DOI: http://dx.doi.org/10.20986/revesppod.2024.1686/2024
ORIGINAL
Qualitative pilot study on the orthotic management of tibialis posterior tendon dysfunction by podiatrists
Estudio piloto cualitativo sobre el manejo ortopédico de la disfunción del tendón tibial posterior por podólogos
George Banwell1
Eva Lopezosa Reca1
Alfred Gatt2
Gabriel Gijón Noguerón1
Laura Ramos Petersen1
1Departamento de Enfermería y Podología. Universidad de Málaga, España
2Departament of Podiatry. University of Malta. Msida, Malta
Abstract
Introduction: Posterior tibial tendon dysfunction (PTTD) is a progressive and disabling condition with both conservative and surgical treatment options. The aim of this qualitative pilot study was to identify the differences in the methods of assessment and conservative management by a group of podiatrists.
Material and methods: The data was collected through recorded structured interviews, including questions related to the treatment and methods of assessment used for the pathology of PTTD. A thematic analysis of the transcripts was carried out to identify the codes and themes. Six podiatrists were interviewed in their own clinical setting.
Results: Seven themes were extracted from the interviews after the thematic analysis. The results varied between the podiatrists, some putting more emphasis on certain aspects of assessment and treatment than others. There were differences between treatment methodology, the types of professionals referred to and follow up periods. There were some similarities with certain treatments, such as foot orthosis treatment, however differences in the materials and modifications used.
Conclusion: Due to the small differences between the assessment and treatment methodology, and the lack consensus on certain aspects, more research should be done to identify a more detailed orthotic management of PTTD and a guideline created to prevent variability in treatment.
Key words: Posterior tibial tendon dysfunction, foot orthoses, podiatrist, treatment, outcome measures
Resumen
Introducción: La disfunción del tendón tibial posterior (DTTP) es una condición progresiva y discapacitante con opciones de tratamiento tanto conservadoras como quirúrgicas. El objetivo de este estudio piloto cualitativo fue identificar las diferencias en los métodos de evaluación y manejo conservador por parte de un grupo de podólogos.
Material y métodos: Los datos se recopilaron a través de entrevistas estructuradas grabadas, que incluyeron preguntas relacionadas con el tratamiento y los métodos de evaluación utilizados para la patología de la DTTP. Se realizó un análisis temático de las transcripciones para identificar los códigos y temas. Se entrevistó a seis podólogos en sus propios entornos clínicos.
Resultados: Se extrajeron 7 temas de las entrevistas después del análisis temático. Los resultados variaron entre los podólogos, algunos enfatizando más ciertos aspectos de la evaluación y el tratamiento que otros. Hubo diferencias en la metodología de tratamiento, los tipos de profesionales a los que se referían y los periodos de seguimiento. Hubo algunas similitudes con ciertos tratamientos, como el tratamiento con ortesis para el pie, sin embargo, hubo diferencias en los materiales y modificaciones utilizados.
Conclusión: Debido a las pequeñas diferencias entre la metodología de evaluación y tratamiento, y la falta de consenso en ciertos aspectos, se debería realizar más investigación para identificar un manejo ortopédico más detallado de la DTTP y crear pautas para prevenir la variabilidad en el tratamiento.
Palabras clave: Disfunción del tendón tibial posterior, ortesis para el pie, podólogo, tratamiento, medidas de resultado
Received: 10-01-2024
Accepted: 12-02-2024
Corresdepondence: Eva Lopezosa Reca
evalopezosa@uma.es
Introduction
The tibialis posterior tendon (TPT) is the largest and most anterior tendon on the medial aspect of the ankle(1). The TPT is susceptible to Posterior Tibialis Tendon Dysfunction (PTTD), which is a multifactorial condition, caused by a combination of intrinsic and extrinsic factors, such as mechanical overload, malalignment, and inflexibility(2). It is a common pathology, which has been shown to have a prevalence of up to 10 % in middle-aged women(3), as well as a high prevalence of PTTD in obese patients, and those who also suffer from plantar fasciitis(2).
