sant Cugat del Vallès, Barcelona, Dr. Joan Anton Prat Subirana, consulted this podiatrist regarding what could be done about the overuse injuries presented by our athletes preparing at the CAR for the Barcelona ‘92 Olympics. These injuries were mainly treated with rest at the time(11). For this purpose, a grant of €6000 was awarded for the design of the first validated pressure platform in the world and the Podomedel mold chamber(16,27). Today, this pressure platform continues to be used in the various CAR centers across Spain.
Ernesto Maceira(18) introduced the concept of energy conservation during gait for optimal running economy and explained how kinetic energy transforms into potential energy, and vice versa, at the center of mass. He considers gait to be a learned movement that is difficult to acquire but becomes automatic once mastered. If this gait is efficient, the musculoskeletal system will require minimal oxygen consumption to function adequately.
In 1986, Benno Nigg(19) a physicist at the University of Calgary, proposed the neurobiomechanical paradigm, theorizing that neither impact forces nor excessive pronation alone cause overuse injuries(19). Instead, muscles must adapt to modulate these forces. Nigg opposed highly cushioned footwear and excessive orthotic corrections, favoring natural pronation compensations at higher joint levels. His studies highlighted mitochondrial roles and VO2max in muscle energy sources.
After Cavanagh’s foundational study, Maceira became the third author in 25 years to address oxygen consumption. Today’s advanced gas analyzers allow the study of ATP and oxygen consumption, suggesting a new paradigm linking overuse injuries to mitochondrial activity and training zones.
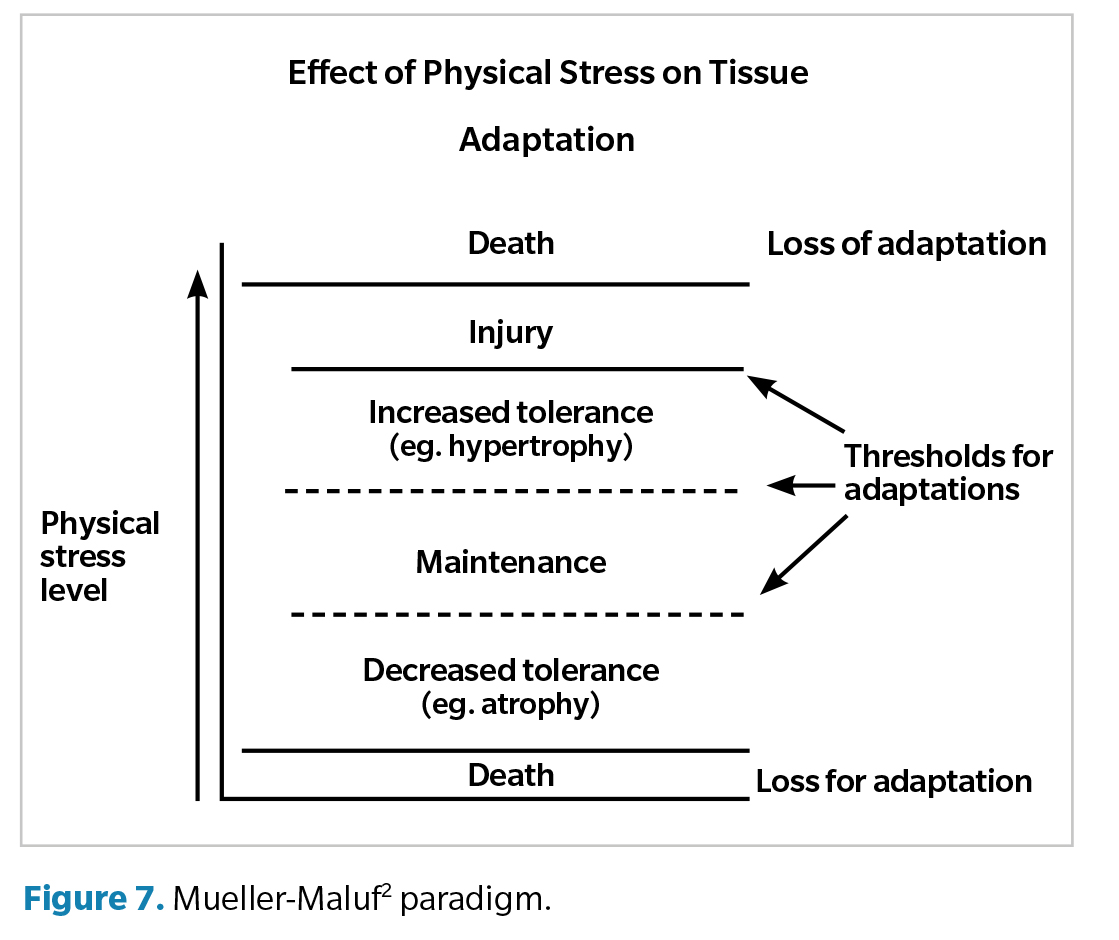
Mueller and Maluf’s paradigm(2) describes the effects of physical stress on musculoskeletal tissues under low or high stress levels. It defines optimal physical stress thresholds, with the musculoskeletal system adapting in five ways: atrophy, maintenance, hypertrophy, rupture, or death. Excessive stress can cause either significant atrophy or hypertrophy, leading to overuse injuries. During recovery, applying submaximal stress stimulates tissue repair; without stress, tissue atrophy occurs. Müller outlines physiological thresholds that influence recovery positively or negatively. Overuse injuries arise via three mechanisms: high magnitude stress over a short duration, low magnitude stress over an extended period, or moderate magnitude stress applied repeatedly (Figure 7).
Proposal for a new correlation model