Diagnosis of PTTD can be performed using physical assessments, such as the single(4,5,6) or double heel rise test(7), as well as imaging methods such as ultrasound or Magnetic Resonance Imaging (MRI) (8,9,10,11). Other tests which have also been described in the literature include: the posterior tibial edema sign (PTE) (4,9), first metatarsal rise (FMR) sign(7), first ray mobility test(11), unipedal standing balance test(3), pain on palpation of tendon of the TP(4), weakness with contraction4, and too many toes sign(6).
Non-surgical treatments for PTTD that have been defined in the literature include physiotherapy(12,13,14,15,16) and orthotics, such as foot orthoses (FO) (17,18,19,20,21,22) and ankle foot orthoses (AFO) (15,16,19,21,23).. Often these treatments are used in combination for optimal results(14,15,16,21).. Other therapies also include ice therapy, anti-inflammatory medication, rest, footwear, weight loss, therapeutic ultrasound, and patient education(24).
A study in which 29 podiatrists were interviewed highlights a variety in assessment methods specifically related to “real time gait analysis” with 132 different observations noted during the assessment(25). Another study which interviewed patients with PTTD highlighted the poor knowledge among health care professionals to refer correctly and in a timely manner to someone who can diagnose and treat the issue(26). Not only this but a 2021 study looking at 186 patients, concluded that white patients were 2.8 times more likely to receive orthotics than black people(27). Therefore, more understanding is needed to identify treatment patterns in PTTD to better understand the clinical reasoning.
Therefore, the aim of this study was to investigate what methods are used by a group of podiatrists in the process of diagnosis, treatment, and referral pathway for PTTD, to identify if continuity exists within these professionals.
Materials and methods
This study adopted a qualitative approach to explore the experiences of podiatrists and their approach to PTTD regarding the assessment, referral, and treatment of the pathology, with a particular focus on orthotics.
Participants
The target population was podiatrists who work with patients living with PTTD. Podiatrists who were not registered with an association were excluded. Subjects were invited to participate in the qualitative study via email, where the details of the study were presented. Participants willing to take part in the study were contacted by telephone to determine their availability. They all agreed to take part in the study and provided informed and written consent. Interviews took place from February to March 2022.
Data collection
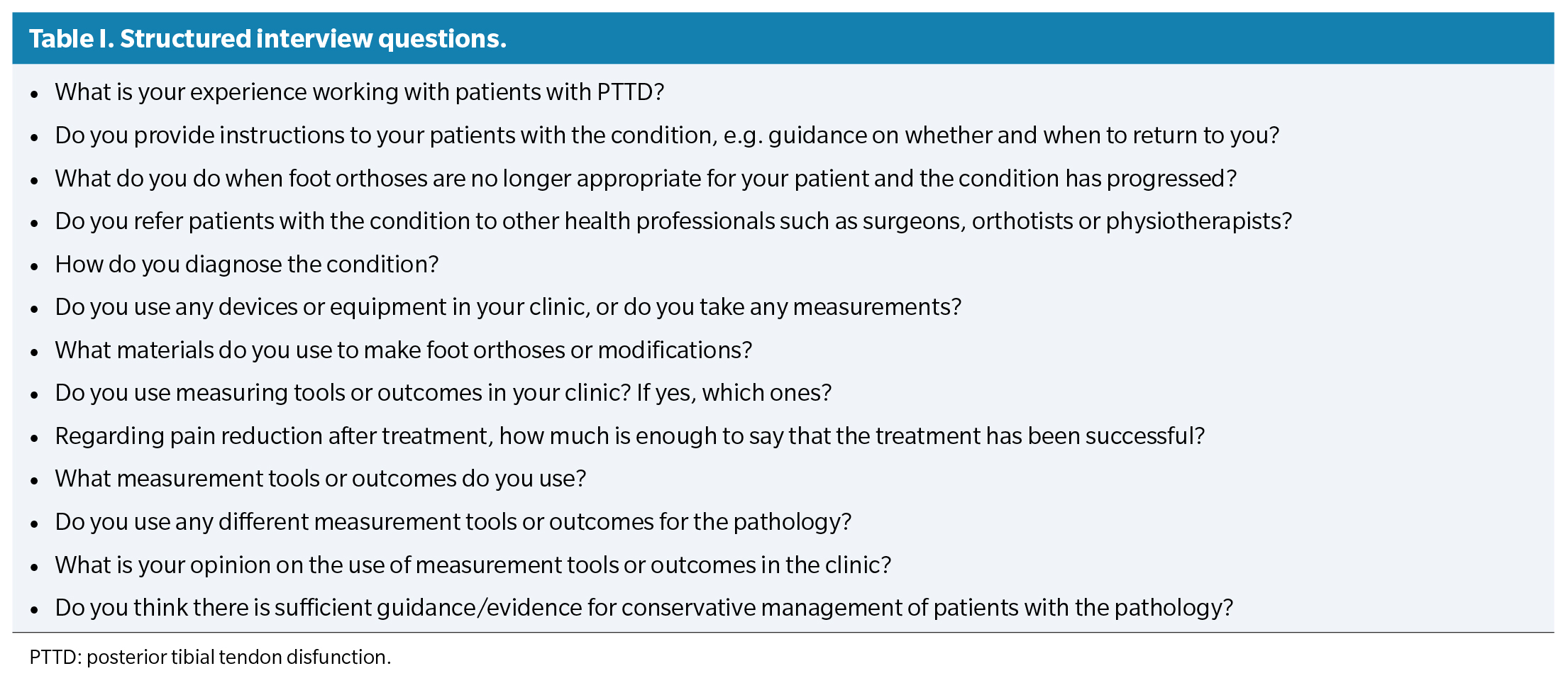
Data collection was performed through structured interviews, with questions previously drafted using the knowledge of the clinical researcher as a guide and a review of the literature on PTTD (Table 1). All questions were approved by the Ethics Committee. Interviews were recorded with a handheld recorder and field notes were also taken to supplement the data. Quantitative data were also collected, in particular the number of years of clinical experience. The interviews were conducted by a single researcher (GB), who is experienced in the management of PTTD. Interviews were not repeated, and transcripts were not returned to participants for comment.