If we consider the tissue stress model(12,), which correlates the force applied to a tissue with its corresponding stress, and the Mueller and Maluf model(2), which explains tissue response regarding applied stress to the tissue, it would be interesting to correlate these concepts with the physiological model of what occurs within the muscular mitochondria. If physical stress on a tissue is defined as the force applied over a specific tissue area(20), it seems logical to think that modulating this stress could aid in the rehabilitation of such tissue. The physical stress paradigm was developed to address how tissues, organs, and systems adapt to varying levels of physical stress. Tissues consist of specialized cells that cooperate to perform one or more functions, and tissues combine to form organs. The four tissue types in the human body are epithelial, connective, muscular, and nervous tissue. The physical stress model is perfectly applicable to all four tissue types. This paradigm defines thresholds—lower and upper limits of loads—within which a range of outcomes can occur, from significant atrophy to hypertrophy and tissue death. Between these two extremes, one can observe a decrease in tissue tolerance to stimulus, maintenance of the tissue based on stimulus, an increase in tissue tolerance to stimulus, tissue injury, and tissue death. However, this idea is applied macroscopically and does not address molecular or cellular issues. Our group aims to propose a model based on what occurs at the molecular or cellular level within the myocyte. We correlate these theoretical thresholds described by Müeller & Maluf with the mathematical thresholds Vt1 and Vt2 obtained in a CPET. The importance of this lies in the fact that Vt1 and Vt2, as we explained earlier, are mathematically precise for each patient but vary between individuals. For this reason, we believe that the numerical quantification we propose through physiological parameters can be highly relevant in rehabilitating overuse injuries. All of this can be represented in the different training zones, allowing the monitoring of load progression during the recovery process for overuse injuries.
Additionally, these ideas have significant potential applications in other fields, as they could explain and treat primary cardiac or pulmonary problems manifesting as heart or respiratory failure and causing severe physical deconditioning. The ideas from the Müeller & Maluf paradigm can be applied to improve this deconditioning through a personalized training program guided by Vt1 and Vt2, which determine the training zones obtained via CPET.
The goal of this article is to provide a theoretical framework for correlating the thresholds described in the physical stress theory with the Vt1 and Vt2 values to promote optimal responses in tissue recovery and training zones derived from a CPET. This approach would allow for the design of rehabilitation programs for affected tissues or organs based on scientifically and mathematically quantifiable principles of exercise physiology occurring in muscle mitochondria. We propose that extensive and then intensive aerobic training zones serve as a good complement for treating overuse injuries, as these zones promote an increase in the number of mitochondria and thus improve oxygen utilization. We reserve the zones beyond Vt2—i.e., extensive and intensive anaerobic zones—for cases where there has already been a full recovery from the injury, as these zones will enhance Vt2 and delay the onset of fatigue (read: overuse injury). These zones are well-defined both in terms of heart rate and as a percentage of VO2max between Vt1 and Vt2. We know that muscle is highly adaptable, as are tendons, ligaments, joint capsules, etc. (21), making quantifiable active rehabilitation potentially beneficial. Simultaneously, we must not overlook the role of orthotic devices designed to reduce physical stress on biological tissues, which are essential in treating overuse injuries. In the sports world, we understand that following this integrated rehabilitation system could result in a quicker and safer return to play, avoiding relapses or unnecessary delays in recovery(21).
Final reflexions
Although the need for further research in this area is evident, the purpose of this article is to propose a new application for CPET by correlating the physical stress paradigm proposed by Mueller and Maluf with overuse injuries, particularly at the muscular level.
The first consequence of an overuse injury preventing an athlete from training properly is a decrease in %O2, making it crucial to continue muscle stimulation since muscle atrophy is directly related to %O2. We must remember that ATP, aside from the scarce reserves available, is produced within the myocyte, either in its cytoplasm or mitochondria. Once this overuse injury is overcome, the athlete will gradually improve their physical condition through integrated training, with the final days focused on enhancing mechanical efficiency.
We acknowledge the need for more studies on this subject, which is not the aim of this article. Instead, we seek to provide preliminary references linking exercise physiology to overuse injuries from a mechanical perspective. Exercise physiology offers quantitative measurement of various parameters, and in research, quantifying data helps resolve part of the problem. Investigating exclusively with qualitative parameters, no matter how validated the study may be, is always more prone to errors and inaccuracies.
We acknowledge that these methods have significant limitations, but we are confident that future studies will correlate, using A.I., what occurs in the energy physiology of the muscle, as there are no overuse injuries in the basal muscle metabolism. Currently, the treatment for lung carcinoma is determined, whether through surgery or chemotherapy, based on the percentage of oxygen utilization. This decision impacts potential cure rates if surgery is performed, or a poor prognosis if only chemotherapy is used.(22) Medicine is becoming more precise every day, and this precision is obtained not by studying the macroscopic tissue but by examining its microscopic structure. Similarly, artificial intelligence will likely be able to perform molecular or ultramolecular studies of these energy production pathways in the not-too-distant future. We believe that the response thresholds of tissues proposed by Mueller and Maluf for the treatment of overuse injuries(22) could be compared to the training zones between Vt1 and Vt2, extensive aerobic training and intensive aerobic training. When cardiac rehabilitation is performed for heart failure, the work is done below Vt, and similarly, when treating significant deconditioning or physical deterioration, one must also work below Vt, as it is when the best benefits from a physical activity program are obtained.
Conflicts of interest
None declared.
Funding
None declared.
Authors’ contributions
Study conception and design: FPSA, VPP.
Data mining: FPSA, VPP.
Análisis e interpretación de los resultados: FPSA, VPP.
Creación, redacción y preparación del boceto inicial: FPSA, VPP.
Revisión final: FPSA, VPP, XOD, CEM, OHG.
References
- Cavanagh PR, Williams KR. The effect of stride length variation on oxygen uptake during distance running. Med Sci Sports Exerc. 1982;14(1):30-5. DOI: 10.1249/00005768-198201000-00006.
- Mueller MJ, Maluf KS. Tissue adaptation to physical stress: a proposed “Physical Stress Theory” to guide physical therapist practice, education, and research. Phys Ther. 2002;82(4):383-403.
- González Peris M. Guia de prescripció de l’exercici físic per a la salut. Barcelona: Generalitat de Catalunya; 2022.
- Pifarré San Agustín F, Rosselló L, Hileno R, Palmi J, Bañares L, Planas A, et al. The use of oxygen as a possible screaning biomarker for the diagnosis of chronic fatigue. Apunts Sports Med. 2022;57(214):100379. DOI: 10.1016/j.apunsm.2022.100379.
- López Chicharro J, Fernández Vaquero A. Fisiología del ejercicio físico. Madrid: Editorial Panamericana; 2008.