Data analysis
Braun and Clarke’s six-step thematic analysis framework for data analysis was followed(28). Data analysis was carried out by two researchers. The interviews were transcribed from the recordings, a line-by-line analysis of the transcribed experiences of each participant was conducted, field notes and all transcripts were read, and codes were developed. The initial codes were then collated and grouped into themes. Particular attention was paid to both the frequency of emerging codes and their importance to multiple participants. Finally, the extracted codes were reviewed within their themes, defined, and named. MAXQDA 2022 qualitative data analysis software was used to facilitate coding and analysis.
Results
A total of 6 interviews were analysed thematically. Within the participants, 2 were female and 4 were male and the range of experience of working with the PTTD varied from 2 to 16 years. From the interviews, 54 codes were identified, which were organized into 7 themes:
- Equipment, instruments, and assessment methods.
- Measurement tools.
- Treatment.
- Materials and modifications used in the manufacture of FO.
- Procedure to follow if the initial treatment did not work.
- Instructions provided to patients.
- Treatment success.
Theme 1. Equipment, instruments, and assessment methods
All participants mentioned the use of clinical tests, in particular the heel rise test was mentioned by the majority. Some mentioned the importance of the difference between single and double heel rise test. In addition, one participant indicated the performance of a biomechanical evaluation and the assessment of the windlass mechanism. The vast majority also mentioned that pain is a good indicator of the pathology.
Most of the participants said that they use some kind of equipment, such as a pressure platform or treadmill, justifying that it guides them in their treatment and follow-up methods. Five of the participants mentioned the use of ultrasound for diagnosis and/or follow-up of PTTD throughout treatment and some also mentioned the use of MRI. One aspect that was raised was the price of assessment methodology, as the cost of certain tests was deemed to not be justifiable due to their cost or that the patient would not be able to afford it: “Well depending on the patient’s ability to access that test. Sometimes it is more complicated to ask for it or the patient cannot afford it” (Participant 4).
Less experienced participants attached particular importance to having a long conversation with the patient prior to the physical assessment: “I almost spend 10 minutes talking to the patient” (Participant 3).
Theme 2. Measurement tools
None of the participants reported using an official outcome measure specific to the foot and ankle to assess their patients. However, all participants assessed the outcome of their treatments, all using a visual analogue scale (VAS)29 to assess the level of pain before and after treatment. Most participants defined this scale as their primary assessment: “I mostly use the visual analogue pain scale, the patient tells me that they are doing better, that their daily life has improved” (Participant 6).