- Robergs RA, Dwyer D, Astorino T. Recommendations for improved data processing from expired gas analysis indirect calorimetry. Sports Med. 2010;40(2):95-111. DOI: 10.2165/11319670-000000000-00000.
- Galiano Orea D, Rueda Sánchez M. El pie del jugador de baloncesto y su influencia ante lesiones a distancia. Archivos de medicina del deporte: federación española de medicina del deporte y de la confederación iberoamericana de medicina del deporte. 1996;13(52):149-53.
- Grimaldi Puyana M, Cuadrado Reyes J. Medios para cuantificar la carga interna de entrenamiento de equipo. La frecuencia cardiaca, el consumo de oxígeno, la concentración de lactato en sangre y la percepción subjetiva del esfuerzo: un a revisión. Madrid: PubliCE Standard; 2011.
- Pifarré F, Sanuy X, Rosselló L, Blázquez J, Gil G, Reig F, et al. El aprovechamiento de oxígeno como un posible biomarcador en el síndrome de fatiga crónica. En: Rosselló i Aubach L, Montesó Curto P (ed.). Síndromes de sensibilización central y actividad física Tarragona: URV publicacions; 2019. p. 79-99.
- Nijs J, De Meirleir K. Prediction of peak oxygen uptake in patients fulfilling the 1994 CDC criteria for chronic fatigue syndrome. Clin Rehabil. 2004;18(7):785-92. DOI: 10.1191/0269215504cr751oa.
- Pifarré San Agustín F. Física y Biomecánica para fisioterapeutas o podólogos. Lérida: Ediciones de la Universidad de Lérida; 2021.
- McPoil TG, Hunt GC. Evaluation and management of foot and ankle disorders: present problems and future directions. J Orthop Sports Phys Ther. 1995;21(6):381-8. DOI: 10.2519/jospt.1995.21.6.381.
- McPoil TG, Schuit D, Knecht HG. A comparison of three positions used to evaluate tibial varum. J Am Podiatr Med Assoc. 1988;78(1):22-8. DOI: 10.7547/87507315-78-1-22.
- Kirby KA. Rotational equilibrium across the subtalar joint axis. J Am Podiatr Med Assoc. 1989;79(1):1-14. DOI: 10.7547/87507315-79-1-1.
- Rueda Sánchez M. Los desequilibrios del pie. Barcelona: Paidotribo; 2004.
- Montañola Vidal A. Sistema de análisis plantar y biomecánica de la marcha humana mediante plataformas optométricas de luz no estable (PONLE). Podol Clin. 2004;Nº Extra:50-61.
- Maceira Suárez E. Análisis cinemático y cinético de la marcha humana. Rev Pie y tobillo. 2003;17(1):29-37.
- Nigg BM, Nurse MA, Stefanyshyn DJ. Shoe inserts and orthotics for sport and physical activities. Med Sci Sports Exerc. 1999;31(7 Suppl):S421-8. DOI: 10.1097/00005768-199907001-00003.
- Fukubayashi T, Kurosawa H. The contact area and pressure distribution pattern of the knee. A study of normal and osteoarthrotic knee joints. Acta Orthop Scand. 1980;51(6):871-9. DOI: 10.3109/17453678008990887.
- Pedret C, Rodas G, Balius R, Capdevila L, Bossy M, Vernooij RW, et al. Return to Play After Soleus Muscle Injuries. Orthop J Sports Med. 2015;3(7):2325967115595802. DOI: 10.1177/2325967115595802.
- Nawoor-Quinn Z, Oliver A, Raobaikady R, Mohammad K, Cone S, Kasivisvanathan R. The Marsden Morbidity Index: the derivation and validation of a simple risk index scoring system using cardiopulmonary exercise testing variables to predict morbidity in high-risk patients having major cancer surgery. Perioper Med (Lond). 2022;11(1):48. DOI: 10.1186/s13741-022-00279-8.
- Pifarré San Agustín F, Escoda Mora J, Casal Castells A, Prats Armengol T, Carles Gomá S, Levy Benasuly AE. Las lesiones por sobrecarga en las extremidades inferiores desde el punto de vista biomecánico. Rev Int Cienc Podol. 2016;10(2):106-21.