One participant said that after treatment they re-evaluate their patients with the heel rise test: “You can do the heel rise test again, to assess if you have actually managed to reverse some of the functional disability of the tendon” (Participant 1).
Theme 3. Treatment
One of the participants mentioned that part of the treatment would be to explain the pathology to the patient: “I explain the pathology they have” (Participant 5).
All participants mentioned the use of FO or some kind of orthosis, however, this was the only thing that all participants agreed on in terms of treatment.
Injection therapy was mentioned by half of the participants as a possible initial treatment. Laser, taping, dry needling, and the use of ice were also mentioned, however they were only mentioned once. Regarding other orthotic treatment methods, only two participants mentioned the use of an AFO as a possible treatment: “Otherwise often the next step would be injection therapy, physiotherapy and in some cases I have had to use some AFO splints” (Participant 6).
Theme 4. Materials and modifications used in the manufacture of FO
The materials used by participants to make FOs varied, with most providing an explanation as to why they used those materials. One participant, while not providing the name of the material, did provide a detailed explanation of what is required of the FO to reduce pathological forces: “Semi-rigid or rigid FO, which act as a support for the arch and simulate the tendon force, pulling the arch upwards” (Participant 1).
Half of the participants indicated the use of polypropylene, indicating the specific thickness and a detailed explanation of why: “I always opt for hard materials, such as 3-millimeter polypropylene. Can you use other materials that I can reinforce? Yes, you can use them, like resin or 2-millimeter polypropylene, but in this case, they are patients with a large component of pronation, collapsed, and that is why I use 3-millimeter polypropylene and high-density EVA (Ethylene-vinyl acetate) for posting” (Participant 6).
On the other hand, other participants did not provide an explanation, simply indicating the material they use: “Resin and EVA” (Participant 3).
Theme 5. Procedure to follow if the initial treatment did not work
Most participants indicated that, if the initial treatment did not work, they would undertake other more aggressive treatments and/or refer to another healthcare professional, such as a physiotherapist, if they had not done so before. All mentioned referral to an orthopedic surgeon for surgical treatment. Only one participant said that they would refer to an orthotist and highlighted the importance of the multidisciplinary team within the treatment of PTTD. In addition, another participant, although mentioning an AFO, identified it as an aggressive treatment: “Normally this pathology cures quite well because as the cause is purely mechanical, many times controlling the pronation, with a more aggressive treatment, they usually have a good response” (Participant 4).
One participant mentioned that they would reassess the patient and assess if anything else could be done before referring: “I do a new biomechanical examination and see if any modifications can be made” (Participant 5).
One of the participants mentioned that if the patient refused orthotic treatment, other treatments to reduce pain would be offered.
Theme 6. Instructions provided to patients.
The instructions provided by the participants to their patients varied widely in terms of follow-up appointments, footwear advice, weight management and physiotherapy as an adjunctive treatment.
Some of the participants had strict guidelines that they followed regarding follow-up appointments and others were more flexible. Most described an initial follow-up, which ranged from 1.5 weeks to 1 month. Two participants indicated that the patient would have a follow-up at 1 month, however, if the patient had problems, they should return earlier. Regarding further follow-up, there was also no consensus, with some participants indicating a 6-month follow-up, others the patient should return if they have any problems, and the majority indicating a 1-year follow-up.
Half of the participants interviewed considered footwear advice to be important; one participant said that this was one of the most important aspects of treatment. Another element that was highlighted as very important by one participant was weight, however, the rest did not mention it: “The endocrinologist and nutritionist can help us by decreasing the patient’s weight, which usually improves the symptomatology” (Participant 1).
Most participants mentioned that they provide recommendations of some form of physiotherapy exercise, particularly strengthening. Some also indicated the importance of increased proprioception and reduced inflammation, which would be provided by them, or by a physiotherapist.
Theme 7. Treatment success
There were a variety of responses as to what participants considered to be successful treatment. One participant defined that successful treatment takes time, due to the constant load on the foot.
Some participants defined that for treatment to be successful, the patient had to be pain free, unless they were doing a lot of activity: “I always try to aim for virtually complete absence of pain. To be 100% successful for me there has to be total absence of pain” (Participant 5).
One participant simply defined a reduction in pain as sufficient, even if complete absence was not achieved: “You don’t need 100 %, if it is reduced from an 8 to a 4, I consider it successful” (Participant 2).
Other participants described in more detail why complete absence of pain may not be an appropriate or possible goal: “For me, when the patient is able to do the activities that they want to do, within logic, the treatment is successful” (Participant 6).
Discussion
This qualitative pilot study has answered the main objective by identifying differences in the methods of assessment, referral, and conservative treatment of PTTD by a group of podiatrists. The results demonstrate a lack of unanimity in the opinions of the participants on the management of PTTD, including variation in assessment, treatment, referral practices and follow-up duration.
The methodology used to make the diagnosis varied, with some participants placing more emphasis on certain techniques over others. However, one method which was used by all was the heel rise test, which has been previously described in the literature(4,5,6).
Regarding treatment methodology, all participants used FO, however the specific prescription was varied regarding the material and design of the devices. Only two participants reported orthotic treatment other than FO, such as AFO. This highlights that most participants are either unaware of the importance of an AFO for the treatment of this condition in the later stages or feel that it is not appropriate. This has been previously defined in the literature as important in both the early and late stages of the condition (15,16,19,21,23).
When asked about follow-up practices, there was also variability, with some patients being seen earlier than others, with no explanation as to why patients were reviewed this way. However, most participants instructed their patients to return if they had problems. Considering the progressive nature of the condition, if the patient must wait a long time for an appointment with the surgeon and/or physiotherapist, then this could lead to a progression of the condition, causing further disability and frustration for the patient(26).
During the interviews, references were made to multiple health care professionals by most of the participants, stating that other professionals can be relied upon when treatment had been unsuccessful. However the time of referral was not clearly defined, and few participants discussed the referral to other healthcare professionals as a routine part of their treatment. This highlights the lack of importance of a multidisciplinary team approach to the treatment of the condition. Considering all the elements that can both improve and worsen the condition, the lack of a multidisciplinary approach in the early stages of the condition is suboptimal. The problem of both the lack of continuity of treatment and the importance of the multidisciplinary team are highlighted in an article by Bowring and Chockalingham in 2009(30).
Most described the use of a VAS to measure pain and certain physical tests to determine the outcome of their treatment. However, when discussing how they measure the success of their treatment, some also mentioned the happiness of the patient and quality of life, without indicating the use of a subjective outcome measure to evaluate and document this. Regarding whether a treatment has been successful or not, there was also a variety of responses. Some participants considered that a reduction in pain with which both the practitioner and the patient are happy was sufficient, and that some residual pain is to be expected. Other participants however defined residual pain as unacceptable and that all options should be exhausted to the point where treatment is as successful as it can be.
Thought should be given to the lack of consensus, and whether this is a reflection of a lack of evidence, or a lack of knowledge about PTTD. More concrete guidelines should be provided to ensure standardization of care of PTTD, especially due to its progressive nature. More research is needed to identify whether this would be a practical and implementable solution to reduce variability.
The limitations of this paper are the small number of participants included as well as the lack of variety of professionals, since it would have been interesting to determine how other professionals, besides podiatrists, manage PTTD. The strengths of this paper are that it is the first to identify the methodology used by a group of podiatrists in the management of PTTD.
Future research should be aimed at reviewing the literature to see if there is sufficient evidence on the best treatment practices for the condition, as well as to gather the opinions of experts to create a best practice guideline.
This paper shows that there is a lack of unanimity regarding diagnosis, advice, treatment, follow up, and referral practices. This lack of unanimity is likely due to a lack of evidence on the appropriate management of PTTD, as well as a lack of an official detailed guideline.
Ethical Declaration
This qualitative study received the ethical approval from the Eth- ics Committee of the Universidad Católica San Antonio de Murcia (UCAM) (CE012208). This study was carried out in full accordance with the provisions of the Declaration of Helsinki regarding ethical principles for medical research involving human subjects.
Conflict of interest
The authors declare no conflicts of interest.
Funding
None.
Author’s contributions
Conception and study design: GB, LRP.
Data collection: GB, LRP.
Result analysis and interpretation: GGN, LRP.
Creation, drafting, and preparation of the initial draft of the paper: AG, GGN.
Review and final acceptance: ELR, AG, GGN.
References
- Lhoste-Trouilloud A. The tibialis posterior tendon. J Ultrasound. 2012;15(1):2-6. DOI: 10.1016/j.jus.2012.02.001.
- Federer AE, Steele JR, Dekker TJ, Liles JL, Adams SB. Tendonitis and Tendinopathy: What Are They and How Do They Evolve? Foot Ankle Clin. 2017;22(4):665-76. DOI: 10.1016/j.fcl.2017.07.002.
- Kohls-Gatzoulis J, Angel J, Singh D. Tibialis posterior dysfunction as a cause of flatfeet in elderly patients. Foot. 2004;14(4):207-9. DOI: 10.1016/j.foot.2004.06.003.
- Kulig K, Lee SP, Reischl SF, Noceti-DeWit L. Effect of posterior tibial tendon dysfunction on unipedal standing balance test. Foot Ankle Int. 2015;36(1):83-9. DOI: 10.1177/1071100714551020.
- Ross MH, Smith MD, Mellor R, Durbridge G, Vicenzino B. Clinical Tests of Tibialis Posterior Tendinopathy: Are They Reliable, and How Well Are They Reflected in Structural Changes on Imaging? J Orthop Sports Phys Ther. 2021;51(5):253-60. DOI: 10.2519/jospt.2021.9707.
- Albano D, Martinelli N, Bianchi A, Romeo G, Bulfamante G, Galia M, et al. Posterior tibial tendon dysfunction: Clinical and magnetic resonance imaging findings having histology as reference standard. Eur J Radiol. 2018;99:55-61. DOI: 10.1016/j.ejrad.2017.12.005.
- Hintermann B, Gächter A. The first metatarsal rise sign: A simple, sensitive sign of tibialis posterior tendon dysfunction. Foot Ankle Int. 1996;17(4):236-41. DOI: 10.1177/107110079601700410.
- Arnoldner MA, Gruber M, Syré S, Kristen KH, Trnka HJ, Kainberger F, et al. Imaging of posterior tibial tendon dysfunction - Comparison of high-resolution ultrasound and 3 T MRI. Eur J Radiol. 2015;84(9):1777-81. DOI: 10.1016/j.ejrad.2015.05.021.
- Gonzalez FM, Harmouche E, Robertson DD, Umpierrez M, Singer AD, Younan Y, et al. Tenosynovial fluid as an indication of early posterior tibial tendon dysfunction in patients with normal tendon appearance. Skeletal Radiol. 2019;48(9):1377-83. DOI: 10.1007/s00256-018-3142-y.
- DeOrio JK, Shapiro SA, McNeil RB, Stansel J. Validity of the posterior tibial edema sign in posterior tibial tendon dysfunction. Foot Ankle Int. 2011;32(2):189-92. DOI: 10.3113/FAI.2011.0189.
- Nallamshetty L, Nazarian LN, Schweitzer ME, Morrison WB, Parellada JA, Articolo GA, et al. Evaluation of posterior tibial pathology: Comparison of sonography and MR imaging. Skeletal Radiol. 2005;34(7):375-80. DOI: 10.1007/s00256-005-0903-1.
- Kulig K, Lederhaus ES, Reischl S, Arya S, Bashford G. Effect of eccentric exercise program for early tibialis posterior tendinopathy. Foot Ankle Int. 2009;30(9):877-85. DOI: 10.3113/FAI.2009.0877.
- Bek N, ?im?ek IE, Erel S, Yakut Y, Uygur F. Home-based general versus center-based selective rehabilitation in patients with posterior tibial tendon dysfunction. Acta Orthop Traumatol Turc. 2012;46(4):286-92. DOI: 10.3944/AOTT.2012.2488.
- Kulig K, Reischl SF, Pomrantz AB, Burnfield JM, Mais-Requejo S, Thordarson DB, et al. Nonsurgical management of posterior tibial tendon dysfunction with orthoses and resistive exercise: A randomized controlled trial. Phys Ther. 2009;89(1):26-37. DOI: 10.2522/ptj.20070242.
- Alvarez RG, Marini A, Schmitt C, Saltzman CL. Stage I and II posterior tibial tendon dysfunction treated by a structured nonoperative management protocol: An orthosis and exercise program. Foot Ankle Int. 2006;27(1):2-8. DOI: 10.1177/107110070602700102.
- Houck J, Neville C, Tome J, Flemister A. Randomized Controlled Trial Comparing Orthosis Augmented by Either Stretching or Stretching and Strengthening for Stage II Tibialis Posterior Tendon Dysfunction. Foot Ankle Int. 2015;36(9):1006-16. DOI: 10.1177/1071100715579906.
- Chicoine D, Bouchard M, Laurendeau S, Moisan G, Belzile EL, Corbeil P. Biomechanical effects of three types of foot orthoses in individuals with posterior tibial tendon dysfunction. Gait Posture. 2021;83:237-44. DOI: 10.1016/j.gaitpost.2020.11.001.
- Koltak C, Yurt Y. Comparison of the effects of low level laser and insoles on pain, functioning, and muscle strength in subjects with stage 2 posterior tibial tendon dysfunction: A randomized study. J Back Musculoskelet Rehabil. 2021;34(6):1069-78. DOI: 10.3233/BMR-200199.
- Bek N, Öznur A, Kavlak Y, Uygur F. The effect of orthotic treatment of posterior tibial tendon insufficiency on pain and disability. Pain Clinic. 2003;15(3):345-50. DOI: 10.1163/156856903767650907.
- Chao W, Wapner KL, Lee TH, Adams J, Hecht PJ. Nonoperative management of posterior tibial tendon dysfunction. Foot Ankle Int. 1996;17(12):736-41. DOI: 10.1177/107110079601701204.
- Nielsen MD, Dodson EE, Shadrick DL, Catanzariti AR, Mendicino RW, Malay DS. Nonoperative Care for the Treatment of Adult-acquired Flatfoot Deformity. J Foot Ankle Surg. 2011;50(3):311-4. DOI: 10.1053/j.jfas.2011.02.002.
- Neville C, Lemley FR. Effect of ankle-foot orthotic devices on foot kinematics in stage II posterior tibial tendon dysfunction. Foot Ankle Int. 2012;33(5):406-14. DOI: 10.3113/FAI.2012.0406.
- Neville C, Flemister AS, Houck J. Effects of the airlift PTTD brace on foot kinematics in subjects with stage II posterior tibial tendon dysfunction. J Orthop Sport Phys Ther. 2009;39(3):201-9. DOI: 10.2519/jospt.2009.2908.
- Bowring B, Chockalingam N. Conservative treatment of tibialis posterior tendon dysfunction--a review. Foot (Edinb). 2010;20(1):18-26. DOI: 10.1016/j.foot.2009.11.001.
- Harradine P, Gates L, Metcalf C, Bowen C. Podiatrists’ views and experiences of using real time clinical gait analysis in the assessment and treatment of posterior tibial tendon dysfunction. J Foot Ankle Res. 2021;14(1):42. DOI: 10.1186/s13047-021-00482-8.
- Campbell RF, Morriss-Roberts C, Durrant B, Cahill S. “I need somebody who knows about feet” a qualitative study investigating the lived experiences of conservative treatment for patients with posterior tibial tendon dysfunction. J Foot Ankle Res. 2019;12:51. DOI: 10.1186/s13047-019-0360-z.
- Stevens TT, Hartline JT, Ojo O, Grear BJ, Richardson DR, Murphy GA, et al. Race and Insurance Status Association With Receiving Orthopedic Surgeon-Prescribed Foot Orthoses. Foot Ankle Int. 2021;42(7):894-901. DOI: 10.1177/1071100721990343.
- Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3(2):77-101. DOI: 10.1191/1478088706qp063oa.
- Heller GZ, Manuguerra M, Chow R. How to analyze the Visual Analogue Scale: Myths, truths and clinical relevance. Scand J Pain. 2016;13(1):67-75. DOI: 10.1016/j.sjpain.2016.06.012.
- Bowring B, Chockalingam N. A clinical guideline for the conservative management of tibialis posterior tendon dysfunction. Foot. 2009;19(4):211-7. DOI: 10.1016/j.foot.2009.08.001.